E
Ear, nose and throat surgery (ENT surgery). Procedures vary from minor day-case surgery (e.g. myringotomy) to major head and neck dissections. Anaesthetic considerations:
– airway obstruction may be present (often worse on lying flat), particularly in adults presenting with known or suspected tumours. Flexible nasendoscopy performed in clinic can be a useful source of information regarding the patient’s upper airway anatomy. Potential difficulty with intubation/mask ventilation should be assessed.
– obstructive sleep apnoea (with features of chronic hypoxaemia) may be present.
– specific emergencies include bleeding tonsil, inhaled foreign body, epiglottitis and peritonsillar abscess.
– anxiolytic, analgesic or antisialagogue premedication may be useful depending on the clinical context and intended anaesthetic technique.
– induction appropriate to the patient’s age, co-morbidities, anticipated airway difficulty, etc.
– techniques for securing the airway in potentially difficult cases include:
– direct laryngoscopy under deep inhalational anaesthesia.
– fibreoptic intubation (awake or anaesthetised).
– tracheostomy or cricothyrotomy performed under local anaesthesia.
– options for airway maintenance:
– tracheal tube: traditionally used for most procedures, with a throat pack if bleeding or debris is anticipated. Preformed tubes are useful. Oral intubation is suitable for many procedures, including laryngectomy and tonsillectomy. Nasal intubation provides better surgical access to the oral cavity; topical local anaesthetic agents and vasopressor drugs (e.g. cocaine) are used to reduce nasal bleeding (see Nose). A small-diameter (5 mm) tube, passed orally or nasally, is usually suitable for microlaryngoscopy.
– LMA (flexible/reinforced): avoids problems associated with intubation/extubation but may impair surgical access and be more prone to displacement.
– facemask anaesthesia: suitable for minor ear operations (e.g. myringotomy/grommets).
– injector techniques: often used for bronchoscopy, laryngoscopy, tracheal surgery.
– access to the airway during surgery is restricted, therefore monitoring is particularly important. Obstruction of the airway is possible, especially during tonsillectomy if a mouth gag is used.
– N2O is usually avoided in middle ear surgery, because of expansion of gas-filled cavities.
– surgery involving the face and neck may damage the facial and laryngeal nerves respectively (see Hyperthryoidism). Absence of neuromuscular blockade may be requested by the surgeon in order to allow identification of nerves by electrical stimulation. Spontaneous ventilation, or IPPV using opioids (e.g. remifentanil), a volatile agent and induced hypocapnia, may be employed.
– thoracotomy is occasionally required, e.g. mobilisation of the stomach for anastomosis.
– laser surgery is common, especially for laryngeal surgery.
– adrenaline solutions are often used by the surgeon.
– tracheal extubation is performed with the patient deeply anaesthetised or awake (but not in between, because of the risk of laryngospasm) and in the head-down, lateral position to reduce airway soiling.
 postoperatively: as for any surgery. Major procedures may require ICU/IPPV postoperatively.
postoperatively: as for any surgery. Major procedures may require ICU/IPPV postoperatively.
See also, Intubation, difficult; Mandibular nerve blocks; Maxillary nerve blocks
Early warning scores. Simple scoring systems used to aid identification of critically ill patients or those at risk of further clinical deterioration. Several different systems have been described, employing different groups of physiological parameters (e.g. systolic BP, heart rate, respiratory rate, temperature, neurological status and urine output) that are weighted on the basis of their deviation from a ‘normal’ range. Early warning schemes may be used to ‘trigger’ calls for assistance from the patient’s primary team, a medical emergency team, an outreach team or others. In the UK, the modified early warning score is most commonly used.
Cuthbertson BH, Smith GB (2007). Br J Anaesth; 98: 704–6
See also, Acute life-threatening events – recognition and treatment
East–Freeman automatic vent, see Ventilators
Eaton–Lambert syndrome, see Myasthenic syndrome
 right heart failure and cyanosis (due to right-to-left shunting).
right heart failure and cyanosis (due to right-to-left shunting).
 tricuspid valve regurgitation.
tricuspid valve regurgitation.
 ASD is often present.
ASD is often present.
May lead to arrhythmias, conduction defects (especially the Wolff–Parkinson–White syndrome) and sudden death. Surgery may be indicated in severe cases.
[Wilhelm Ebstein (1836–1912), German physician]
ECF, see Extracellular fluid
ECG, see Electrocardiography
Echocardiography. Cardiac imaging using reflection of ultrasound pulses from interfaces between tissue planes. A single beam may be studied as it passes through the heart, displaying movement of tissue planes over time, usually recorded on moving paper (M mode). Alternatively, beams are directed in different directions from the same point, covering a sector of tissue; a moving cross-section may then be displayed on a screen. Analysis of the frequencies of reflected pulses may provide information about the velocity of moving structures and blood flow (Doppler effect); flow characteristics may be colour-coded and superimposed on sector images. The passage of injected saline may be studied as it travels through the heart, probably due to entrainment of small air bubbles.
Useful in diagnosing and quantifying valvular heart disease, congenital heart disease, patent foramen ovale, myocardial and pericardial disease, and in assessing myocardial function. Techniques for the latter involve measurement of left ventricular dimensions and provide information about ejection fraction and cardiac output. Doppler techniques may be used to estimate pressure gradients across valves, as the gradient is related to the difference in velocities across the stenosis. Abnormalities of ventricular wall movement may occur in the early stages of myocardial ischaemia, before ECG changes occur.
Transoesophageal echocardiography gives a good view of much of the heart, and has been used perioperatively and in ICU.
Eclampsia. Convulsions caused by hypertensive disease of pregnancy (pre-eclampsia).
 complications of pre-eclampsia, especially coagulopathy.
complications of pre-eclampsia, especially coagulopathy.
 cerebral oedema/haemorrhage, coma, death.
cerebral oedema/haemorrhage, coma, death.
 aspiration of gastric contents, cardiac failure, pulmonary oedema.
aspiration of gastric contents, cardiac failure, pulmonary oedema.
Incidence is 2–3 cases per 10 000 births in the UK. Occurs antepartum in 45% of cases, intrapartum in 20% and postpartum in 35% (usually under 2–4 days postpartum but eclampsia has been reported up to 2–3 weeks afterwards). Only 40% of cases have hypertension and proteinuria in the preceding week, and in many cases premonitory signs of headache, photophobia and hyperreflexia do not precede convulsions, which may recur if untreated. Mortality is almost 2% in the UK, usually from CVA; perinatal mortality is 5–6%. Maternal mortality is up to 25% mortality in developing countries.
 anticonvulsant drugs; magnesium sulphate is the drug of choice for treating eclamptic seizures, superseding diazepam and phenytoin that were traditionally used in the UK; it reduces the incidence of recurrent convulsions and of fetal/maternal complications. Thiopental is suitable in resistant cases; tracheal intubation is required.
anticonvulsant drugs; magnesium sulphate is the drug of choice for treating eclamptic seizures, superseding diazepam and phenytoin that were traditionally used in the UK; it reduces the incidence of recurrent convulsions and of fetal/maternal complications. Thiopental is suitable in resistant cases; tracheal intubation is required.
 head-down, left lateral position, if the trachea is unprotected.
head-down, left lateral position, if the trachea is unprotected.
Ecothiopate iodide. Organophosphorus compound, used as eye drops to treat severe glaucoma. Plasma cholinesterase levels may be reduced for 3–4 weeks following its use, prolonging the action of suxamethonium.
Ectopic beats, see Atrial ectopic beats; Junctional arrhythmias; Ventricular ectopic beats
ED50, see Therapeutic ratio/index
Edetate, see Cyanide poisoning; Sodium calcium edetate
Edrophonium chloride. Acetylcholinesterase inhibitor, used to reverse non-depolarising neuromuscular blockade, and in the diagnosis of myasthenia gravis and dual block. Has also been used to treat SVT. Binds reversibly to acetylcholinesterase, with onset of action 30 s and duration of about 5 min. Of faster onset than neostigmine, and with fewer muscarinic side effects.
• Dosage:
 reversal of neuromuscular blockade: 0.5–0.7 mg/kg iv with atropine.
reversal of neuromuscular blockade: 0.5–0.7 mg/kg iv with atropine.
 differentiation between myasthenic and cholinergic crises: 2 mg iv, 1 h after the last dose of cholinergic drug. Increased muscle strength occurs in myasthenic crisis; worsening of weakness in cholinergic crisis.
differentiation between myasthenic and cholinergic crises: 2 mg iv, 1 h after the last dose of cholinergic drug. Increased muscle strength occurs in myasthenic crisis; worsening of weakness in cholinergic crisis.
 diagnosis of dual block: 10 mg iv; causes transient improvement in muscle power.
diagnosis of dual block: 10 mg iv; causes transient improvement in muscle power.
• Side effects: bradycardia, hypotension, nausea, vomiting, diarrhoea, abdominal cramps, increased salivation, muscle fasciculation. Convulsions and bronchospasm may also occur. The ECG should always be monitored when edrophonium is administered, and atropine must always be available.
Efficacy. Maximal effect attainable by a drug; e.g. morphine is more efficacious than codeine. A pure antagonist has an efficacy of zero.
Eicosanoids. Collective term used for products of arachidonic acid metabolism involved in inflammation, immunity and cell signalling. Include:
 prostanoids: produced by the cyclo-oxygenase pathway, i.e. prostaglandins, prostacyclin and thromboxanes.
prostanoids: produced by the cyclo-oxygenase pathway, i.e. prostaglandins, prostacyclin and thromboxanes.
 leukotrienes produced by the lipoxygenase pathways.
leukotrienes produced by the lipoxygenase pathways.
Eisenmenger’s syndrome. Right-to-left cardiac shunt developing after long-standing left-to-right shunt; shunt reversal occurs because increased pulmonary blood flow results in increased pulmonary vascular resistance and pulmonary hypertension. Prognosis is poor, since pulmonary hypertension is not affected by surgical correction of the shunt. May follow any left-to-right shunt, although the original description referred to VSD. May occur late in ASD and patent ductus arteriosus.
 dyspnoea, effort syncope, angina, haemoptysis.
dyspnoea, effort syncope, angina, haemoptysis.
 supraventricular arrhythmias, right ventricular failure, features of pulmonary hypertension.
supraventricular arrhythmias, right ventricular failure, features of pulmonary hypertension.
Anaesthesia is tolerated poorly; reduction in peripheral resistance increases the shunt with worsening hypoxaemia, that in turn further increases pulmonary vascular resistance. Factors that decrease pulmonary blood flow also exacerbate the right-to-left shunt, e.g. IPPV. Risk of systemic air embolism following iv injection of bubbles is high.
Pregnancy is also tolerated badly; maternal mortality is 30–50%. Very cautious epidural anaesthesia has been suggested if pregnancy progresses to term.
Heart–lung transplantation is the only definitive treatment.
Ejection fraction. Left ventricular stroke volume as a fraction of end-diastolic volume.
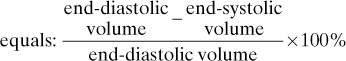
Useful as an indication of the heart’s ability to eject stroke volume. Measured using nuclear cardiology, echocardiography, pulmonary artery catheterisation or contrast angiography. Normally greater than 60%. May also be determined for the right ventricle.
Ejector flowmeter. Device used for scavenging from anaesthetic breathing systems. O2 or air passing through the ejector causes entrainment of waste gases by the Venturi principle. The rate of removal is adjusted using a flowmeter until it equals the rate of fresh gas supply. Several litres of driving gas may be required per minute, at a pressure of at least 1 bar.
EKG, see Electrocardiography
Elastance. Reciprocal of compliance. Total elastance for lungs + chest wall is approximately 10 cmH2O/l.
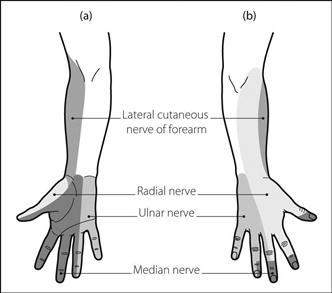
Elbow, nerve blocks. Used for surgery to the hand and wrist; useful for supplementation of a brachial plexus block. May be performed using surface anatomy landmarks, a peripheral nerve stimulator and/or ultrasound guidance.
• The following nerves are blocked (Fig. 57):
 median (C5–T1): lies immediately medial to the brachial artery in the antecubital fossa. A needle is inserted with the elbow extended, level with the epicondyles, to approximately 5 mm, and 5 ml local anaesthetic agent injected. Subcutaneous infiltration blocks cutaneous branches.
median (C5–T1): lies immediately medial to the brachial artery in the antecubital fossa. A needle is inserted with the elbow extended, level with the epicondyles, to approximately 5 mm, and 5 ml local anaesthetic agent injected. Subcutaneous infiltration blocks cutaneous branches.
 radial (C5–T1): lies in the antecubital fossa in the groove between biceps tendon medially and brachioradialis muscle laterally. A needle is inserted level with the epicondyles with the elbow extended, and directed proximally and laterally to contact the lateral epicondyle. 2–4 ml solution is injected, and a further 5 ml during withdrawal to skin. This is repeated with the needle directed more proximally.
radial (C5–T1): lies in the antecubital fossa in the groove between biceps tendon medially and brachioradialis muscle laterally. A needle is inserted level with the epicondyles with the elbow extended, and directed proximally and laterally to contact the lateral epicondyle. 2–4 ml solution is injected, and a further 5 ml during withdrawal to skin. This is repeated with the needle directed more proximally.
 lateral cutaneous nerve of the forearm (C5–7): lies alongside the radial nerve. It is a continuation of the musculoskeletal nerve of the brachial plexus. May be blocked by subcutaneous infiltration between biceps and brachioradialis, using the same puncture site as for the radial nerve.
lateral cutaneous nerve of the forearm (C5–7): lies alongside the radial nerve. It is a continuation of the musculoskeletal nerve of the brachial plexus. May be blocked by subcutaneous infiltration between biceps and brachioradialis, using the same puncture site as for the radial nerve.
 ulnar (C6–T1): passes through the ulnar groove behind the medial humeral epicondyle. With the elbow flexed to 90°, a fine needle is inserted 1–2 cm proximal to the groove, pointing distally. At 1–2 cm depth, 2–5 ml solution is injected. Neuritis may follow injection into the nerve, or block within the ulnar groove.
ulnar (C6–T1): passes through the ulnar groove behind the medial humeral epicondyle. With the elbow flexed to 90°, a fine needle is inserted 1–2 cm proximal to the groove, pointing distally. At 1–2 cm depth, 2–5 ml solution is injected. Neuritis may follow injection into the nerve, or block within the ulnar groove.
