Ear, Nose, and Throat Emergencies
Epistaxis
1. Epistaxis is a common problem in travelers.
2. Reduced humidity in airplanes, cold climates, and high-altitude environments can produce drying and erosion of the nasal mucosa.
3. Other major causes include infections, inflammatory rhinitis, inhaled medications, mucosal breakdown caused by infiltration by malignancy or granulomatous disease, and nasal trauma.
4. Daily applications of a small quantity of petroleum jelly (Vaseline) to the septum can help to keep the nasal mucosa moist.
5. Although most cases of epistaxis are minor, some present life-threatening emergencies.
6. Ninety percent of nosebleeds are anterior, and exhibit unilateral, steady, nonmassive bleeding. Ten percent are posterior and may present with massive bleeding.
7. A posterior source of the bleeding should be considered when epistaxis is bilateral, brisk, and not controlled with pinching the nostrils or with an anterior nasal pack.
Treatment
1. The existing clot should be completely cleared, usually by having the patient blow his nose.
2. One or two sprays of a topical nasal vasoconstrictor (e.g., oxymetazoline [Afrin] or phenylephrine [Neo-Synephrine]) should be inhaled into the affected nostril.
3. The patient should be kept sitting (i.e., keeping the head elevated and still).
4. The patient should be instructed to grasp and pinch his entire nose, maintaining continuous pressure against the septum for at least 15 minutes. If this maneuver does not control the bleeding, nasal packing may be required.
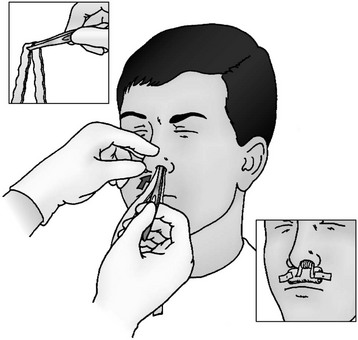
5. Anterior epistaxis nasal pack
a. Soak a piece of cotton or gauze with a vasoconstrictor such as oxymetazoline nasal spray, and insert it into the nose, leaving it in place for 5 to 10 minutes.
b. Petroleum jelly–impregnated gauze or strips of a nonadherent dressing can then be packed into the nose so that both ends of the gauze remain outside the nasal cavity (Fig. 33-1). This prevents the patient from inadvertently aspirating the nasal packing.
c. Complete packing of the nasal cavity of an adult patient requires a minimum of 1 m (3.3 ft) of packing to fill the nasal cavity and tamponade the bleeding site. When placing the gauze, it should be started as far posteriorly as is possible.
d. Expandable packing material such as Weimert Epistaxis Packing, Merocel nasal tampon, Rapid Rhino, or the Rhino Rocket is available commercially. The packing material can be lubricated with K-Y jelly or water before insertion. A tampon or balloon tip from a Foley catheter can also be used as improvised packing.
e. Anterior nasal packing blocks sinus drainage and predisposes to sinusitis. Prophylactic antibiotics (see Sinusitis, later) are recommended until the pack is removed in 48 to 72 hours.
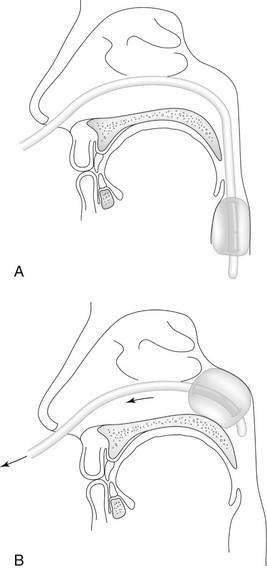
6. Posterior epistaxis nasal pack
a. If the bleeding site is located posteriorly, use a 14- to 16-French Foley catheter with a 30-mL balloon to tamponade the site (Fig. 33-2).
b. Prelubricate the catheter with either petroleum jelly (Vaseline) or a water-based lubricant.
c. Insert it through the nasal cavity into the posterior pharynx. Visualize the catheter tip in the back of the throat. Inflate the balloon with 15 mL of air or water, and gently withdraw the catheter back until resistance is met.
d. Secure the catheter firmly to the patient’s forehead with several strips of tape.
e. Avoid severe pressure on the nares.
f. Pack the anterior nose in front of the catheter balloon as described earlier.
g. Administer an antibiotic to provide prophylaxis for sinusitis (see later).
