CHAPTER 15 Duodenal Obstruction
Step 1: Surgical Anatomy
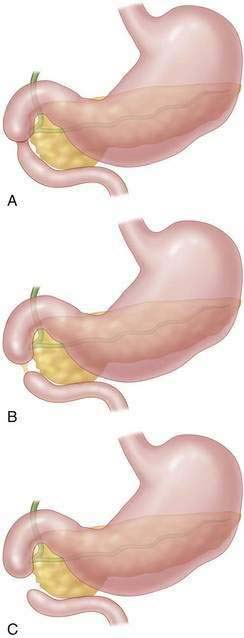
♦ In congenital duodenal atresia, the obstruction is distal to the ampulla of Vater in 85% of patients. A complete obstruction may be a luminal web (most common), an atresia connected by a fibrous cord, or complete separation of proximal and distal segments (Fig. 15-1).
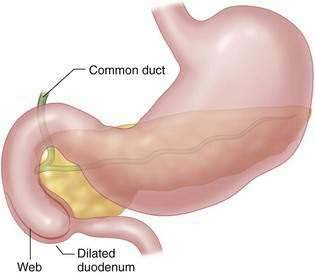
♦ The ampulla is located close to the medial wall of the web, and care must be taken to avoid injuring it during repair.
♦ A fenestrated duodenal web with incomplete obstruction may not be noted at birth but can be seen later with feeding intolerance or obstruction when solid foods are started.
Step 2: Preoperative Considerations
♦ The differential diagnosis includes malrotation with volvulus, small bowel atresia, and Hirschsprung disease in patients with bilious vomiting. In patients with nonbilious emesis, the differential includes pyloric atresia and antral web.
Step 3: Operative Steps
♦ Open and laparoscopic techniques are described, and both achieve the same anatomic result. The patient is positioned in the supine position for both approaches.
♦ The objective of surgery in most cases is to bypass the obstruction rather than resect it, thus avoiding injury to the ampulla of Vater or annular pancreas.
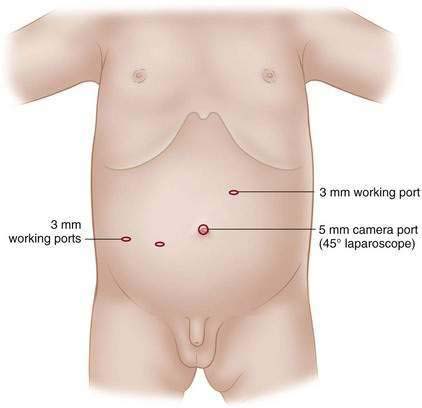
♦ Open surgery is done through a right-sided transverse supraumbilical incision. Trocar placement for the laparoscopic approach is shown in Fig. 15-4.
♦ The hepatic flexure is mobilized, and the duodenum is Kocherized to provide exposure to the first, second, and third portion of the duodenum.
♦ The level of obstruction is identified by transition from the dilated proximal segment to the collapsed unused distal bowel. If an annular pancreas is present, the level of obstruction is beneath the gland and bypass is performed from the bowel proximal and distal to the pancreatic tissue.
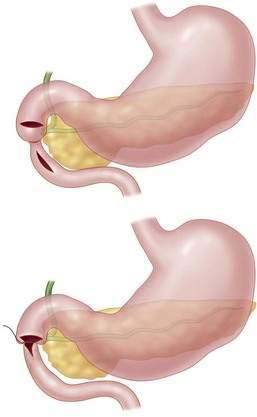
♦ After placing traction sutures, a transverse duodenotomy is made on the anti-mesenteric portion of the dilated proximal duodenum and a longitudinal incision on the anti-mesenteric border of the distal duodenum (Fig. 15-5).
♦ Prior to anastomosis the distal bowel is cannulated with an 8-10 French catheter and saline infused and followed to the ileocecal valve to rule out a distal obstruction.
Step 4: Postoperative Care
♦ Patients are extubated in the operating room unless co-morbidities such as cardiac anomalies require continued ventilatory support.
Step 5: Pearls and Pitfalls
♦ The level of obstruction may be obscured by a “windsock” deformity that results in dilation of the duodenum distal to the obstruction.
♦ In some cases the lateral portion of the web can be resected to relieve the obstruction without injury to the ampulla if it is clearly visualized.
♦ If the ampulla is distal to the obstruction (15%) and close to the duodenotomy, care must be taken to avoid common duct ligation or injury when placing the posterior row of duodenoduodenostomy sutures.
♦ A transanastomotic feeding tube may facilitate faster initiation of post-operative enteral feedings (Fig. 15-7).
♦ Patients with significant co-morbidities may benefit from gastrostomy tube placement in anticipation of poor oral feeding.
♦ Minimize bag-mask ventilation or nasal continuous positive airway pressure, which may disrupt the anastomosis in the early postoperative period.
Escobar MA, Ladd AP, Grosfeld JL, et al. Duodenal atresia and stenosis: long-term follow-up over 30 years. J Pediatr Surg. 2004;39:867-871. discussion 867-871
Naik-Mathuria B, Olutoye OO. Foregut abnormalities. Surg Clin North Am. 2006;86:261-284.
Spilde TL, St Peter SD, Keckler SJ, et al. Open vs laparoscopic repair of congenital duodenal obstructions: a concurrent series. J Pediatr Surg. 2008;43:1002-1005.