Elderly, anaesthesia for. Increasingly common as the population ages. Mortality and morbidity are higher in older patients.
• Anaesthetic considerations, compared with younger patients:
– ischaemic heart disease is more likely, with reduced ventricular compliance and contractility, and cardiac output.
– decreased blood flow to vital organs.
– cerebrovascular insufficiency is common.
– widespread atherosclerosis with a less compliant arterial system. Hypertension is common.
– veins are more tortuous, thickened and fragile.
– DVT is more common.
– decreased lung compliance and alveolar surface area.
– increased closing capacity, therefore more airway collapse with resultant increase in alveolar–arterial O2 difference. Normal alveolar PO2 is approximately:
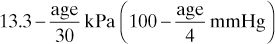
– decreased response to hypercapnia and hypoxaemia.
– higher incidence of postoperative atelectasis, PE and chest infection.
– increased sensitivity to many drugs, especially CNS depressants.
– half-lives of many drugs are increased.
– fluid balance is more critical with reduction in total body water; dehydration is common following trauma and illness.
– diabetes mellitus and malnutrition are more common.
– cerebrovascular disease is common.
– confusion and postoperative cognitive dysfunction are more likely, and may be caused by hypoxia, hyperventilation, drugs, hospitalisation and any illness.
– autonomic nervous system dysfunction is common.
– impaired hearing, vision and memory loss are common.
– heat loss during anaesthesia is more likely due to impairment of both central control and compensatory mechanisms.
– hiatus hernia is more common, with risk of regurgitation and aspiration.
– systemic diseases and multiple drug therapy are more common.
In general, patients are frailer, with greater likelihood of perioperative complications and slower healing. Attention to detail (e.g. fluid balance) is more important than with younger patients, since physiological reserves are less. Smaller doses of most agents are required, and arm–brain circulation time is prolonged.
Warming blankets, adequate humidification and appropriate monitoring (e.g. of urine output) should be provided. Postoperative O2 therapy should be instituted immediately and possibly continued for 1–3 days, since hypoxia may readily occur.
Electrical symbols. Used to denote components of electrical circuits. Specific symbols are also used on electrical equipment to indicate the safety features or other characteristics or instructions (Fig. 58).
See also, Electrocution and electrical burns
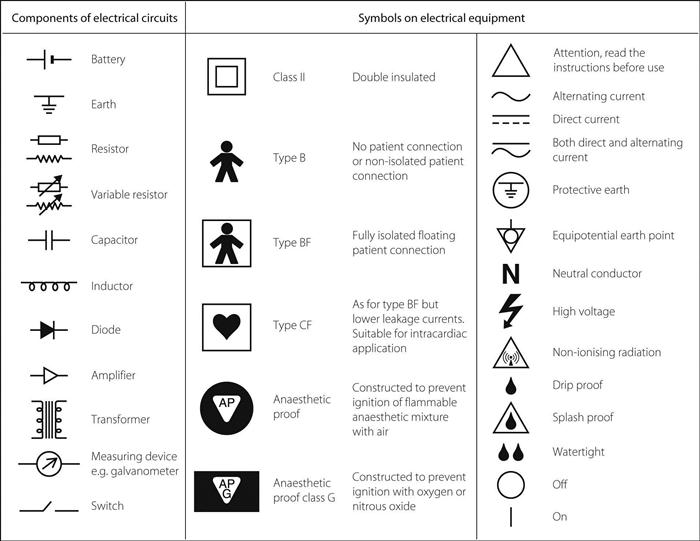
Fig. 58 Electrical symbols
Electroacupuncture, see Acupuncture
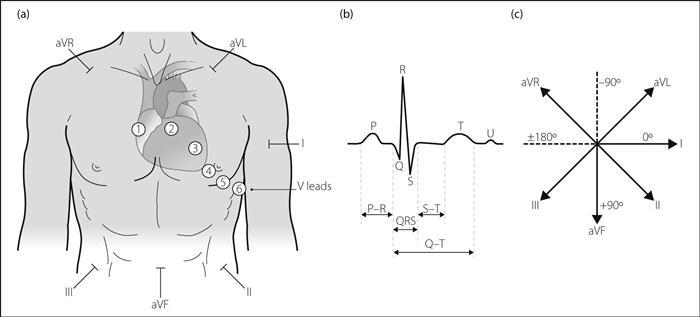
Electrocardiography (ECG). Recording and display of cardiac electrical activity. First performed through the intact chest in 1887 by Waller. Used for investigation of cardiac disease, particularly ischaemic heart disease and arrhythmias, also for monitoring cardiac rhythm.
Standard modern ECG recordings are obtained from different combinations of chest and limb electrodes, each set recording along a different vector, thus providing information about a different part of the heart. A ‘lead’ refers to the recorded voltage difference between two electrodes; one acts as the positive electrode, the other as the negative (or reference) electrode. The limb leads (I–III, aVR, aVL, aVF) record in the frontal plane, the chest leads (V1–6) in the transverse plane. The leads may be represented on the chest and heart as in Figure 59a. Thus abnormalities of the inferior portion of the heart will be demonstrated in the ‘inferior’ leads (i.e. aVF, II and III), and abnormalities of the anterolateral heart in aVL, I, II, etc. V1–2 demonstrate electrical activity from the right side of the heart, V3–4 from the septum and front, and V5–6 from the left side. Depolarisation towards a positive electrode (or repolarisation away) results in a positive deflection; depolarisation away (or repolarisation towards) causes negative deflection.
– I: between left arm (positive electrode) and right arm (negative).
– II: between left leg (positive electrode) and right arm (negative).
– III: between left leg (positive electrode) and left arm.
– V1: fourth intercostal space, right sternal edge.
– V2: fourth intercostal space, left sternal edge.
– V3: midway between V2 and V4.
– V4: fifth intercostal space, left midclavicular line.
Output is displayed on an oscilloscope or recorded on moving paper. Frequency range is 0.5–80 Hz. Magnitude of deflection is proportional to the amount of heart muscle, but reduced by passage through the chest. Skin resistance is reduced by cleaning with alcohol and skin abrasion. Electrodes are usually silver/silver chloride with chloride conducting gel, to reduce generation of potentials in the electrode by the recorded potential, and reduce impedance variability. Electrodes of differing compounds may generate potential by a battery-like effect. Interference may result from muscle activity, radiofrequency waves from diathermy and other equipment and inductance by electrical equipment. Differential amplifiers with common-mode rejection (elimination of signals affecting both input terminals of a recording system) are used to reduce interference.
• Plan for the interpretation of standard ECG, with normal values (Fig. 59b):
 patient’s name, clinical context, date.
patient’s name, clinical context, date.
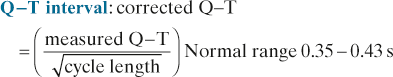
 rate: heart rate in beats/min is calculated by dividing the number of 5 mm squares between successive QRS complexes into 300, assuming a recording speed of 25 mm/s.
rate: heart rate in beats/min is calculated by dividing the number of 5 mm squares between successive QRS complexes into 300, assuming a recording speed of 25 mm/s.
– regular or irregular. An irregular rhythm may be regularly (e.g. missing every third QRS) or irregularly irregular (e.g. completely random in AF).
– presence/absence of P waves, flutter waves in atrial flutter, ventricular ectopic beats, pacing spikes, etc.
 axis: summation of electrical potentials from the standard and aV leads, plotted as vectors. The normal axis lies between –30° and +90° (Fig. 59c).
axis: summation of electrical potentials from the standard and aV leads, plotted as vectors. The normal axis lies between –30° and +90° (Fig. 59c).
Left axis deviation (< −30°) may occur in:
– normal subjects (especially if pregnant), ascites, etc.
– left bundle branch block, left anterior hemiblock.
– left ventricular hypertrophy.
Right axis deviation (> 90°) may occur in:
– right ventricular hypertrophy.
– right bundle branch block, left posterior hemiblock.
 P wave (atrial depolarisation):
P wave (atrial depolarisation):
– positive in I, II, and V4–6; negative in aVR, since depolarisation moves downwards and to the left.
– shape.
 P–R interval: normally 0.12–0.2 s (3–5 mm squares).
P–R interval: normally 0.12–0.2 s (3–5 mm squares).
 QRS complex (ventricular depolarisation):
QRS complex (ventricular depolarisation):
– duration is 0.04–0.12 s (1–3 mm squares).
– amplitude in I + II + III > 5 mm. Left ventricular hypertrophy exists if the R wave in V6 + S wave in V1 > 35 mm. In right ventricular hypertrophy the R : S ratio > 1 in V1–2.
– abnormal waves, e.g. J and δ waves in hypothermia and Wolff–Parkinson–White syndrome respectively.
– level within 1 mm of baseline.
– shape.
 T wave (ventricular repolarisation):
T wave (ventricular repolarisation):
– orientation as for QRS complexes.
– shape.
During anaesthesia/intensive care, a three-electrode system (allowing recording of the three standard limb leads) is often used and lead II is selected for continuous rhythm monitoring. A five-electrode system incorporating a right leg and precordial electrode (in addition to the right arm/left arm/left leg electrodes) enables recording of an anterior chest lead; useful when monitoring left ventricular myocardial ischaemia. The CM5 lead configuration (central manubrium V5) also ‘looks at’ the left ventricle:
 right arm electrode in suprasternal notch.
right arm electrode in suprasternal notch.
 left arm electrode over apex of heart (V5 position).
left arm electrode over apex of heart (V5 position).
 left leg electrode on left shoulder or leg serves as ground.
left leg electrode on left shoulder or leg serves as ground.
See also, Cardiac cycle; Heart block: His bundle electrography; Myocardial infarction
– concurrent drug therapy may include antidepressant drugs, including monoamine oxidase inhibitors, lithium.
– premedication is usually omitted.
– monitoring is required as for any procedure.
– a single induction dose of iv agent is usually given. Methohexital was traditionally used because of its short action and pro-convulsant properties. Propofol (at 1 mg/kg) provides greater haemodynamic stability and more rapid post-ictal recovery whilst having the same therapeutic benefit as methohexital and has become the induction agent of choice.
– suxamethonium 0.5 mg/kg is commonly given, although smaller doses have been used.
– a soft mouth guard is inserted to protect the teeth and gums.
– intense parasympathetic discharge may follow passage of current, and may be followed by increased sympathetic activity. Atropine should always be available; routine administration has been suggested.
Electrocution and electrical burns. Hazard of using electrical equipment; during anaesthesia, malfunction or improper use of diathermy, monitoring equipment or infusion devices may cause sudden cardiac arrest or burns.
• Effects:
 heat production due to high resistance of tissues. Amount of heat is related to current density. May produce burns at sites of current entry/departure.
heat production due to high resistance of tissues. Amount of heat is related to current density. May produce burns at sites of current entry/departure.
 nerve and muscle stimulation; e.g. effect of current across chest (approximate values):
nerve and muscle stimulation; e.g. effect of current across chest (approximate values):
– 15 mA: tonic muscle contraction, i.e. ‘can’t let go’ threshold.
– > 5 A: tonic contraction of the myocardium (utilised in defibrillation).
– frequency of alternating current: 50–60 Hz is particularly dangerous but cheap to provide.
– timing of shock (e.g. R on T phenomenon).
 regular checking and maintenance of electrical equipment.
regular checking and maintenance of electrical equipment.
 use of batteries only (impractical).
use of batteries only (impractical).
 double insulation of all conducting wires within equipment (class II).
double insulation of all conducting wires within equipment (class II).
 reduction of stray leakage currents, e.g. due to drops in potential along the length of conductors, caused by capacitance between casing and innards or inductance. Leakage currents may be sufficient to produce microshock. Earth conductors are connected to each other to reduce differences between them. Current-operated earth-leakage circuit breakers may be used. Standards for leakage currents are defined, e.g. 10 µA maximum from the casing or delivered to the patient for intracardiac equipment; 100–500 µA for other equipment, depending on usage.
reduction of stray leakage currents, e.g. due to drops in potential along the length of conductors, caused by capacitance between casing and innards or inductance. Leakage currents may be sufficient to produce microshock. Earth conductors are connected to each other to reduce differences between them. Current-operated earth-leakage circuit breakers may be used. Standards for leakage currents are defined, e.g. 10 µA maximum from the casing or delivered to the patient for intracardiac equipment; 100–500 µA for other equipment, depending on usage.
Medical electrical equipment is marked with the appropriate electrical symbols to indicate its level of safety features (see Fig. 58).
 beta: normal 13–30 Hz waves. Prominent over the frontal area during the awake and active state.
beta: normal 13–30 Hz waves. Prominent over the frontal area during the awake and active state.
As age increases, infantile beta activity is slowly replaced by adult alpha activity. Characteristic patterns occur in normal sleep. During anaesthesia, alpha rhythms become depressed, and are replaced by theta and delta rhythms. Slow rhythms may reappear at deeper levels of anaesthesia, followed by periods of little or no activity separated by bursts of activity (burst suppression). The pattern differs with different agents used. Perioperative use is limited by electrical interference, difficult interpretation and production of large amounts of paper. Modified forms of EEG have therefore been developed, e.g. cerebral function monitor, cerebral function analysing monitor, power spectral analysis, bispectral index monitor. Used to investigate intracranial activity in, e.g., head injury, epilepsy, cerebrovascular disease, coma, encephalopathies, surgery. Similar principles are involved in measuring evoked potentials.