Esophageal Foreign Bodies
1. Esophageal foreign bodies may cause significant morbidity.
2. Respiratory compromise caused by tracheal compression or by aspiration of secretions can occur.
3. Mediastinitis, pleural effusion, pneumothorax, and abscess may be seen with perforations of the esophagus from sharp objects or pressure necrosis caused by large objects.
4. The use of a Foley balloon-tipped catheter passed beyond an obstruction and removed with gentle traction can be an effective method for removing a blunt esophageal foreign body. Associated complications include laryngospasm, epistaxis, pain, esophageal perforation, and tracheal aspiration of the dislodged foreign body. Uncooperative patients or sharp objects that completely obstruct the esophagus restrict the use of this technique. Use of this technique is recommended only in extreme wilderness settings or when endoscopy is not available.
a. Lubricate a 12- to 16-French Foley catheter, and place it orally into the esophagus while the patient is seated.
b. After placing the patient in the Trendelenburg position, pass the catheter beyond the foreign body and inflate the balloon with water.
c. Withdraw the catheter with steady traction until the foreign body can be removed from the hypopharynx or is expelled by coughing.
d. Take care to avoid lodging the foreign body in the nasopharynx.
e. Any significant impedance to withdrawal should terminate the attempt
Foreign Bodies in the Ear
Signs and Symptoms
1. Patient may experience significant discomfort.
2. Nausea or vomiting may occur if a live insect is in the ear canal.
3. Patient may complain of a sense of fullness in the affected ear.
4. Associated hearing loss may occur.
5. Bleeding may occur either from direct trauma or from the patient’s attempts to remove the foreign body.
6. Insects can injure the tympanic membrane or external canal.
7. Erythema and swelling of the canal or a foul-smelling discharge may develop over time.
Treatment
1. The insect should be killed before removal. Instill one of the following:
2. Irrigation is the simplest method of foreign body removal.
a. Do not irrigate if the tympanic membrane is perforated.
b. An ordinary 20- to 60-mL syringe with an irrigation tip or catheter may be used for irrigation.
3. Sometimes the object can be easily extracted with forceps.
4. Avoid pushing the object in deeper.
5. Analgesics should be given if indicated.
6. Following removal, inspect the external canal.
7. If evidence of infection or abrasion is noted, administer a combination antibiotic and steroid otic suspension (e.g., neomycin and polymyxin B and hydrocortisone otic suspension [Cortisporin], or ciprofloxacin with hydrocortisone [Cipro HC]), four to five times per day for 2 to 3 days.
Sinusitis
Signs and Symptoms
Treatment
1. Encourage hydration to promote sinus drainage.
2. Nasal vasoconstrictors (e.g., Afrin) may provide relief during initial management. These should not be used for longer than 5 days to avoid a rebound phenomenon.
3. Warm facial compresses may provide symptomatic relief.
4. Decongestants and nonsteroidal antiinflammatory drugs may be useful in reducing secretions (avoid antihistamines).
5. In severe cases, a short course of oral prednisone may be considered.
6. Analgesic medication may be necessary.
7. The organisms most commonly implicated in bacterial sinusitis are H. influenzae and Streptococcus pneumoniae (in adults).
8. A higher incidence exists of anaerobic organisms (e.g., Bacteroides, Peptostreptococcus, and Fusobacterium species are seen in chronic sinusitis).
9. Specific antibiotic treatment involves the following:
a. Amoxicillin 500 mg PO q8h for 10 to 14 days
b. Trimethoprim/sulfamethoxazole (Bactrim, Septra) 1 tab (double strength) PO q12h for 10 to 14 days
c. Amoxicillin/clavulanate (Augmentin) 500 mg PO q12h for 10 to 14 days
d. Azithromycin (Zithromax) 500 mg as a single dose on day 1, followed by 250 mg once daily on days 2 through 5
10. For worsening or severe toxicity (e.g., lethargy, vomiting, high fever), or if symptoms do not improve with antibiotics, seek urgent follow-up.