Chapter 14 Drug eruptions
Key Points: Drug Eruptions
Table 14-1. Drugs Most Likely to Produce a Cutaneous Reaction
| DRUG | REACTIONS PER 1000 PATIENTS |
|---|---|
| Amoxicillin | 51.4 |
| Trimethoprim-sulfamethoxazole | 47 |
| Ampicillin | 42 |
| Ipodate sodium | 27.8 |
| Whole blood | 28 |
| Cephalosporins | 13 |

Figure 14-3. Classic lesions of erythema multiforme secondary to co-trimoxazole, demonstrating targetoid appearance.
(Courtesy of James E. Fitzpatrick, MD.)
Mathelier-Fusade P: Drug-induced urticarias, Clin Rev Allergy Immunol 30:19–23, 2006.
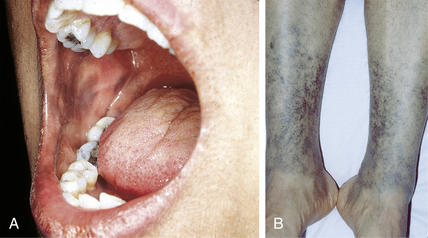
Table 14-2. Drugs Producing Changes in Skin Pigmentation
| COLOR | DRUG |
|---|---|
| Slate-gray | Chloroquine Hydroxychloroquine (see Fig. 14-5A) Minocycline (see Fig. 14-5B) Phenothiazines |
| Slate-blue | Amiodarone |
| Blue-gray | Gold (chrysoderma) |
| Yellow | Beta-carotene Quinacrine |
| Red | Clofazimine |
| Brown (hyperpigmentation) | Adrenocorticotropic hormone (ACTH) Bleomycin Oral contraceptives Zidovudine |
High HA, Ayers RA, Cowper SE: Gadolinium is quantifiable within the tissue of patients with nephrogenic systemic fibrosis, J Am Acad Dermatol 56:710–712, 2007.

Figure 14-8. Demeclocycline-induced phototoxic reaction on the dorsum of the hands.
(Courtesy of James E. Fitzpatrick, MD.)