Electrolyte. Compound that dissociates in solution to produce ions, allowing conduction of electricity; also refers to the ions themselves. Sodium, potassium, calcium, magnesium and hydrogen ions are the most important cations in the body; chloride and bicarbonate ions the most important anions.
Electrolyte imbalance, see individual disorders
Electrolyte solutions, see Intravenous fluids
Electromechanical dissociation (EMD). Term used to describe a cardiac state in which organised electrical depolarisation occurs throughout the myocardium, but there is no synchronous shortening of the myocardial fibres and mechanical contractions are absent. Part of the spectrum of pulseless electrical activity, though the latter also includes mechanical contractions too weak to produce a detectable cardiac output.
Electromyography (EMG). Recording of spontaneous or evoked electrical activity from skeletal muscle; usually combined with nerve conduction studies that measure the velocity of nerve conduction following stimulation at different sites along a nerve pathway. Thus useful in distinguishing between disorders of muscle, isolated or generalised nerve disease or lesions, and disorders affecting the neuromuscular junction.
In anaesthesia, it has been used to determine frontalis muscle tone to monitor depth of anaesthesia. Also used in neuromuscular blockade monitoring; nerve stimulation and muscle action potential recording are achieved using surface skin electrodes, although needle electrodes have been used. Less convenient than devices measuring mechanical muscle response, it may detect electrical activity when mechanical contraction is undetectable.
Is also used to investigate critical illness polyneuropathy and the neuromuscular function of the eye, bladder, GIT, etc.
Electron capture detector. Device used in the analysis of gas mixtures that have been separated by, for example, gas chromatography; particularly useful in detecting halogenated compounds. Electrons within an ionisation chamber pass from cathode to anode, but are ‘captured’ by the halogenated substance blown through the chamber. The current passing across the chamber is therefore reduced, depending on how many electrons are captured. Used to quantify the amount of known substances, not to identify unknown ones.
Emergence phenomena. Usually consist of agitation and confusion, with laryngospasm, breath-holding, etc.; may be equivalent to the second stage of anaesthesia seen on induction, or be due to other causes of confusion, including the central anticholinergic syndrome and dystonic reactions. Hallucinations and frightening dreams are common after ketamine.
 inadequate preparation of patients for surgery:
inadequate preparation of patients for surgery:
 full stomach, i.e. risk of aspiration of gastric contents.
full stomach, i.e. risk of aspiration of gastric contents.
 untreated pre-existing disease, electrolyte imbalance, etc.
untreated pre-existing disease, electrolyte imbalance, etc.
 appropriate investigations and cross-matching of blood not performed or not ready.
appropriate investigations and cross-matching of blood not performed or not ready.
– haemorrhage and hypovolaemia.
– intestinal obstruction/intra-abdominal pathology: dehydration and hypovolaemia, electrolyte imbalance, etc. Further risk of aspiration due to delayed gastric emptying and vomiting/haematemesis.
– trauma: haemorrhage, head injury, chest trauma, etc.
– airway obstruction/inhaled foreign body.
– related to specialist surgery, e.g. cardiac surgery, neurosurgery.
The balance between the need for preoperative treatment and urgency of surgery is sometimes difficult, but inadequate preoperative correction of fluid and electrolyte disturbance is consistently associated with increased perioperative mortality. Treatment of cardiac failure is also important whenever possible. Careful preoperative assessment and discussion with the surgeon are vital. Anaesthetic management is as for routine surgery but with the above considerations. Thus smaller doses of drugs than usual are given initially. Rapid sequence induction is usually employed. Measures against heat loss are important. Invasive monitoring and postoperative HDU/ICU and IPPV should be considered.
Regional techniques are particularly useful for limb surgery, but epidural/spinal anaesthesia is hazardous if hypovolaemia is present.
Special Issue (2013). Anaesthesia; 68 s1: 1–124
See also, specific procedures; Anaesthetic morbidity and mortality
Emetic drugs. Given to empty the stomach, e.g. following poisoning, or preoperatively to reduce risk of aspiration pneumonitis. Now rarely used, because of poor efficacy and the risk of causing aspiration; particularly dangerous after ingestion of corrosive or petroleum derivatives, or in unconscious patients. Include apomorphine and ipecacuanha; copper sulphate and sodium chloride are no longer used.
EMG, see Electromyography
EMLA cream (Eutectic mixture of local anaesthetics). Mixture of prilocaine base 2.5% and lidocaine base 2.5% as an oil–water emulsion. The melting point of each local anaesthetic agent is lowered by the presence of the other; the resultant mixture has a melting point of 18°C and is effective in providing analgesia of the skin 60–90 min after topical application and covering with an occlusive dressing. May continue to be released from skin depots even after removal of surface cream. Particularly useful in children. May produce blanching of the skin; increases in methaemoglobin have been reported several hours after application.
EMO inhaler, see Vaporisers
Emphysema, see Chronic obstructive pulmonary disease
Emphysema, subcutaneous. Presence of gas in subcutaneous tissues.
 pneumothorax or rupture of a viscus, e.g. oesophagus.
pneumothorax or rupture of a viscus, e.g. oesophagus.
 infection with gas-producing organisms, e.g. gas gangrene.
infection with gas-producing organisms, e.g. gas gangrene.
 rarely, deliberate self-injection of subcutaneous air in disordered mental states.
rarely, deliberate self-injection of subcutaneous air in disordered mental states.
Empyema. Collection of pus within the pleural cavity. A complication of chest trauma (especially if haemothorax was present), pneumonia, chest drainage, thoracic surgery and subdiaphragmatic abscess. Clinical features include pyrexia, chest pain and productive cough. CXR features are those of a pleural effusion; if encapsulated it may resemble a pulmonary cyst. Diagnosis is confirmed by imaging and aspiration of pus. Treatment depends on aetiology but includes antibacterial drugs, chest drainage (sometimes requiring ultrasound or CT scan guidance) and surgery. May rarely lead to bronchopleural fistula.
Enalapril maleate. Angiotensin converting enzyme inhibitor, used to treat hypertension and cardiac failure (including following MI). A prodrug, it is converted to enalaprilat by hepatic metabolism. Longer acting than captopril, with onset of action within 2 h; half-life is up to 35 h via active metabolites.
Encephalitis. Acute infection of the brain parenchyma, usually caused by a virus, that results in diffuse inflammation affecting the meninges. Usually presents with the triad of fever, headache and altered mental status. Other clinical features include neck stiffness, lethargy, confusion, coma, encephalopathy, focal neurological signs and epilepsy.
• Causes:
 autoimmune encephalitis (including anti-NMDA receptor encephalitis and anti-voltage-gated potassium channel encephalitis) is being increasingly recognised; presents with psychiatric, epileptic and movement disorder features.
autoimmune encephalitis (including anti-NMDA receptor encephalitis and anti-voltage-gated potassium channel encephalitis) is being increasingly recognised; presents with psychiatric, epileptic and movement disorder features.
Differential diagnosis includes meningitis and cerebral abscess. Investigations include CSF examination (mild increase in protein, lymphocytosis, normal glucose in viral encephalitis), CT and MRI scanning, EEG and viral titres/cultures from blood and CSF. Treatment is largely supportive, with tracheal intubation and IPPV for patients with depressed consciousness. Aciclovir should be given to all cases of suspected viral encephalitis whilst a definitive diagnosis is sought.
Encephalopathy. Diffuse disorder of cerebral function with or without focal neurological deficit. Usually results in delirium, stupor and coma. Aetiology is as for coma.
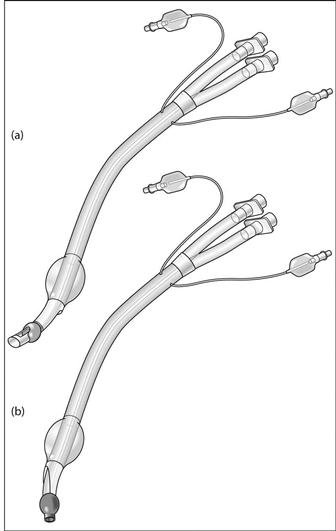
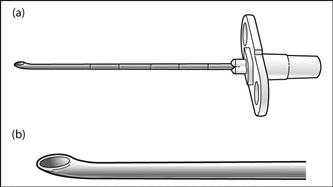
Endobronchial blockers (Bronchial blockers). Used in thoracic surgery to isolate a portion of lung, e.g. to avoid air leaks during IPPV or prevent contamination of normal lung with secretions, pus or blood. Less often used now, except for paediatric surgery, endobronchial tubes being more popular and versatile. Previous versions were made of red rubber; modern versions are thin plastic catheters with an inflatable distal cuff, usually inserted under direct vision via a bronchoscope, either before tracheal intubation with a standard tracheal tube or after intubation with a specific tube–blocker combination.
Endobronchial tubes. Used in thoracic surgery to allow sleeve resection of the bronchus, or to isolate infected lung or potential air leak, e.g. in bronchopleural fistula or emphysematous lung cysts. Other pulmonary surgery (e.g. pneumonectomy/lobectomy, pleural, aortic, oesophageal and mediastinal surgery) is possible with conventional tracheal tubes, although surgery may be made easier by collapsing one lung. Also used in ICU in patients with severe, unilateral lung injury or bronchopleural fistula. Risks of one-lung anaesthesia should be considered before use.
Different tubes, usually made of red rubber, were developed in the 1930s–1950s, and included single-lumen and double-lumen designs, for insertion into the left (most commonly) or right main bronchus. Modern double-lumen tubes are usually plastic, with thinner walls and low-pressure cuffs, and have the following features (Fig. 60):
 oropharyngeal portion, concave anteriorly.
oropharyngeal portion, concave anteriorly.
– the catheter mount to the tracheal lumen is clamped, and the tracheal lumen opened to air.
– the tracheal lumen is reconnected and both sides of the chest are checked as before.
Complications are as for tracheal intubation (see Intubation, complications of). Bronchial rupture may occur if excessive volumes are used for cuff inflation. Incorrect positioning, or movement during positioning of the patient, may result in uneven ventilation and impaired gas exchange.
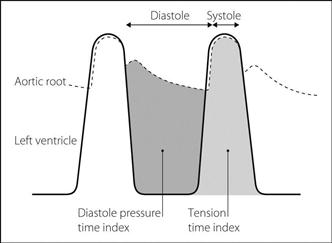
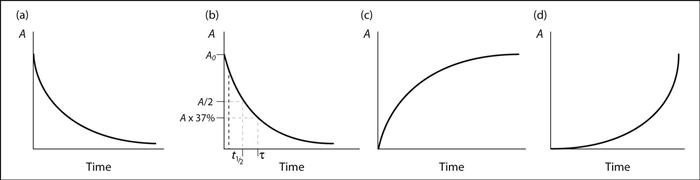
Endocardial viability ratio (EVR). Ratio of diastolic pressure time index to tension time index, obtained by recording left ventricular and aortic root pressure tracings (Fig. 61). May indicate myocardial O2 supply/demand ratio and likelihood of myocardial ischaemia (thought to be likely when the ratio is under 0.7).
Endocarditis, infective. Infective inflammation of the endocardial lining of the heart and valves, most commonly the aortic valve (previously the mitral valve). Commonly associated with abnormal valves (e.g. rheumatic, degenerative or prosthetic valves) or congenital heart disease, but approximately 50% of cases involve normal valves. Men are twice as commonly affected. Nosocomial endocarditis may result from catheter-related sepsis or invasive procedures (e.g. endoscopy, dental extractions). Results in tissue destruction and vegetations of platelets, macrophages and organisms, with systemic embolisation. Systemic immune complex deposition may also occur. Overall mortality is ~40%.
• Traditionally divided into acute and subacute, although definitions are imprecise:
– usually due to virulent organisms, e.g. Streptococcus pneumoniae, Staphylococcus aureus.
– presents early with rapid progression to death unless early aggressive treatment is instituted.
– usually due to Streptococcus viridans or enterococci.
– underlying structural heart disease or presence of prosthetic valves is usual.
– chronic malaise and slow course of disease are typical.
 fever (90%), malaise, weight loss, night sweats, anaemia.
fever (90%), malaise, weight loss, night sweats, anaemia.
 heart murmurs (85%), cardiac failure, valve lesions.
heart murmurs (85%), cardiac failure, valve lesions.
 peripheral embolisation/vasculitic phenomena, e.g. splinter haemorrhages in nail beds, conjunctivae and retina (Roth spots), painful fingertip swellings (Osler’s nodes), painless haemorrhagic lesions on palms and soles (Janeway lesions), kidneys (causing haematuria), CNS (causing CVA). Splenomegaly and clubbing may occur.
peripheral embolisation/vasculitic phenomena, e.g. splinter haemorrhages in nail beds, conjunctivae and retina (Roth spots), painful fingertip swellings (Osler’s nodes), painless haemorrhagic lesions on palms and soles (Janeway lesions), kidneys (causing haematuria), CNS (causing CVA). Splenomegaly and clubbing may occur.
 echocardiography (initially transthoracic then transoesophageal if the former is negative).
echocardiography (initially transthoracic then transoesophageal if the former is negative).
European Society of Cardiology Task Force (2009). Eur Heart J; 30: 2369–413
Endocrine disorders, see individual diseases
Endomorphins. Endogenous opioid peptides for µ opioid receptors. Produce spinal and supraspinal analgesia experimentally; have been found in the human brain, although their role is uncertain.
Endorphins. Endogenous opioid peptides derived from β-lipotropin, secreted by the anterior pituitary and hypothalamus. β-Endorphin (31 amino acids) is the most potent endogenous opioid, active mainly at µ and δ opioid receptors. Also inhibits GABA and promotes dopamine secretion. Derived from pro-opiomelanocortin (99 amino acids), from which ACTH is derived. Thought to be involved in central pain pathways, emotion, etc. May also be involved in haemorrhagic and septic shock; thought to reduce SVR, cardiac output and BP, while decreasing GIT motility and sympathetic activity and enhancing parasympathetic activity. This may explain why naloxone sometimes improves cardiovascular variables in shock.
