Dynamic function tests
On subsequent pages, individual DFT procedures are discussed in the context of specific hormonal axes. Here, we describe the principles that underpin some of these DFTs, and look at aspects of interpretation. The abbreviations used for the various hormones and the tests are listed in Tables 41.1 and 41.2 respectively.
Table 41.1
Abbreviations for some hormones
| Adrenocorticotrophic hormone | ACTH |
| Arginine vasopressin | AVP |
| Corticotrophin releasing hormone | CRH |
| Follicle stimulating hormone | FSH |
| Gonadotrophin releasing hormone | GnRH |
| Growth hormone | GH (or HGH) |
| Growth hormone releasing hormone | GHRH |
| Luteinizing hormone | LH |
| Parathyroid hormone | PTH |
| Thyroid stimulating hormone | TSH |
| Thyrotrophin releasing hormone | TRH |
| Thyroxine | T4 |
| Triiodothyronine | T3 |
Table 41.2
Commonly used abbreviations for various dynamic function tests
| IST | Insulin stress test |
| OGTT | Oral glucose tolerance test |
| SST | Short Synacthen test |
| DST | Dexamethasone suppression test |
| CAPFT | Combined anterior pituitary function test |
Insulin stress test
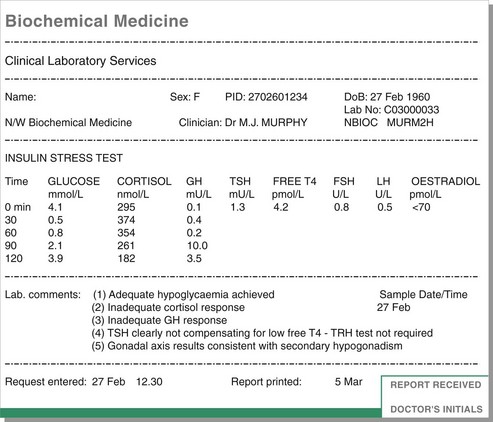
This test is carried out when hypopituitarism is suspected. It is also known as the insulin tolerance test. Enough insulin is administered to produce hypoglycaemic stress (blood glucose <2.2 mmol/L). This tests the ability of the anterior pituitary to produce ACTH and GH in response. Cortisol is measured instead of ACTH; this assumes that the adrenals can respond normally to ACTH. A peak GH in excess of 6 µg/L is regarded as evidence of adequate reserve. For cortisol there is less consensus about what should be regarded as an adequate response; however, anything less than 500 nmol/L is inadequate, and many endocrinologists use cut-offs substantially in excess of this, e.g. 550 nmol/L. An example of the results of an insulin stress test is shown in Figure 41.1.
TRH test
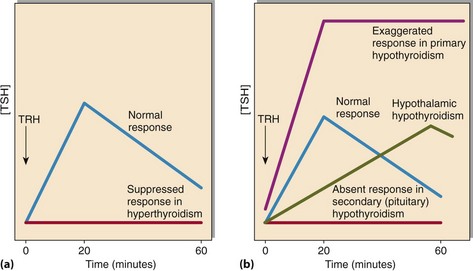
TRH is given as an intravenous bolus; blood sampling is at 0, 20 and 60 minutes (Fig 41.2). In normal subjects TRH elicits a brisk release of both TSH and prolactin. This test may be used to assess the adequacy of anterior pituitary reserve, or to evaluate suspected hypothalamic disease, in which the TSH response to TRH is characteristically delayed (TSH higher at 60 minutes than at 20 minutes). Much less frequently it may be indicated in suspected hyper- or hypothyroidism or subclinical thyroid disease. Where there has been prolonged negative feedback due to hyperthyroidism, the pituitary response to TRH is flat (TSH rises by <2 mU/L); conversely, an exaggerated TSH response (>25 mU/L) is seen in hypothyroidism.
GnRH test
In normal adults, GnRH produces a marked rise in LH and a smaller rise in FSH; typical expected increments in adults are >15 U/L for LH and >2 U/L for FSH. In children the FSH response is greater than the LH response. This test is indicated where there is clinical or biochemical evidence of hypogonadism, particularly in the absence of the expected compensatory rises in LH and FSH. It may be performed alone or as part of a combined anterior pituitary function test (see p. 85). The latter simply consists of the three separate DFTs described above (IST, TRH test and GnRH test) performed simultaneously. Collectively they provide a comprehensive assessment of anterior pituitary reserve.
Synacthen tests
The short Synacthen test (SST) is one of the most commonly performed DFTs. The procedure is described on page 97. Of the three criteria that are used to define a normal response (see Fig. 48.3 on p. 97), the final cortisol is the most important, and the increment the least important. As with the IST, there is lack of agreement on what constitutes an adequate cortisol response to Synacthen; cut-offs for the final level vary between 500 and 580 nmol/L.
Dexamethasone suppression tests
High dose dexamethasone suppression test
Failure to suppress in response to low dose dexamethasone may occur because of autonomous ACTH production by the pituitary (Cushing’s disease), or ectopic ACTH production (usually malignant), or adrenal production of cortisol (see p. 98). The high dose DST (8 mg) is used to distinguish the first two of these options. ACTH production in Cushing’s disease does usually suppress in response to high dose dexamethasone, whereas malignant production of ACTH usually does not.
Dynamic function tests – protocol variation
Protocols for individual DFTs vary from one centre to another. For example, an additional cortisol specimen is collected at 60 minutes in some SST protocols, although this rarely alters the interpretation of the SST. Likewise, the long Synacthen test may be performed as a day-long procedure, with 1 mg Synacthen administered in the morning and cortisol samples collected for up to 24 hours; others perform this test as outlined on p. 97. The reasons for the different protocols are often practical rather than evidence-based but it is always wise to check with the local laboratory before proceeding with any DFT.