Duct Excision
Preoperative Workup
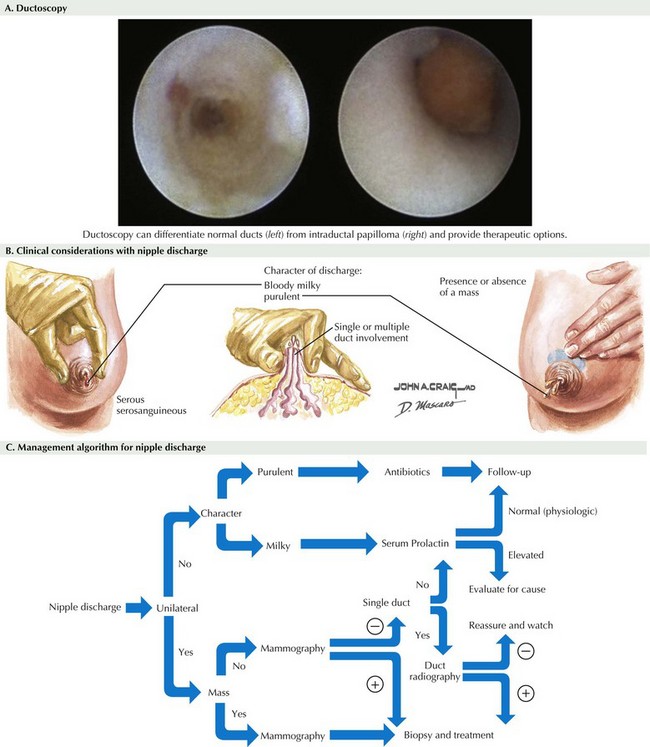
Diagnostic mammography is currently the test of choice in the workup of PND and is generally indicated in all patients. Ultrasound, magnetic resonance imaging (MRI), and ductography are being studied for prediction of malignant disease in PND, although no consensus exists on their use. Also under investigation is ductoscopy, real-time endoscopic imaging of the ductal system. Ductoscopy can differentiate normal ducts from intraductal papilloma and provide therapeutic options (Fig. 47-1, A). Although great advances have been made in the equipment and success of ductoscopy, its use is still limited to specialized centers.
There are several algorithms for the workup of PND, but the most important aspect of the evaluation is to prove that the discharge is not caused by a malignancy (Fig. 47-1, B and C). This often requires surgical resection and pathologic examination of the duct.
Surgical Principles
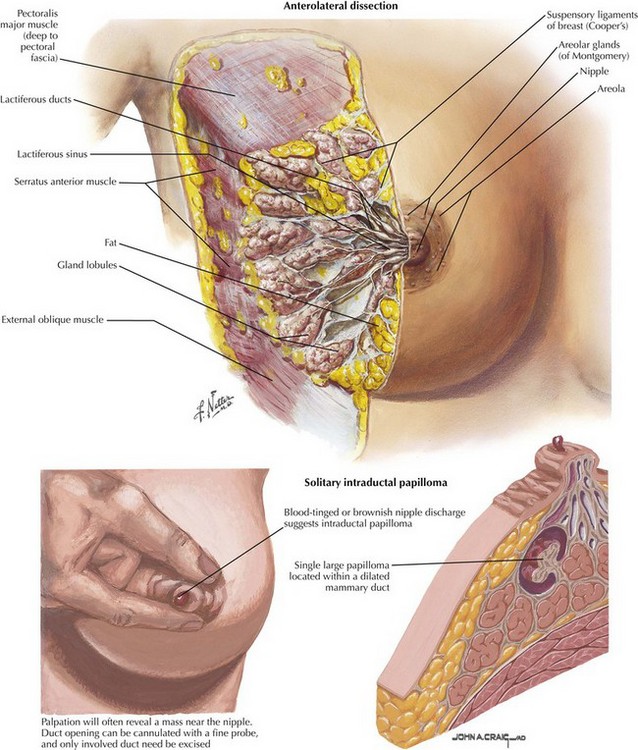
Duct anatomy is complex, and therefore an attempt should be made to identify the duct from which there is pathologic discharge. Several methods are used to achieve this. First, the nipple can be expressed in the operating room and the draining duct cannulated with a lacrimal probe (Fig. 47-2). Another method is to inject methylene blue preoperatively to guide the dissection of the correct duct. Some authors suggest preoperative ductography to distend the duct of interest and determine the distance needed to dissect from the ductal orifice to the lesion. Some centers equipped with ductoscopy can attempt to visualize and remove the lesion endoscopically; if this is not successful, a standard duct excision is done.
Excision Technique
A cone of tissue surrounding the duct of interest is dissected down to the gland lobule (Fig. 47-2). After the duct and surrounding tissue are removed, the remaining defect can be closed with absorbable suture. Before closing the skin, the nipple should be checked to ensure it is everted. If not, a subcutaneous stitch can be placed to evert the nipple.
Dietz, JR, Crowe, JP, Grundfest, S, Arrigain, S, Kim, JA. Directed duct excision by using mammary ductoscopy in patients with pathologic nipple discharge. Surgery. 2002;132(4):582–587.
Hussain, AN, Policarpio, C, Vincent, MT. Evaluating nipple discharge. Obstet Gynecol Surv. 2006;61(4):278–283.
Kuerer, HM. Kuerer’s breast surgical oncology. New York: McGraw-Hill Medical; 2010.
Louie, LD, Crowe, JP, Dawson, AE, et al. Identification of breast cancer in patients with pathologic nipple discharge: does ductoscopy predict malignancy? Am J Surg. 2006;192(4):530–533.
Mokbel, K, Escobar, PF, Matsunaga, T. Mammary ductoscopy: current status and future prospects. Eur J Surg Oncol. 2005;31(1):3–8.