Endothelin. Vasoconstrictor peptide derived from vascular endothelium, involved in regulation of basal vascular tone and BP. Produced from an inactive precursor, it acts at specific endothelin receptors to cause vasoconstriction (type A receptors). Type B receptor activation may also result in production of nitric oxide and prostacyclin. May be involved in local blood flow and in various cardiovascular disorders, notably cardiac failure and pulmonary hypertension. Endothelin receptor antagonists such as bosentan (which antagonises both A and B receptors) have been investigated as possible treatments for these.
Endothelium-derived relaxing factor, see Nitric oxide
Endotoxins. Lipopolysaccharides (LPS) present on the surface of Gram-negative bacteria. LPS consist of: a lipid chain (lipid A), responsible for the biological effects; a core polysaccharide; and oligosaccharide side chains specific to each strain. Released when the bacteria die, and extremely toxic, probably via release and activation of many inflammatory substances, including cytokines. Endotoxaemia may be involved in the aetiology of sepsis, although it may occur in the absence of infection, and proven Gram-negative sepsis may not be accompanied by endotoxaemia. Translocation of GIT organisms or their endotoxins into the bloodstream across the gut wall has been suggested to occur in critical illness. Attempts have been made to prevent endotoxaemia by killing GIT organisms (selective decontamination of the digestive tract), and to treat established endotoxaemia with anti-endotoxin antibodies.
Wendel M, Paul R, Heller AR (2007). Intensive Care Med; 33: 25–35
Endotracheal tubes, see Tracheal tubes
End-plate potentials. Depolarisation potentials produced at the postsynaptic motor end-plate of the neuromuscular junction by binding of acetylcholine (ACh) to receptors. Their size and duration depend on the amount of ACh released, the number of ACh receptors free and the activity of acetylcholinesterase. Miniature end-plate potentials (under 1 mV) are thought to be produced by random release of ACh from single vesicles (quantal theory), and are too small to initiate muscle contraction. Simultaneous release of ACh from many vesicles follows depolarisation of the pre-synaptic membrane; the resultant large end-plate potential causes depolarisation of adjacent muscle membrane, and muscle contraction.
End-tidal gas sampling. Gives the approximate composition of alveolar gas, unless major  mismatch exists or tidal volume is very small. Useful for estimating alveolar and hence arterial PCO2, e.g. for monitoring adequacy of ventilation. Alveolar concentrations of inhalational anaesthetic agents may also be monitored. May also indicate extent and rate of uptake of inhalational agents, if expired and inspired concentrations are compared, and the state of O2 supply/demand. On-line multiple gas monitors are now routine, providing breath-by-breath measurements. Since the gas sampled by these is not strictly end-tidal, the sampling line being placed some distance away from the patient’s airway, the term ‘end-expiratory’ is more accurately applied. Mixing of end-expiratory gas with fresh gas may lead to inaccuracy, especially if samples are taken between the breathing system filter and the anaesthetic machine.
mismatch exists or tidal volume is very small. Useful for estimating alveolar and hence arterial PCO2, e.g. for monitoring adequacy of ventilation. Alveolar concentrations of inhalational anaesthetic agents may also be monitored. May also indicate extent and rate of uptake of inhalational agents, if expired and inspired concentrations are compared, and the state of O2 supply/demand. On-line multiple gas monitors are now routine, providing breath-by-breath measurements. Since the gas sampled by these is not strictly end-tidal, the sampling line being placed some distance away from the patient’s airway, the term ‘end-expiratory’ is more accurately applied. Mixing of end-expiratory gas with fresh gas may lead to inaccuracy, especially if samples are taken between the breathing system filter and the anaesthetic machine.
Energy. Capacity to perform work, whether mechanical, chemical or electrical. Kinetic energy is the energy of a body due to its motion; potential energy is the energy of a body due to its state or position. Thus a body on a table has potential energy due to the effect of gravity; when it falls, this is converted to kinetic energy. Similarly, the potential energy of a stretched spring is converted to kinetic energy as it recoils. The law of conservation of energy states that energy cannot be destroyed or created, but only converted to other forms of energy, e.g. heat, light, sound. Molecules within a body have potential energy due to their chemical composition and forces between them, and kinetic energy due to their movement. SI unit is the joule, although the Calorie (Cal; equals 1000 cal) is widely used for dietary energy estimations.
Energy is liberated in the body by breakdown of metabolic substrates, e.g. approximately 4 Cal/g carbohydrate and protein, 9 Cal/g fat, 7 Cal/g alcohol. It may be stored in high phosphate bonds, e.g. in ATP, and in other compounds, e.g. glycogen.
Energy balance. Difference between Calorie intake and energy output. If intake is less than expenditure, energy balance is negative and endogenous energy stores are utilised; if it is greater, balance is positive and the individual gains weight. Many critically ill patients (e.g. those with trauma, sepsis) have increased catabolism and glycogenolysis, insulin resistance with resultant lipolysis and increased basal metabolic rate. In order to provide adequate nutrition in these patients, it is possible to estimate energy expenditure, e.g. with indirect calorimetry using bedside devices (‘metabolic carts’). This allows measurement of O2 and CO2 exchange and thus respiratory exchange ratio; however such techniques are not widely used because of inaccuracies related to gas leaks from the patient/ventilator circuit and the effect of water vapour.
Enflurane. 2-Chloro-1,1,2-trifluoroethyl difluoromethyl ether (Fig. 62). Inhalational anaesthetic agent, introduced in 1966.
 colourless volatile liquid with ether-like smell; vapour is 7.5 times denser than air.
colourless volatile liquid with ether-like smell; vapour is 7.5 times denser than air.
 SVP at 20°C 24 kPa (175 mmHg).
SVP at 20°C 24 kPa (175 mmHg).
 MAC 1.7% (middle age); 1.9% (young adults); 2.4–2.5% in children/teenagers.
MAC 1.7% (middle age); 1.9% (young adults); 2.4–2.5% in children/teenagers.
 non-flammable and non-corrosive. Stable without additives and unaffected by light.
non-flammable and non-corrosive. Stable without additives and unaffected by light.
• Effects:
– smooth and rapid induction and recovery.
– epileptiform EEG activity may occur (typically a three per second spike and wave pattern), especially at doses > 2 MAC with coexisting hypocapnia. Convulsions may occur postoperatively.
– increased cerebral blood flow but reduced intraocular pressure.
– depresses airway reflexes less than halothane and therefore tracheal intubation is more difficult when the patient is breathing spontaneously.
– causes greater respiratory depression than halothane or isoflurane; an increased respiratory rate is common, with decreased tidal volume.
– causes fewer arrhythmias than halothane, and less sensitisation of the myocardium to catecholamines.
– dose-dependent uterine relaxation.
About 2% metabolised, the rest excreted via the lungs. Although fluoride ions may be produced by metabolism, toxic levels are usually not reached, although they have been reported in obese patients after prolonged anaesthesia. Patients with pre-existing renal impairment or receiving other nephrotoxic drugs or enzyme-inducing drugs, e.g. isoniazid, are also thought to be at risk.
Hepatitis has been reported following enflurane; cross-sensitivity with halothane has been suggested, but this is disputed.
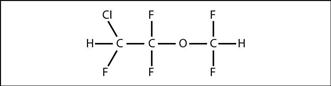
Fig. 62 Structure of enflurane
Enkephalins. Endogenous opioid peptides found in the CNS, especially:
Methionine enkephalin and leucine enkephalin (each 5 amino acids) are derived from proenkephalin; they are thought to be involved in the modulation of pain pathways, e.g. gate control theory of pain. Active mainly at δ opioid receptors.
Enoxaparin, see Heparin
Enoximone. Selective (PDE III) phosphodiesterase inhibitor unrelated to catecholamines or cardiac glycosides. Used as an inotropic drug, particularly in cardiogenic or other types of shock, in which there is an element of heart failure (e.g. after cardiac surgery, and in patients awaiting heart transplants). Increases cardiac contractility and stroke volume with minimal tachycardia, and without increasing myocardial O2 demand. Also causes vasodilatation (reducing both preload and afterload), thereby decreasing ventricular filling pressures. BP may fall.
Acts directly on cardiac muscle rather than adrenergic (or other) receptors.
Undergoes hepatic metabolism to partially active metabolites, excreted renally.
ENT surgery, see Ear, nose and throat surgery
Enteral nutrition, see Nutrition, enteral
Entonox. Trade name for gaseous N2O/O2 50 : 50 mixture, supplied in cylinders at a pressure of 137 bar. Invented by Tunstall in 1962. Cylinders are coloured blue with blue/white quartered shoulders. May also be supplied by pipeline. Formed by bubbling O2 through liquid N2O (Poynting effect).
Cylinders must be kept above –7°C (pseudocritical temperature) to prevent liquefaction of the N2O (a process called lamination). If this occurs and gas is drawn from the top of the cylinder, O2 will be delivered first, followed by almost pure N2O. In the large cylinders used for connection to a pipeline system via a manifold, gas is therefore drawn first from the bottom of the cylinder by a tube; should liquefaction of N2O now occur, N2O containing about 20% O2 is delivered first. Warming and repeated inversion of the cylinders will reconstitute the gaseous mixture.
Widely used for inhalational analgesia for trauma and minor procedures, e.g. physiotherapy or change of dressings; most commonly used with a demand valve for self-administration. Onset of analgesia is rapid, with minimal cardiovascular, respiratory or neurological side effects. Should sedation occur, the patient reduces the intake and recovery rapidly occurs. Caution is required if the patient has an undrained pneumothorax, as N2O may increase its size.
Continuous use (e.g. in ICU) has declined because of interaction of N2O with the methionine synthase system.
Envenomation, see Bites and stings
Environmental impact of anaesthesia. Has attracted increasing attention through two main areas:
Suggested measures to minimise the above include:
 increased recycling, including glass from ampoules.
increased recycling, including glass from ampoules.
 power-saving strategies, e.g. turning off equipment not in use.
power-saving strategies, e.g. turning off equipment not in use.
 avoidance of N2O, use of low-flow systems.
avoidance of N2O, use of low-flow systems.
 consideration of transportation costs when ordering equipment/drugs.
consideration of transportation costs when ordering equipment/drugs.
Sneyd JR, Montgomery H, Pencheon D (2010). Anaesthesia; 65; 435–7
Environmental safety of anaesthetists. Hazards faced may be due to:
 inhalational agents: fears were expressed, especially in the 1960s, because of reported high incidence of lymphoid tumours in anaesthetists. Chronic exposure to low concentrations of volatile agent was thought to be responsible, hence attempts to remove it from the immediate atmosphere by adsorption or scavenging. Such an association was not supported by subsequent studies, and effects of breathing small amounts of volatile agents are thought to be minimal, if any. Effects of N2O are now considered potentially more harmful; increased incidence of spontaneous abortion and possibly congenital malformation in theatre workers or their spouses is suspected but has never been conclusively proven. This may be via methionine synthase inhibition.
inhalational agents: fears were expressed, especially in the 1960s, because of reported high incidence of lymphoid tumours in anaesthetists. Chronic exposure to low concentrations of volatile agent was thought to be responsible, hence attempts to remove it from the immediate atmosphere by adsorption or scavenging. Such an association was not supported by subsequent studies, and effects of breathing small amounts of volatile agents are thought to be minimal, if any. Effects of N2O are now considered potentially more harmful; increased incidence of spontaneous abortion and possibly congenital malformation in theatre workers or their spouses is suspected but has never been conclusively proven. This may be via methionine synthase inhibition.
Effect on performance is controversial; there is no conclusive evidence that the low atmospheric concentrations measured are deleterious. Any risks are reduced by scavenging, avoiding spillage, monitoring contamination levels and testing apparatus for leaks. Workplace exposure limits set out in COSHH regulations for Great Britain and Northern Ireland are 100 ppm N2O, 50 ppm enflurane/isoflurane and 10 ppm halothane (each over an 8-h period). In the USA, the National Institute for Occupational Safety and Health has recommended an 8-h time-weighted average limit of 2 ppm for halogenated anaesthetic agents in general (0.5 ppm together with exposure to N2O).
 infection, e.g. with hepatitis or HIV infection. Risks are reduced by immunisation against hepatitis B, wearing of gloves and goggles, avoidance of needles wherever possible, and careful disposal of any contaminated equipment. Needles should never be resheathed by holding their cover in one’s hand. Devices for safe handling of used needles (e.g. non-removable caps or cannulae/syringes with self-retracting needles) became mandatory in the USA in 2001, with European legislation introduced in 2006. In case of accidental needlestick injuries:
infection, e.g. with hepatitis or HIV infection. Risks are reduced by immunisation against hepatitis B, wearing of gloves and goggles, avoidance of needles wherever possible, and careful disposal of any contaminated equipment. Needles should never be resheathed by holding their cover in one’s hand. Devices for safe handling of used needles (e.g. non-removable caps or cannulae/syringes with self-retracting needles) became mandatory in the USA in 2001, with European legislation introduced in 2006. In case of accidental needlestick injuries:
– testing for HIV and hepatitis infection requires informed patient consent and counselling, a cause of much controversy should a healthcare worker suffer a needlestick injury from an unconscious patient. If considered necessary, PEP with 2–3 antiretroviral agents (including zidovudine) started within 72 h after exposure and continued for 28 days is recommended. PEP reduces the risk of infection by 80%. Follow-up HIV serology testing should be performed at 1, 3 and 6 months.
Risk of infection after accidental exposure of healthcare workers is estimated at 0.3% for HIV (needlestick; higher risk after conjunctival inoculation), 3% for hepatitis C and up to 30% for hepatitis B. Risk is affected by the number of viral particles inoculated and the route. Other more contagious infections: deaths were reported following exposure to patients infected with severe acute respiratory syndrome.
 risk of electrocution and burns, explosions and fires, radiation exposure, back injury, stress and fatigue. Access to addictive drugs makes abuse of anaesthetic agents easier. Alcohol abuse is common among doctors. Increased risk of suicide is suspected, but not proven.
risk of electrocution and burns, explosions and fires, radiation exposure, back injury, stress and fatigue. Access to addictive drugs makes abuse of anaesthetic agents easier. Alcohol abuse is common among doctors. Increased risk of suicide is suspected, but not proven.
