26 E-learning
What is E-learning?
Examples of e-learning include:
• independent learning using learning modules available online
• access to information and learning resources online
• web-based synchronous presentation by a teacher to a group of students
• students learning together online in real time, facilitated by a tutor
• asynchronous discussion forums or chat rooms and bulletin boards
• social networks such as Facebook
• interactive multi-media activities including games and simulations online or on a DVD
• virtual patients with whom the learner has to interact
• videos or audio recordings of lectures distributed through online streaming and podcasts using mobile devices such as telephones.
Reasons for introducing E-learning
• an emphasis on student-centred and individualised learning with ‘just-for-you’ learning, ‘just-in-time’ learning and ‘just-the-right-place’ learning
• distributed learning with students learning at different sites
• increased access to medical studies for students from different backgrounds with programmes required to cater for an increasingly diverse group of students
• advances in medicine with the problem of information overload
• the continuum of education from undergraduate through postgraduate to continuing medical education
• international dimensions and globalisation with an expansion of the traditional classroom to include students from around the world
• the changing roles of a doctor with the need to learn new skills and acquire new competencies at different times in their career
• acquisition of the skills and tools that learners need to develop in order to prosper in an information society
• high expectations of students – the ‘digital natives’ – who come to medical school with more than 10 000 hours experience in e-learning
• collaborative or peer-to-peer learning, which can be significantly facilitated by social media networking
• inter-professional education with non-threatening learning opportunities online where doctors, nurses and other members of the healthcare team can participate
• sharing of rich learning resources with potential financial benefits.
Educational features
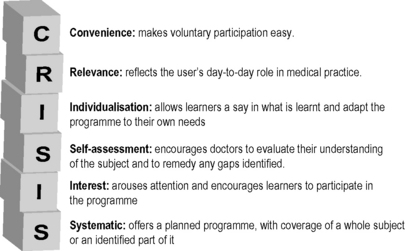
E-learning meets the criteria specified in the CRISIS framework for effective continuing education (Fig. 26.1) :
Convenience: students and trainees can learn anytime and anywhere.
Relevance: theory can be related to practice with on-the-job learning and the use of virtual patients extending the learner’s clinical experience.
Individualisation: e-learning can be designed to meet the needs of individual students in terms of their past experience and learning styles.
Self-assessment: students can be assisted to assess their own competence through questions and assessment opportunities incorporated into the e-learning activity.
Interest: e-learning can be dynamic, engaging, and user friendly if properly developed.
Systematic: an e-learning programme can systematically cover a topic and a curriculum map can be embodied that provides a framework for the student’s learning.
The role of the teacher
In e-learning the teacher is not redundant. Good collaboration is necessary between content experts, educationists and technologists. All of the roles for the teacher described in Chapter 1 are required but the emphasis in e-learning differs to some extent from what is expected in more traditional situations.
Role model
Teachers facilitating learning online serve as role models for the students and can play an important part in shaping their attitudes and professionalism. Unfortunately staff may not be the best role models with regard to the use of e-learning or how information is accessed online. Prensky (2006) has described students as the ‘digital natives’ and staff as the ‘digital immigrants’.
Assessor
Computers and information technology have an important role to play in assessment by making it possible for an assessment component to be incorporated into learning resources. Students can be encouraged to assess their achievement of the learning outcomes and to adjust if necessary their pace and path through the learning programme. Assessment should be viewed no longer as ‘assessment of learning’ but ‘assessment for learning’ and this provides a richer learning experience for the student. This concept is highlighted in Chapter 28.
Computers can be used to improve the effectiveness and efficiency of delivering traditional examinations, in scoring the student responses, and in the provision of feedback to the learner. Progress has been made with regard to online assessment for both formative and summative purposes. While the approach offers potential benefits it needs to be carefully managed to ensure that the examination runs smoothly. With summative assessment it is essential to ensure that adequate hardware and back-up systems are available. The AMEE Guide 39 covers many of the issues of online e-assessment (Dennick et al 2009).
Resource developer
The development of resources that combine appropriately the pedagogy and the technology is not an easy task. It requires a range of specialised skills that few teachers possess. A team approach is necessary involving content expert, instructional designer, educationist and technologist. Much has been written about this subject, and the 10 steps in the production of an e-learning programme are described in an AMEE guide (Harden et al 2012).
Reflect and react
1. The future is blended learning. As a teacher think what this means for you in your course and whether you have the optimum mix of face-to-face and e-learning.
2. Be aware of the range of tools available including synchronous and asynchronous online learning, podcasts and social media.
3. Consider your role in e-learning. Do you serve as a role model for your students with regard to accessing information online and using learning resources?
4. Is your aim to make your teaching more effective and efficient using e-learning or is your aim to use e-learning to benefit your students in ways not otherwise possible, for example by personalising their learning?
Cartwright C.A., Korsen N., Urbach L.E. Teaching the teachers: helping faculty in a family practice residency improve their informatics skills. Acad. Med.. 2002;77:385-391.
Dennick R., Wilkinson S., Purcell N. Online eAssessment. AMEE Guide No. 39. Med. Teach.. 2009;31:192-206.
Ellaway R., Masters K. e-Learning in Medical Education. AMEE Guide No. 32. Dundee: AMEE, 2008.
A description of how e-learning is now part of mainstream medical education.
Harden, et al. Ten steps in planning an e-learning course.. 2012. AMEE Guide. In press.
A practical guide to the production of an e-learning programme.
McKendree J. E-learning. In: Swanwick T., editor. Understanding Medical Education: Evidence, Theory and Practice. Chichester: Wiley-Blackwell; 2010:151-163. (Chapter 11).
Effective e-learning should be viewed as a curriculum design issue.
Ruiz J.G., Mintzer M.J., Leipzig R.M. The impact of e-learning in medical education. Acad. Med.. 2006;81:207-212.
A comprehensive introduction to e–learning.
Sandars J.E. M-learning. In: Dent J., Harden R.M., editors. A Practical Guide for Medical Teachers. London: Elsevier, 2011. (Chapter 32).
Clark R.C., Mayer R.E. E-learning and the Science of Instruction – Proven Guidelines for Consumers and Designers of Multimedia Learning, second ed. Chichester: Jossey Bass; 2007.
An introduction to some of the theory underpinning the use of e-learning.
Littlejohn A., Pegler C. Preparing for Blended E-learning. London: Routledge; 2007.
A description of the core skills required by teachers in blended learning.
Prensky M. Don’t Bother Me Mom – I’m Learning! How Computer and Video Games Are Preparing Your Kids For Twenty-first Century Success – and How You Can Help!. Minnesota: Paragon House, 2006. (Chapter 4)