Similar concerns exist for staff on the ICU.
Andersen MP, Nielsen OJ, Wallington TJ (2012). Anesth Analg; 114: 1081–5
See also, Contamination of anaesthetic equipment; COSHH regulations
• Classified according to the reaction catalysed:
 oxidoreductases: oxidation/reduction, e.g. metabolism of many drugs.
oxidoreductases: oxidation/reduction, e.g. metabolism of many drugs.
 transferases: transfer of groups between molecules, e.g. transaminases.
transferases: transfer of groups between molecules, e.g. transaminases.
 hydrolases: hydrolytic cleavage or reverse, e.g. acetylcholinesterase.
hydrolases: hydrolytic cleavage or reverse, e.g. acetylcholinesterase.
 isomerases: intramolecular rearrangements, e.g. mutases.
isomerases: intramolecular rearrangements, e.g. mutases.
 ligases: reactions involving high-energy bonds, e.g. ATP, and formation of C–C, C–N, etc.
ligases: reactions involving high-energy bonds, e.g. ATP, and formation of C–C, C–N, etc.
See also, Enzyme induction/inhibition; Michaelis–Menten kinetics
• May affect metabolism of the original drug and other drugs, leading to drug interactions, e.g.:
– barbiturates increase metabolism of warfarin, phenytoin and chlorpromazine.
– phenytoin increases metabolism of digitoxin, thyroxine, vecuronium, pancuronium and tricyclic antidepressants.
– alcohol increases metabolism of warfarin, barbiturates and phenytoin.
– smoking increases metabolism of vecuronium, pancuronium, morphine, aminophylline, chlorpromazine and phenobarbital.
– ecothiopate reduces metabolism of suxamethonium.
– metronidazole reduces metabolism of acetaldehyde produced by alcohol metabolism.
– cimetidine reduces metabolism of lidocaine, morphine, pethidine, labetalol, propranolol and nifedipine.
Ephedrine hydrochloride. Sympathomimetic and vasopressor drug, mainly used to treat hypotension (especially in spinal and epidural anaesthesia). Sometimes used in the treatment of bronchospasm and autonomic neuropathy.
• Actions:
 directly stimulates α- and β-adrenergic receptors.
directly stimulates α- and β-adrenergic receptors.
 releases noradrenaline from nerve endings.
releases noradrenaline from nerve endings.
• Effects:
 increased heart rate, myocardial contractility and BP.
increased heart rate, myocardial contractility and BP.
 CNS arousal and pupillary dilatation.
CNS arousal and pupillary dilatation.
• Dosage:
Tachyphylaxis occurs with repeated administration. May cause restlessness and palpitations in overdose.
Epidural anaesthesia. Introduction of local anaesthetic agent into the epidural space in order to induce loss of sensation adequate for surgery (the term ‘epidural analgesia’ refers to provision of pain relief, e.g. during labour). Can be divided anatomically into cervical, thoracic, lumbar and caudal. Caudal analgesia was first performed in 1901; lumbar blockade was performed by Pages in 1921 and popularised by Dogliotti in the 1920s–1930s, although it was probably introduced by Corning following his initial experiments. Continuous catheter techniques were introduced in the late 1940s.
Following injection, local anaesthetic may act at epidural, paravertebral or subarachnoid nerve roots, or directly at the spinal cord. Systemic effects may also occur.
Indications are as for spinal anaesthesia; main advantages are avoidance of dural puncture, and those related to catheter technique, i.e. allows control over onset, extent and duration of blockade. Thus used for peri- and postoperative analgesia, analgesia following chest trauma, obstetric analgesia and anaesthesia, and treatment of chronic pain. However, blockade is less intense than spinal anaesthesia, with greater chance of missed segments, and the dose of drug injected is potentially dangerous if incorrectly placed.
Opioid analgesic drugs may be injected into the epidural space to provide analgesia.
(For anatomy, path taken by needle, etc., see Epidural space.)
 deep and superficial infiltration with local anaesthetic is performed.
deep and superficial infiltration with local anaesthetic is performed.
 16–19 G Tuohy needles are usually employed, especially for catheter insertion. The curved blunt tip reduces the risk of dural puncture and facilitates catheter direction (Fig. 63). The needle is usually marked at 1 cm intervals (Lee markings), and may be winged. The Crawford needle (straight-tipped with an oblique bevel) is sometimes used. The stylet is removed when the needle tip is gripped by the interspinous ligament (see Vertebral ligaments). Less damage to the longitudinal ligamentous fibres has been claimed if the needle is inserted with the bevel facing laterally; the needle may then be rotated 90° once the space is entered. However, insertion with the bevel facing cranially is usually advocated, since this avoids the risk of dural puncture during rotation of the needle.
16–19 G Tuohy needles are usually employed, especially for catheter insertion. The curved blunt tip reduces the risk of dural puncture and facilitates catheter direction (Fig. 63). The needle is usually marked at 1 cm intervals (Lee markings), and may be winged. The Crawford needle (straight-tipped with an oblique bevel) is sometimes used. The stylet is removed when the needle tip is gripped by the interspinous ligament (see Vertebral ligaments). Less damage to the longitudinal ligamentous fibres has been claimed if the needle is inserted with the bevel facing laterally; the needle may then be rotated 90° once the space is entered. However, insertion with the bevel facing cranially is usually advocated, since this avoids the risk of dural puncture during rotation of the needle.
 the epidural space is identified by exploiting the negative pressure that is usually present within it. Methods include: the hanging drop technique; a bubble indicator placed at the needle hub; collapsing drums or balloons (e.g. Macintosh’s); and the ‘loss of resistance’ technique:
the epidural space is identified by exploiting the negative pressure that is usually present within it. Methods include: the hanging drop technique; a bubble indicator placed at the needle hub; collapsing drums or balloons (e.g. Macintosh’s); and the ‘loss of resistance’ technique:
– saline: minimal ‘give’ when compressed, thus easier to judge resistance to injection. May be confused with CSF if dural puncture occurs (differentiated by detection of glucose/protein in CSF but not in saline, using reagent strips).
– air: avoids confusion with CSF but compressible in the syringe, i.e. ‘bounces’; judgement of loss of resistance is therefore harder. Neckache is common and thought to be caused by small air emboli (may be detected by sensitive Doppler ultrasound). Pneumocephalus has been reported.
– local anaesthetic: may be less painful during insertion, but risks iv or subarachnoid injection.
 injection of a test dose through the needle is controversial and rarely performed, especially if a catheter is to be inserted.
injection of a test dose through the needle is controversial and rarely performed, especially if a catheter is to be inserted.
– single or fractionated injections are controversial, as above.
– assessment and management of blockade: as for spinal anaesthesia.
 a catheter technique is almost always used.
a catheter technique is almost always used.
 bupivacaine, levobupivacaine or ropivacaine 0.25–0.75%, and lidocaine 1–2%, are most commonly used in the UK. Onset with bupivacaine is about 15–30 min; effects last about 1.5–2.5 h. Lower concentrations of bupivacaine (≤ 0.1%), especially combined with opioids, e.g. fentanyl 2–4 µg/ml, are commonly used to provide analgesia whilst allowing mobility, particularly in obstetrics and for postoperative analgesia (see Spinal opioids). Infusions (≤ 15–20 ml/h) or boluses (≤ 20 ml) may be used; the former are especially common postoperatively since the duration of action is shorter than with concentrated solutions. Onset with lidocaine is about 5–15 min; effects last about 1–1.5 h if 1: 200 000 adrenaline is added. Higher concentrations are used if muscle relaxation is required. Alkalinised solutions produce faster onset of denser blockade.
bupivacaine, levobupivacaine or ropivacaine 0.25–0.75%, and lidocaine 1–2%, are most commonly used in the UK. Onset with bupivacaine is about 15–30 min; effects last about 1.5–2.5 h. Lower concentrations of bupivacaine (≤ 0.1%), especially combined with opioids, e.g. fentanyl 2–4 µg/ml, are commonly used to provide analgesia whilst allowing mobility, particularly in obstetrics and for postoperative analgesia (see Spinal opioids). Infusions (≤ 15–20 ml/h) or boluses (≤ 20 ml) may be used; the former are especially common postoperatively since the duration of action is shorter than with concentrated solutions. Onset with lidocaine is about 5–15 min; effects last about 1–1.5 h if 1: 200 000 adrenaline is added. Higher concentrations are used if muscle relaxation is required. Alkalinised solutions produce faster onset of denser blockade.
 lumbar blockade: 10–30 ml is usually adequate. Rough guide: 1.5 ml/segment to be blocked, including sacral segments; 1.0 ml/segment if over 50 years or in pregnancy; 0.75 ml/segment if over 80 years.
lumbar blockade: 10–30 ml is usually adequate. Rough guide: 1.5 ml/segment to be blocked, including sacral segments; 1.0 ml/segment if over 50 years or in pregnancy; 0.75 ml/segment if over 80 years.
Effect of gravity: the dependent side tends to experience faster and denser block.
 thoracic block: 3–5 ml is used to block 2–4 segments at the required level.
thoracic block: 3–5 ml is used to block 2–4 segments at the required level.
 cervical block: 6–8 ml is usually used.
cervical block: 6–8 ml is usually used.
 tachyphylaxis is common; it may be related to local pH changes but the precise mechanism is unclear.
tachyphylaxis is common; it may be related to local pH changes but the precise mechanism is unclear.
• Effects: similar to spinal anaesthesia, but block (and hypotension) are slower in onset. Density of block and muscle relaxation are less, with greater incidence of incomplete block. Motor block may be assessed using the Bromage scale.
• Contraindications: as for spinal anaesthesia.
 related to insertion of needle/catheter:
related to insertion of needle/catheter:
– trauma:
– dural tap: usually obvious if caused by the epidural needle, as CSF flows back. Puncture by the epidural catheter may be harder to detect; flow of CSF may not be obvious, especially if saline was used to identify the epidural space.
– knotting of the catheter is possible if excessive lengths are inserted.
– hypotension as for spinal anaesthesia.
– local anaesthetic toxicity due to systemic absorption or iv injection.
– accidental spinal blockade (subarachnoid): onset is usually within a few minutes. May lead to total spinal block if a large amount of drug is injected, with rapidly ascending motor and sensory blockade, respiratory paralysis and central apnoea, cranial nerve involvement with fixed dilated pupils and loss of consciousness. Management includes oxygenation with tracheal intubation and IPPV, and cardiovascular support. Recovery without adverse effects is usual if hypoxaemia and hypotension are avoided.
– isolated cranial nerve palsies, e.g. fifth and sixth, and Horner’s syndrome, have been reported.
Extensive blocks may develop after top-up injections during apparently normal epidural blocks.
– prolonged blockade: uncommon; has lasted up to 8–12 h after the last injection.
– anterior spinal artery syndrome: thought to be related to severe hypotension, not to the technique itself.
– adverse drug reactions to agents used: rare.
– arachnoiditis, cauda equina syndrome.
– abscess formation/meningitis: thought to be rare if aseptic techniques are used.
Epidural opioids, see Spinal opioids
Epidural space. Continuous space within the vertebral column, extending from the foramen magnum to the sacrococcygeal membrane of the sacral canal. The vertebral canal becomes triangular in cross-section in the lumbar region, its base anterior; the epidural space is that part external to the spinal dura. It is very narrow anteriorly, and up to 5 mm wide posteriorly.
 internal: dura mater of the spinal cord (at the foramen magnum, reflected back as the periosteal lining of the vertebral canal).
internal: dura mater of the spinal cord (at the foramen magnum, reflected back as the periosteal lining of the vertebral canal).
– posteriorly: ligamenta flava, and periosteum lining the vertebral laminae.
Contains epidural fat, epidural veins (Batson’s plexus), lymphatics and spinal nerve roots. Connective tissue layers have been demonstrated by radiology and endoscopy within the epidural space, in some cases (rarely) dividing it into right and left portions.
 artefactual or transient negative pressure:
artefactual or transient negative pressure:
– anterior dimpling of the dura by the needle.
– back flexion causing stretching of the dural sac, and/or squeezing out of CSF.
– transmitted negative intrapleural pressure via thoracic paravertebral spaces.
– relative overgrowth of the vertebral canal compared with the dural sac.
– true positive pressure: bulging of dura due to pressure of CSF.
• Passage taken by an epidural needle when entering the epidural space (median approach):
 3: supraspinous ligament (along the tips of spinous processes from C7 to sacrum).
3: supraspinous ligament (along the tips of spinous processes from C7 to sacrum).
 4: interspinous ligament (between spinous processes of adjacent vertebrae).
4: interspinous ligament (between spinous processes of adjacent vertebrae).
 5: ligamentum flavum (between laminae of adjacent vertebrae).
5: ligamentum flavum (between laminae of adjacent vertebrae).
The normal distance between the skin and the epidural space varies between 2 and 9 cm.
For the lateral approach: 1, 2, 5, 6.
See also, Epidural anaesthesia; Vertebrae; Vertebral ligaments
Epidural volume expansion, see Combined spinal–epidural anaesthesia
Epiglottitis. Infective inflammation of the epiglottis, often resulting in upper airway obstruction. Caused by Haemophilus influenzae type b in over 50% of cases. Most common in children aged 2–5 years but may also occur in adults (usually aged 20–40 years); the incidence in the UK has fallen since a specific vaccine was introduced. Classically follows an acute course, with fever, marked systemic upset, stridor and adoption of the sitting position with the jaw thrust forward and an open drooling mouth. These features, plus absence of cough, help distinguish it from croup. Epiglottitis may progress to complete airway obstruction, which may be provoked by pharyngeal examination and anxiety (e.g. due to iv cannulation). Although lateral X-rays of the neck may reveal epiglottic enlargement, they may also provoke obstruction, and clinical assessment is sufficient in severe cases. Pulmonary oedema may occur if obstruction is severe.
– general state: exhaustion, toxaemia, etc.
– respiratory distress: stridor, use of accessory respiratory muscles, including flaring of the nostrils, intercostal and suprasternal recession, tachypnoea, cyanosis.
 experienced anaesthetic, paediatric and ENT help should be sought.
experienced anaesthetic, paediatric and ENT help should be sought.
 nebulised adrenaline (0.4 ml/kg [400 µg/kg] of a 1 : 1000 racemic solution to a maximum of 5 ml [5 mg]).
nebulised adrenaline (0.4 ml/kg [400 µg/kg] of a 1 : 1000 racemic solution to a maximum of 5 ml [5 mg]).
 iv fluids and antibacterial drugs are required, although iv cannulation should not be attempted before relief of the airway obstruction. Third-generation cephalosporins are the drugs of choice because of increasing resistance to the traditionally used chloramphenicol or ampicillin.
iv fluids and antibacterial drugs are required, although iv cannulation should not be attempted before relief of the airway obstruction. Third-generation cephalosporins are the drugs of choice because of increasing resistance to the traditionally used chloramphenicol or ampicillin.
 anaesthesia is as for airway obstruction; commonly inhalational induction using sevoflurane in O2 with the patient sitting until tracheal intubation is possible. Induction is usually slow. Apparatus for difficult intubation plus facilities for urgent tracheostomy must be available. Atropine may be given once an iv cannula is sited. An oral tracheal tube is passed initially, and is changed for a nasal tube to allow better fixation and comfort.
anaesthesia is as for airway obstruction; commonly inhalational induction using sevoflurane in O2 with the patient sitting until tracheal intubation is possible. Induction is usually slow. Apparatus for difficult intubation plus facilities for urgent tracheostomy must be available. Atropine may be given once an iv cannula is sited. An oral tracheal tube is passed initially, and is changed for a nasal tube to allow better fixation and comfort.
 intubation is usually required for less than 24 h. Spontaneous ventilation is usually acceptable. Humidification is essential. Sedation may not be required, but care must be taken to avoid accidental extubation.
intubation is usually required for less than 24 h. Spontaneous ventilation is usually acceptable. Humidification is essential. Sedation may not be required, but care must be taken to avoid accidental extubation.
 members of the patient’s household should receive prophylactic antibacterial agents.
members of the patient’s household should receive prophylactic antibacterial agents.
• Traditionally classified into:
– grand mal (tonic–clonic convulsions): tonic (sustained muscle contraction) followed by clonic (jerking) phases lasting about 30 s each, with loss of consciousness. May be preceded by prodromal symptoms hours or days before, and an aura minutes before.
– other types of generalised seizures include atonic and myoclonic.
– may occur with (complex partial) or without (simple partial) derangement of consciousness.
Definition of disease is difficult because certain stimuli will induce convulsions in normal subjects, e.g. hypoxia, hypo/hyperglycaemia. Usually idiopathic, especially in childhood; intracranial lesions and infections (e.g. encephalitis) must be excluded in adults presenting with a single seizure. Pyrexia is a common cause in children; other causes are as for convulsions.
Treatment is with anticonvulsant drugs, and is directed at any underlying cause.
 preoperative assessment: frequency of seizures, date of last seizure, drug therapy (including measurement of blood levels where appropriate). Identification of cause if known.
preoperative assessment: frequency of seizures, date of last seizure, drug therapy (including measurement of blood levels where appropriate). Identification of cause if known.
 therapy is continued throughout the perioperative period; benzodiazepines are often used for premedication because of their anticonvulsant activity.
therapy is continued throughout the perioperative period; benzodiazepines are often used for premedication because of their anticonvulsant activity.
 anaesthetic drugs associated with convulsions are avoided, e.g. enflurane, ketamine. Although propofol may activate the EEG at low concentrations and may cause myoclonic jerks, it is used successfully to treat status epilepticus. Thiopental, halothane and isoflurane have anticonvulsant properties and are therefore the traditional drugs of choice. Doxapram, naloxone and tramadol are avoided. Hypocapnia lowers the seizure threshold.
anaesthetic drugs associated with convulsions are avoided, e.g. enflurane, ketamine. Although propofol may activate the EEG at low concentrations and may cause myoclonic jerks, it is used successfully to treat status epilepticus. Thiopental, halothane and isoflurane have anticonvulsant properties and are therefore the traditional drugs of choice. Doxapram, naloxone and tramadol are avoided. Hypocapnia lowers the seizure threshold.
 anticonvulsant therapy is restarted as soon as possible postoperatively.
anticonvulsant therapy is restarted as soon as possible postoperatively.
[John Hughlings Jackson (1835–1911), English neurologist]
Perks A, Cheema S, Mohanraj R (2012). Br J Anaesth; 108: 562–71
Epinephrine, see Adrenaline
Epistaxis. Nasal bleeding. May occur from:
 veins of the nasal septum (younger patients).
veins of the nasal septum (younger patients).
 arterial anastomoses of the lower part of the nasal septum (Little’s area), especially in older patients. May be associated with hypertension.
arterial anastomoses of the lower part of the nasal septum (Little’s area), especially in older patients. May be associated with hypertension.
Usually follows trauma, but predisposing conditions include bleeding disorders, hereditary telangiectasia and raised venous pressure. Bleeding may be caused by nasal intubation or passage of a nasal airway, especially if a vasoconstrictor (e.g. cocaine) is not used first.
Usually managed by nasal packing but may require ligation of the maxillary or anterior ethmoidal arteries, the former via the neck or oral route, the latter from the front of the nose.
Anaesthetic management is similar to that of the bleeding tonsil (see Tonsil, bleeding).
Epoprostenol, see Prostacyclin
Eptacog alfa. Recombinant activated coagulation factor VIIa. Prohaemostatic agent that activates the coagulation cascade mainly via factors IX and X. Used for patients with complicated coagulation disorders, both pre-existing (e.g. certain types of haemophilia) and acquired, e.g. after major surgery or trauma. Because of the difficulty studying the latter group, most experience is limited to case series and anecdotal reports and this, along with the high cost of the preparation (~£500 per mg), makes its use controversial. Associated with a 1–2% incidence of thrombotic complications, adding to the controversy. Requires functioning platelets and normal fibrinogen levels for maximal clinical effect.
Levi M, Peters M, Buller HR (2005). Crit Care Med; 33: 883–90
Eptifibatide. Antiplatelet drug, used in some acute coronary syndromes. Acts by reversibly inhibiting activation of the glycoprotein IIb/IIIa complex on the surface of platelets.
Equivalence. Amount of a substance divided by its valence. Equivalent weight (gram equivalent) is the weight of substance combining with or chemically equivalent to 8 g O2, or 1 g hydrogen.
Electrical equivalence is the number of moles of ionised substance divided by valence.
Erg. Unit of work in the cgs system. 1 erg = work done by a force of 1 dyne acting through a distance of 1 centimetre.
Ergometrine maleate. Smooth muscle constrictor, with potent effects on uterine and vascular tone; used to reduce postpartum or post-termination uterine bleeding. Uterine contraction occurs 5 min after im injection and 1 min after iv injection; it lasts up to an hour. Slowly being replaced by synthetic oxytocin because of its adverse effects (nausea, vomiting and vasoconstriction causing a marked rise in BP and CVP; the latter is exacerbated by autotransfusion of blood from the uterus, and lasts up to several hours). Therefore hazardous in patients with cardiovascular disease, particularly pre-eclampsia. Despite this, it is often given routinely combined with oxytocin at the end of the second stage of labour. An aggravating role of ergometrine-induced vasoconstriction has been suggested in aspiration pneumonitis. Has been used as a vasopressor, e.g. in spinal anaesthesia.
Error, fixation, see Fixation error
Errors, statistical. In statistics, may lead to incorrect conclusions because of inadequate test design and analysis, too small a sample size or inaccurate data collection. Include:
 type I (α; false positive): acceptance of a result as not due to chance when it is (i.e. false rejection of the null hypothesis). Represented by the P value (probability); a value of 0.05 is usually accepted as the maximum acceptable.
type I (α; false positive): acceptance of a result as not due to chance when it is (i.e. false rejection of the null hypothesis). Represented by the P value (probability); a value of 0.05 is usually accepted as the maximum acceptable.
It is thus ‘easier’ to demonstrate a non-significant result than a significant one. As the required P value is made smaller, the risk of rejecting a real result (i.e. type II error) increases (assuming a constant sample size). Errors may limit the usefulness of an investigation described by its sensitivity, specificity and predictive value.
Ertapenem. Broad-spectum carbapenem and antibacterial drug, active against Gram-positive organisms and anaerobes, but not against pseudomonas or acinetobacter species, unlike imipenem or meropenem.
Erythrocytes (Red blood cells). Biconcave discs, about 2 µm thick and 8 µm in diameter and without nuclei. Produced by red bone marrow. Contain haemoglobin, maintained in an appropriate state for O2 transport (i.e. containing iron in the reduced state, in the presence of 2,3-DPG). Also have an integral role in carbon dioxide transport. Maintenance of structural integrity and osmotic stability is via membrane pumps; the main energy source is aerobic glycolysis.
• Normal laboratory findings (adult):
 red cell count (RBC): 4.5–6.0 × 1012/l blood (male); 4.0–5.2 × 1012/l blood (female).
red cell count (RBC): 4.5–6.0 × 1012/l blood (male); 4.0–5.2 × 1012/l blood (female).
 reticulocyte count: < 2% of red cells. Increased in red cell loss from haemolysis or haemorrhage, signifying a normal bone marrow response. Also increased in treatment of deficiency anaemias.
reticulocyte count: < 2% of red cells. Increased in red cell loss from haemolysis or haemorrhage, signifying a normal bone marrow response. Also increased in treatment of deficiency anaemias.
 mean corpuscle volume (MCV): 80–100 fl. Decreased in iron deficiency or defective haemoglobin synthesis. Increased when reticulocyte count is increased, or due to megaloblastic cell formation (e.g. vitamin B12/folate deficiency). Also increased in alcoholism.
mean corpuscle volume (MCV): 80–100 fl. Decreased in iron deficiency or defective haemoglobin synthesis. Increased when reticulocyte count is increased, or due to megaloblastic cell formation (e.g. vitamin B12/folate deficiency). Also increased in alcoholism.
Examination of the peripheral blood film gives information about haematological disease, e.g. abnormally shaped erythrocytes (sickle cell anaemia, hereditary spherocytosis, target cells in impaired haemoglobin production or liver disease).
Erythromycin. Macrolide-type antibacterial drug with similar spectrum to penicillin; thus a useful alternative in penicillin allergy. Especially useful in respiratory infections (including Legionnaires’ disease and Mycoplasma infections) and staphylococcal infections. Also promotes GIT activity via stimulation of GIT motilin receptors; used as a prokinetic drug in ileus (given iv or via nasogastric tube).
Erythropoiesis. Formation of erythrocytes, usually restricted to the vertebrae, sternum, ribs, upper long bones and iliac crests in adults. Requires iron, vitamin B12 and folate, and possibly other vitamins and minerals. Stepwise differentiation from stem cells includes haemoglobin synthesis and nuclear extrusion to form reticulocytes, taking about 7 days. Regulated by erythropoietin.
Erythropoietin. Glycoprotein hormone secreted mainly by the kidneys, but also by the liver. Secretion is increased by haemorrhage and hypoxia (possibly via prostaglandin synthesis), and inhibited by increased numbers of circulating erythrocytes. Causes increased erythropoiesis. Erythropoietin receptors are present in erythrocytes, bone marrow and on central and peripheral neurones; the latter are involved in neuronal development and repair. Infusion of erythropoietin produced by recombinant genetic engineering has been used to treat anaemia in renal failure, but treatment is very expensive. It has also been used to increase the yield of blood collected for autologous blood transfusion, e.g. 300 U/kg thrice weekly, reducing to 100 U/kg after 2 weeks. The first dose given iv produces higher levels; subsequent sc dosage produces a more sustained effect. Red cell aplasia has been reported following its sc use in renal failure.
Escape beats. On the ECG, complexes arising from sites other than the sinoatrial node, when the latter does not discharge (i.e. sinus arrest or severe bradycardia). Distinct from ectopic beats, which arise prematurely in the cardiac cycle.
Esmolol hydrochloride. Cardioselective β-adrenergic receptor antagonist, with no intrinsic sympathomimetic activity. Hydrolysed by red blood and other esterases, with a half-life of 9 min. Used to treat AF, atrial flutter and SVT, and during anaesthesia to prevent/treat tachycardia and hypertension, e.g. associated with tracheal intubation. Has been used in hypotensive anaesthesia.
Esophagus, see Oesophagus
Etamsylate (Ethamsylate). Haemostatic drug, thought to reduce bleeding by correcting abnormal platelet adhesion. Does not affect fibrinolysis. Has been used to prevent and treat periventricular haemorrhage in premature babies (12.5 mg/kg im/iv qds).
Ethambutol hydrochloride. Antituberculous drug added to triple therapy (isoniazid, rifampicin, pyrazinamide) if resistance is suspected.
Ethamsylate, see Etamsylate
Ethanol poisoning, see Alcohol poisoning
Ether, see Diethyl ether
The principles underlying ethical practice are not mutually exclusive and may even oppose one another, e.g. withholding blood from a Jehovah’s Witness respects his/her autonomy whilst not practising beneficence/non-maleficence.
• Anaesthetic/ICU implications include:
 patients’ rights to confidentiality, including non-disclosure of records without permission, although the doctor has statutory duties that may override this (e.g. reporting of notifiable diseases, births and deaths).
patients’ rights to confidentiality, including non-disclosure of records without permission, although the doctor has statutory duties that may override this (e.g. reporting of notifiable diseases, births and deaths).
 HIV infection: there is a moral duty to treat infected patients as well as taking steps to protect oneself. A doctor who has reason to believe that he/she is infected has a duty to seek advice and testing.
HIV infection: there is a moral duty to treat infected patients as well as taking steps to protect oneself. A doctor who has reason to believe that he/she is infected has a duty to seek advice and testing.
 the duty to seek Research Ethics Committee approval and informed consent for research.
the duty to seek Research Ethics Committee approval and informed consent for research.
 the duty to protect patients from sick and incompetent medical colleagues (see Sick Doctor Scheme).
the duty to protect patients from sick and incompetent medical colleagues (see Sick Doctor Scheme).
 do not attempt resuscitation orders and advance decisions.
do not attempt resuscitation orders and advance decisions.
 admission criteria for, and rationing of, intensive care.
admission criteria for, and rationing of, intensive care.
 withholding or withdrawal of treatment (including surgery) in cases of medical futility.
withholding or withdrawal of treatment (including surgery) in cases of medical futility.
Ethmoidal nerve block, anterior, see Ophthalmic nerve blocks
Ethoheptazine citrate. Analgesic drug, used for mild/moderate pain. Combined with meprobamate, a sedative muscular antispasmodic, and aspirin. Not available in the UK.
Ethosuximide. Anticonvulsant drug used in petit mal epilepsy and myoclonic seizures. Thought to block T-type calcium channels in thalamic neurones.
Ethyl alcohol, see Alcohol poisoning; Alcohol withdrawal syndromes; Alcoholism; Alcohols
Ethyl chloride. Inhalational anaesthetic agent, first described in 1848; popular in the 1920s particularly for induction of anaesthesia because of its rapid action. Extremely volatile (boiling point 13°C) and difficult to control; also inflammable. Now used solely for its cooling action when sprayed on to skin, to cause anaesthesia before minor procedures or to test the extent of regional blockade.
Ethylene. Inhalational anaesthetic agent, used clinically in 1923. A gas of similar blood/gas solubility to N2O, but more potent. Also extremely explosive and unpleasant to inhale. Cylinder body and shoulder are coloured violet.
Ethylene glycol poisoning, see Alcohol poisoning
Ethylene oxide, see Contamination of anaesthetic equipment
Etidocaine hydrochloride. Local anaesthetic agent introduced in 1972, derived from lidocaine. Onset is rapid, and duration of action is similar to that of bupivacaine. Produces motor blockade that may exceed sensory blockade. Used in 1–1.5% solutions. Maximal safe dose is 2 mg/kg. Not available in the UK.
Etomidate. IV anaesthetic agent, introduced in 1973. A carboxylated imidazole (five-membered ring containing three carbon atoms and two nitrogen atoms) compound (Fig. 64), presented in 35% propylene glycol; pH is 8.1. 75% bound to plasma proteins after injection. Methoxycarbonyl-etomidate (MOC-etomidate) is a new etomidate analogue that is rapidly metabolised and does not cause adrenocortical suppression (see below).
• Effects:
– rapid onset of anaesthesia, lasting up to 8 min after a single dose.
– muscle contractions are common; reduced by use of opioids.
– causes less hypotension than propofol and thiopental; thus often used in shocked patients, the elderly and those with cardiovascular disease.
– respiratory depression is less than with thiopental.
– not associated with epileptiform discharges.
– reduces cerebral blood flow and intraocular pressure.
– increases the incidence of PONV.
– does not cause histamine release.
 rapidly metabolised by plasma esterases and liver enzymes; elimination half-life is about 70 min. Largely excreted via the urine. Not cumulative.
rapidly metabolised by plasma esterases and liver enzymes; elimination half-life is about 70 min. Largely excreted via the urine. Not cumulative.
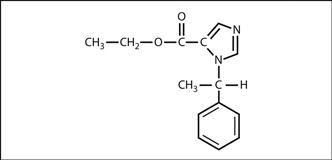
Fig. 64 Structure of etomidate
Etorphine hydrochloride. Analogue of thebaine, a naturally occurring opioid. 1000–3000 times as potent as morphine. Used to immobilise large animals.
European Academy of Anaesthesiology (EAA). Founded in 1978 to improve standards, training and research in anaesthesia. Organises the European Diploma in Anaesthesiology and Intensive Care. Amalgamated with the European Society of Anaesthesiologists and the Confederation of European National Societies of Anaesthesiologists to form the European Society of Anaesthesiology in 2005.
European Board of Anaesthesiology (EBA). Governing body for specialist anaesthetic training within the European Union, under the auspices of the European Union of Medical Specialties, which was founded in 1958. Works with the various anaesthetic bodies in member states.
European Diploma in Intensive Care Medicine (EDIC). Organised by the European Society of Intensive Care Medicine since 1989. Consists of an English written (multiple choice) examination and an oral/clinical one (usually in the country and language of the examinee), together with a requirement for a basic medical specialty and 2 years’ intensive care medicine training.
European Diploma in Anaesthesiology and Intensive Care (EDAIC). Examination held since 2005 by the European Society of Anaesthesiology, having taken over this function from the European Academy of Anaesthesiology, which ran it from 1984. Available in multiple languages; consists of two parts (written and oral), each covering basic science and clinical topics. Pass rates are in the order of 60% and 80% respectively. There is also an optional in-training assessment part.
European Federation of Anaesthesiologists (EFA). Umbrella organisation formed in 2001 to coordinate the activities of and encourage cooperation between the European Academy of Anaesthesiology, European Society of Anaesthesiologists and Confederation of European National Societies of Anaesthesiology. Adopted the European Journal of Anaesthesiology as its official journal.
European Journal of Anaesthesiology. Established in 1984. The official journal of the European Society of Anaesthesiology, having been the official journal of the European Academy of Anaesthesiology, the European Society of Anaesthesiologists, the Confederation of European National Societies of Anaesthesiology, Fondation Européenne d’Enseignement en Anaesthésiologie and European Union of Medical Specialties (since 1999) and the European Federation of Anaesthesiologists (since 2001).
European Medicines Evaluation Agency (EMEA). Body established in 1995 to regulate the introduction and investigation of new drugs throughout Europe, and to ease communication between the various national regulatory bodies. Thus acts as a link between the Committee on Safety of Medicines in the UK and similar bodies in other countries.
European Paediatric Life Support (EPLS). Collaboration between the European Resuscitation Council and the Resuscitation Council (UK). The EPLS course provides training for healthcare professionals in the early recognition of the child in respiratory or circulatory failure and the prevention of respiratory or cardiorespiratory arrest.
European Resuscitation Council (ERC). Formed in 1989 with a mandate to produce guidelines and recommendations appropriate to Europe for the practice of basic and advanced cardiopulmonary and cerebral resuscitation. Composed of elected representatives from the participating European countries. Held its first major international conference in 1992. Regularly produces guidelines regarding basic and advanced CPR. Resuscitation is its official journal.
See also, Resuscitation Council (UK); International Liaison Committee on Resuscitation
European Society of Anaesthesiology (ESA). Formed in 2005 by the amalgamation of the European Society of Anaesthesiologists, the European Academy of Anaesthesiology and the Confederation of European National Societies of Anaesthesiologists. Seeks to provide all the educational and regulatory activities of the three component organisations. Adopted the European Journal of Anaesthesiology as its official journal. Representation of different nationalities within the organisation is via individual members (who are all eligible to join the ESA’s various committees) and the National Anaesthesia Societies Committee (NASC).
European Society of Intensive Care Medicine (ESICM). Founded in 1982 in Geneva to advance knowledge, research and education in intensive care medicine, and subsequently to improve facilities for intensive care medicine in Europe. Holds an annual congress, organises the European Diploma in Intensive Care Medicine and administers several multicentre and multinational surveys, e.g. the European Consortium for Intensive Care Data (ECICD). Also administers the educational programme PACT. Intensive Care Medicine is its official journal.
European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Founded and based in Brussels to advance and promote paediatric and neonatal intensive care. Has medical and nursing branches. Holds an annual congress and has Intensive Care Medicine as its official journal.
European Union of Medical Specialties (Union Européenne des Médecins Spécialistes; UEMS), see European Board of Anaesthesiology
In general, most anaesthetic agents increase latency and decrease amplitude (etomidate consistently increases amplitude) in a dose-related manner. Amplitude increases following tracheal intubation or skin incision, suggesting SEPs represent magnitude of stimulus rather than anaesthetic depth. The technique has also been used to monitor function during craniotomy, e.g. measuring CCT: impaired conduction may represent physical damage, hypoxia or ischaemia.
Anaesthetic agents have minimal effects on spinal evoked potentials; the technique is useful for investigating spinal conduction at any anaesthetic depth. Each side is tested individually; amplitude reduction greater than 50% during surgery is likely to indicate postoperative neurological deficit. Used for surgery for kyphoscoliosis, tumours, vascular lesions, etc., also for surgery to the brachial plexus, aortic arch, etc.
– stimulation of the eighth cranial nerves with audible clicks, usually at 6–10 Hz.
– recording from scalp electrodes (e.g. vertex/mastoid), and reference on the forehead.
Kumar A, Bhattacharya A, Makhija N (2000). Anaesthesia; 55: 225–41
Exercise. Produces physiological changes that increase oxygen flux and removal of waste products from active tissues:
– increased cardiac output mainly due to increased heart rate (to a maximum rate of about 195 beats/min in adults). Stroke volume increases slightly in normal individuals, although it can double in trained athletes. The increase in cardiac output starts before exercise due to cortical activation of the sympathetic nervous system. Following initiation of exercise, CVS reflexes are activated following stimulation of muscle mechanoreceptors, baroreceptors and joint receptors.
– BP increases (systolic > diastolic), reflecting increased cardiac output despite decreased SVR due to vasodilatation in exercising muscles.
– increased venous return due to increased skeletal muscle pump activity and thoracic pump action.
– blood flow is diverted to skin and actively contracting muscles at the expense of renal and splanchnic blood flow. Muscle blood flow may increase 30-fold as a result of accumulation of local metabolites (e.g. K+, lactic acid), a decrease in arterial PO2 and an increase in PCO2. Arteriovenous O2 difference may increase threefold due to a shift of the oxyhaemoglobin dissociation curve to the right secondary to the acidosis, raised temperature in muscles and raised 2,3-DPG levels found during exercise.
– coronary blood flow may increase to up to five times the resting level.
– increased minute ventilation due to increase in respiratory rate and tidal volume. The increase is proportional to the rise in oxygen demand and is due to cortical stimulation and afferent impulses from proprioceptors in muscles, tendons and joints.
– CO2 excretion can reach 8000 ml/min.
 temperature regulation: the heat produced is dissipated by increased sweating, skin vasodilation and heat loss through expired air.
temperature regulation: the heat produced is dissipated by increased sweating, skin vasodilation and heat loss through expired air.
If extreme exercise continues, exhaustion follows; BP falls, cutaneous vasoconstriction occurs, body temperature rises and accumulation of lactic acid and CO2 results in increasing acidosis. Muscle cramps and fatigue occur. Exertional myoglobinuria may be seen.
Exercise testing. Most commonly, involves ECG recording while performing exercise, e.g. using a treadmill or bicycle, with workload increased in steps.
Testing is used to help diagnose chest pain or breathlessness, and to indicate prognosis in ischaemic heart disease, especially following MI. S–T depression is the most significant sign during exercise, but other changes, e.g. S–T elevation, Q waves, may occur. Chest pain, hypotension and arrhythmias may also be provoked. Testing may be combined with other measurements, e.g. arterial BP, respiratory rate, tidal volume, O2 consumption, CO2 output, arterial blood gases and cardiac output. Reduced ejection fraction (e.g. demonstrated by echocardiography) or cardiac output may suggest reversible ischaemia that may persist after cessation of exercise (myocardial stunning).
Inotropic drugs, e.g. dobutamine, may also be used to provoke similar changes to those caused by exercise (dobutamine stress test).
Traditionally, the patient’s own exercise tolerance (e.g. maximum walking distance or stairs climbed) has been used as a general indicator of cardiorespiratory function. More recently, formal cardiopulmonary exercise testing has been used to predict outcomes after major surgery, using the work at which maximal O2 consumption is reached, or the work at which anaerobic energy metabolism (anaerobic threshold) starts, as markers of cardiopulmonary reserve.
Albouaini K, Egred M, Alahmar A, Wright DJ (2007). Heart; 93: 1285–92
Exomphalos, see Gastroschisis and exomphalos
Exotoxins. High-molecular-weight, heat-labile and antigenic proteins produced by micro-organisms. Although some bacteria produce only one significant kind of exotoxin (e.g. clostridia), others produce several (e.g. streptococci and staphylococci). Exotoxins and endotoxins contribute to the pathogenesis of SIRS. Some are used clinically, e.g. botulinum toxins.
Expiratory flow rate, see Forced expiratory flow rate
Expiratory reserve volume (ERV). FRC minus residual volume. Normally 1–1.2 litres. Reduced ERV is usually the cause of reduced FRC. See also, Lung volumes
Expiratory valve, see Adjustable pressure-limiting valve
Expired air ventilation. Component of CPR said to be referred to in the Bible (2 Kings 4: 34–5). Reported in the 1700s and 1800s, but only became medically accepted practice in the 1950s, following demonstration that it was effective in apnoea during anaesthesia. Adequate oxygenation may be maintained with expired air of O2 concentration 15–16%.
Regurgitation of gastric contents may occur during expired air ventilation; this may be reduced by application of cricoid pressure if another person is available.
Various devices, some with valves, are available for avoidance of direct mouth-to-mouth contact, to improve aesthetic acceptability and reduce risk of cross-contamination; most hinder efficient ventilation. An anaesthetic facemask is suitable. Expired air ventilation may be performed through a correctly placed tracheal tube or LMA.
Explosions, see Burns; Chest trauma; Explosions and fires; Incident, major; Smoke inhalation; Trauma
Explosions and fires. Occur when a substance combines with O2 or another oxidising agent, with release of energy. Activation energy is required to start the process, with utilisation of energy produced to maintain combustion. If the reaction proceeds very fast, large amounts of heat, light and sound are given out, i.e. an explosion occurs. Speed of reaction is greatest for stoichiometric mixtures.
• The following are required for explosions to occur:
– anaesthetic agents, e.g. cyclopropane, diethyl ether. C–C bonds are susceptible to breakdown; C–F bonds are resistant, hence the non-flammability of modern inhalation anaesthetic agents.
– gases, e.g. methane and hydrogen in the patient’s GIT.
– grease/oil in anaesthetic pressure gauges (see Adiabatic change).
 gas to support combustion: O2 is standard in most anaesthetic techniques. N2O breaks down to O2 and nitrogen with heat, producing further energy; thus reactions may be more vigorous with N2O than with O2 alone.
gas to support combustion: O2 is standard in most anaesthetic techniques. N2O breaks down to O2 and nitrogen with heat, producing further energy; thus reactions may be more vigorous with N2O than with O2 alone.
– build-up of static electricity.
– electrical equipment, e.g. diathermy, monitors, switches.
– naked flames, cigarettes, hot wires, diathermy, light sources.
May result in burns, direct trauma and smoke inhalation. Although uncommon now with modern techniques, explosions and fires continue to be reported.
• Precautions during anaesthesia include:
 antistatic precautions, e.g. conductive rubber, floor.
antistatic precautions, e.g. conductive rubber, floor.
 checking and maintenance of all electrical equipment. Use of spark-free switches.
checking and maintenance of all electrical equipment. Use of spark-free switches.
 air conditioning and scavenging, to reduce levels of anaesthetic agents. Sparks are reduced by maintaining relative humidity above 50%, and temperature above 20°C.
air conditioning and scavenging, to reduce levels of anaesthetic agents. Sparks are reduced by maintaining relative humidity above 50%, and temperature above 20°C.
Fire-fighting equipment should be present in every operating department.
Non-combustion explosions may occur if cylinders are faulty or internal pressure excessively high.
Exponential process. A process in which the rate of change of a quantity at a given time is in constant proportion to the amount of the quantity at that time.
 exponential decay (negative exponential), e.g. passive lung deflation after a breath, radioactive decay, washout curves (Fig. 65a). Similar curves are obtained in pharmacokinetics, in which several curves may be superimposed. For exponential decay:
exponential decay (negative exponential), e.g. passive lung deflation after a breath, radioactive decay, washout curves (Fig. 65a). Similar curves are obtained in pharmacokinetics, in which several curves may be superimposed. For exponential decay:

where A = value of variable at a given time
b = a particular base, usually e (2.718) because mathematical manipulations are easier
k = a constant (the rate constant)
The rate constant (k) is the constant of proportionality linking the rate of the change of the quantity to its value (i.e. k = rate/quantity). Its reciprocal is the time constant (τ), and is also defined as the time required for completion of the process at the initial rate of change. Substituting τ for k (and e for b):

– at time = τ, A = e–1 of its original value = 37% (63% complete);
– at 2τ, A = e–2 of its original value = 13.5% (86.5% complete);
– at 3τ, A = e–3 of its original value = 5% (95% complete).
The duration of the process is also indicated by half-life (time taken for original value to fall by half; Fig. 65b).
 build-up exponential (wash-in curve), e.g. lung inflation with a constant-pressure generator ventilator, or uptake of inhalational anaesthetic agents (Fig. 65c).
build-up exponential (wash-in curve), e.g. lung inflation with a constant-pressure generator ventilator, or uptake of inhalational anaesthetic agents (Fig. 65c).
 positive exponential (breakaway function), e.g. growth of bacteria (Fig. 65d).
positive exponential (breakaway function), e.g. growth of bacteria (Fig. 65d).
Extended mandatory minute ventilation, see Mandatory minute ventilation
External jugular venous cannulation, The external jugular vein passes posteriorly over the sternomastoid muscle from the angle of the jaw and joins the subclavian vein behind the midpoint of the clavicle (see Fig. 86; Internal jugular venous cannulation). It is often visible and thus easier to locate than the internal jugular vein, although valves may hinder cannulation and misplacement is common. In some individuals the vessel is not a distinct structure but is replaced by a venous plexus. The technique of cannulation involves placing the patient slightly head down with the arms by the side and the head turned to the contralateral side. After cleansing the skin, the skin is punctured well above the clavicle and the needle advanced immediately over the vein at about 20° to the frontal plane. A J-wire may help the catheter negotiate the valves at the junction with the subclavian vein.
Extracellular fluid (ECF). Body fluid compartment; volume is about 14 litres (20% of body weight). Consists of interstitial fluid and plasma. Transcellular fluid (approximately 1 litre, composed of CSF, synovial fluid, etc.) and fluid within dense connective tissue, bone, etc., are usually excluded from the definition since these fluids are not readily exchangeable.
Measurement by dilution techniques is difficult because of eventual exchange with the above compartments, and because the substance used must remain extracellular. Substances used include inulin labelled with carbon-14, mannitol, sucrose, chloride-36 ions, bromide-82 ions, sulphate and thiosulphate. Slightly different values are obtained for each.
Compositions of plasma and interstitial fluid are different (see Fluids, body).
Extracorporeal carbon dioxide removal (ECCO2R). Method of respiratory support in which CO2 is removed via a venovenous extracorporeal circuit and oxygenation is maintained by either apnoeic oxygenation or IPPV at very slow rates (1–4 breaths/min). Facilitates lung-protective ventilation strategies by preventing respiratory acidosis. The extracorporeal circuit runs at only 1–2 l/min; thus lung ischaemia is less likely than with extracorporeal membrane oxygenation. Initial human studies showed improved survival rates compared with conventional IPPV.
Practical considerations and complications are as for cardiopulmonary bypass.
Extracorporeal circulation, see Cardiopulmonary bypass; Extracorporeal carbon dioxide removal; Extracorporeal membrane oxygenation; Haemodiafiltration; Haemodialysis; Haemofiltration; Haemoperfusion; Plasmapheresis; Ultrafiltration
Extracorporeal membrane oxygenation (ECMO). Method of respiratory support for extremely hypoxaemic patients despite optimum mechanical ventilation. An arteriovenous extracorporeal circuit provides oxygenation and removal of CO2 from anticoagulated blood. Very successful in neonates (e.g. with respiratory distress syndrome) but results are less clear in adults, in whom it is used mainly for temporary support before lung transplantation. Removal of a large proportion of the cardiac output by the arteriovenous circuit may exacerbate lung ischaemia. Simpler external oxygenators include the Novolung interventional lung assist device, a pumpless alternative that uses an arteriovenous shunt.
Practical considerations and complications are as for cardiopulmonary bypass.
Energy may be released at any interface and cause pain, e.g. at water/skin interfaces; therefore anaesthesia is required. General and regional techniques have been used. High-frequency ventilation has been used, since diaphragmatic movement is reduced. Other anaesthetic considerations are related to positioning, temperature control, inaccessibility of the patient and monitoring, effects of immersion (increased CVP and pulmonary artery pressure) and requests for pharmacological intervention to increase heart rate and thus rate of discharge. IV fluid administration is usually required to produce a good diuresis, to wash away calculi fragments. Renal bleeding may occur if coagulation is impaired.
Plasma lactate dehydrogenase concentrations may be increased postoperatively. PONV is common.
Extraction ratio (ER). Measure of the amount of removal of drug by an organ, e.g. liver:
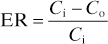
where Ci = drug concentration in blood entering the organ,
Co = drug concentration in blood leaving the organ.
Factors affecting ER include enzyme activity and drug protein-binding.
Drugs with high ER (e.g. lidocaine and propranolol) undergo significant first-pass metabolism in the liver after oral administration. The rate of elimination is thus more dependent on hepatic blood flow than hepatic function; clearance of drugs with a low ER is more sensitive to changes in hepatic function (e.g. enzyme induction/inhibition) than blood flow.
Extradural (epidural) haemorrhage. Haemorrhage between the periosteum and dura.
• May be:
 intracranial: may occur from meningeal vessels (classically the middle meningeal artery), dural sinuses or fractured bone. Features are as for head injury; typically depressed consciousness, contralateral hemiparesis and ipsilateral pupillary dilatation follow a lucid interval of a few hours after recovery from relatively minor trauma. CT shows a typical biconvex hyperintense lesion. Management: as for head injury, with urgent evacuation of the clot.
intracranial: may occur from meningeal vessels (classically the middle meningeal artery), dural sinuses or fractured bone. Features are as for head injury; typically depressed consciousness, contralateral hemiparesis and ipsilateral pupillary dilatation follow a lucid interval of a few hours after recovery from relatively minor trauma. CT shows a typical biconvex hyperintense lesion. Management: as for head injury, with urgent evacuation of the clot.
 spinal: may occur spontaneously in patients with impaired coagulation, or following lumbar puncture, and spinal or epidural anaesthesia. Marked haemorrhage with haematoma formation may cause spinal cord/nerve compression, that may be masked by regional blockade.
spinal: may occur spontaneously in patients with impaired coagulation, or following lumbar puncture, and spinal or epidural anaesthesia. Marked haemorrhage with haematoma formation may cause spinal cord/nerve compression, that may be masked by regional blockade.
Extravascular lung water (EVLW). Volume of water contained within the pulmonary interstitium and alveolar space. Usually 4–5 ml/kg. Measurement of EVLW has attracted attention as a possible means of detecting pulmonary oedema before it becomes apparent, although its usefulness in clinical practice is controversial. Determined by Starling forces and integrity of the pulmonary capillary and alveolar epithelium. Disruption of the former (e.g. by left ventricular failure) or the latter (e.g. in acute lung injury) may result in increased EVLW.
Measured by the double indicator dilution technique in which cold indocyanine dye is injected into the right atrium. The dye is contained within the intravascular space and its dilution curve allows calculation of the intravascular compartment. In contrast, the heat (measured by a thermistor placed in the aorta) from the solution is dissipated into the surrounding lung tissue and its dilution curve represents the sum of the intravascular and extravascular compartments. Subtraction of the curves allows calculation of the EVLW. Other methods of assessing EVLW include CXR, CT and MRI scanning and positron emission tomography techniques.
Extubation, tracheal. Problems that may occur include the following:
 cardiovascular response: similar to that on tracheal intubation but usually of reduced magnitude.
cardiovascular response: similar to that on tracheal intubation but usually of reduced magnitude.
 coughing and laryngospasm: the latter is especially likely to occur at light planes of anaesthesia and in children.
coughing and laryngospasm: the latter is especially likely to occur at light planes of anaesthesia and in children.
In patients in whom deep extubation is unsuitable but when smooth emergence from anaesthesia is particularly important (e.g. neurosurgery, maxillofacial surgery), alternative techniques include exchanging the tracheal tube for an LMA, or use of a remifentanil infusion.
Extubation should be preceded by suction to the pharynx and larynx, preferably under direct vision, to remove secretions and blood that might otherwise be inhaled. Secretions are particularly marked in unpremedicated patients and following neostigmine. Inflation of the lungs with O2 immediately before and during extubation provides an O2 reserve in case of laryngospasm and helps expel sputum from the upper airway. Facilities for reintubation should be available.
In patients in whom reintubation is predicted to be difficult, a bougie, fibrescope or airway exchange catheter may be placed into the trachea before extubation. In this group of patients high-dose corticosteroids may be considered to prevent post-extubation laryngeal oedema. After extubation, adequate ventilation should be confirmed and supplemental oxygen administered during transfer to a recovery room.
Similar considerations apply to patients in ICU after successful weaning from ventilators.
Popat M, Mitchell V, Dravid R, et al (2012). Anaesthesia; 67: 318–40
Eye, anatomy, see Cranial nerves; Orbit; Skull
 inhalational agents may be irritant to the cornea.
inhalational agents may be irritant to the cornea.
 lasers are increasingly used in surgery, especially around the head and neck.
lasers are increasingly used in surgery, especially around the head and neck.
Paraffin-based ointments reduce the incidence of abrasions but may impair vision for up to several hours. Methylcellulose or saline drops may also be efficacious but require regular administration (e.g. hourly). Routine taping of the eyes is the simplest method of preventing corneal abrasions.
Suresh P, Mercieca F, Morton A, Tullo AB (2000). Intensive Care Med; 26: 162–6
Eye, penetrating injury. Anaesthetic considerations:
 as for any intraocular ophthalmic surgery.
as for any intraocular ophthalmic surgery.
 risk of expulsion of intraocular contents should intraocular pressure (IOP) rise.
risk of expulsion of intraocular contents should intraocular pressure (IOP) rise.
 may present as an acute emergency following trauma, for eye or other surgery, i.e. with risk of aspiration of gastric contents.
may present as an acute emergency following trauma, for eye or other surgery, i.e. with risk of aspiration of gastric contents.
– general assessment, particularly of airway and risk of difficult intubation.
– delaying surgery should be considered if possible, to allow gastric emptying. Risk of aspiration pneumonitis may be reduced by metoclopramide, H2 receptor antagonists, etc.
 perioperatively: choice to be made, if surgery cannot wait:
perioperatively: choice to be made, if surgery cannot wait:
– to risk the rise in IOP caused by suxamethonium whilst performing rapid sequence induction. Risks may be reduced by:
– methods used to reduce the rise in IOP, although not always reliable:
– ‘generous’ dose of induction agent, or a supplementary dose before intubation, especially using propofol.
– iv β-adrenergic receptor antagonists, lidocaine, opioids, acetazolamide, and non-depolarising neuromuscular blocking drug pretreatment have been studied, with mixed results.
– rapid sequence induction using high-dose rocuronium.
– inhalational induction/awake intubation: however, coughing and straining increase IOP.
– the above may be combined with measures to reduce risk from aspiration.
The individual patient’s medical condition and severity of injury, and the skill of the anaesthetist, should be carefully considered before deciding on the most appropriate technique. Ultimately, safe tracheal intubation must take precedence over protection of the eye. Other drugs known to increase IOP, e.g. ketamine, should be avoided.