Drowning and Cold-Water Immersion
Drowning: respiratory impairment from submersion or immersion in liquid
Fatal drowning: drowning that results in death
Nonfatal drowning: drowning injury that does not result in death (avoid historical terms such as near drowning and wet or dry drowning)
Immersion: body entry into a liquid medium
Submersion: entry into a liquid medium where the body—particularly the head—is below the surface
Cold-Water Immersion
1. The cold shock response is the most common cause of drowning in cold water.
2. Immediately on immersion, uncontrollable gasping lasts 1 to 3 minutes, which results in aspiration of water unless the head is kept above surface.
3. Sudden skin cooling results in increased peripheral vascular resistance of superficial blood vessels.
4. Heart rate and cardiac output increase; outpouring of catecholamines may lead to fatal dysrhythmias.
5. Cooling of the periphery decreases nerve conduction, and muscle control becomes difficult, making self-rescue virtually impossible.
6. Priority for self-rescue is to maintain the head above water, assuming the heat escape lessening position (HELP) (Fig. 50-1) if possible.
7. If two or more persons are in the water, the huddle position (Fig. 50-2) is recommended to lessen total body heat loss.

FIGURE 50-2 Huddle technique. (Courtesy Alan Steinman, MD.)
8. Because children become hypothermic much more quickly than do adults, they should be placed in the middle of the huddle.
9. Drawstrings should be tightened in clothing to decrease the flow of cold water within clothing layers.
10. In cold water a person may consider whether to stay in place to conserve heat or swim to safety. Note that at 45 to 90 minutes, swim failure may occur as a result of continued reduction of core body temperature causing loss of gross motor function. The average person can swim approximately 800 m (2625 feet) in 10° C (50° F) water while wearing a personal flotation device before swim failure and death occur.
On-Scene Rescue and Patient Management
1. Safety devices should be used to tow the patient, or life preservers should be thrown to people in trouble in the water before a human responder enters the water.
2. Anticipate cervical spine fracture or a significant head injury if trauma (for example, diving or fall) is suspected.
3. Evaluate for hypoglycemia (with or without diabetes), seizure disorder, and acute myocardial infarction as potential causes of drowning.
4. Initiate resuscitation (see later).
5. If rapid extrication from water is not feasible, institute in-water rescue breathing and maintain the patient in a vertical position to minimize the potential for vomiting and further aspiration of water and emesis (Fig. 50-3).
6. After the patient is out of the water, initiate basic life support.
7. Use ABC (airway, breathing, and circulation) rather than CAB sequence, because cardiac arrest in drowning is almost always due to hypoxia.
8. Begin with five rescue breaths, then follow routine basic life support procedures with 30 compressions to 2 ventilations.
9. Cardiopulmonary resuscitation (CPR) with compressions only is not recommended in drowning.
10. Emesis is common during drowning resuscitation; do not attempt to expel water by abdominal thrust or head-down position, which only increase emesis and interfere with adequate ventilation.
11. If the patient is breathing but unconscious, use the recovery position.
12. Transport to an emergency facility with ongoing CPR unless resuscitation is determined futile (see later) or successful.
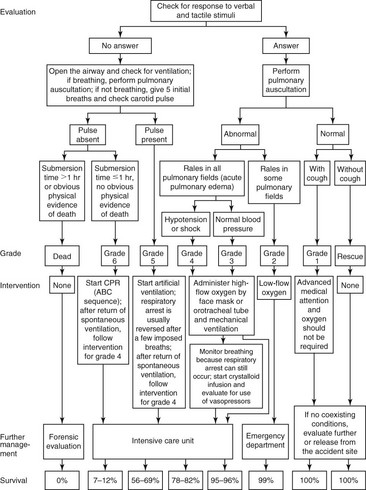
Drowning Classifications and General Treatment
The Symptomatic Patient: Grades 2, 3, and 4
Protection of the airway to ensure oxygenation and ventilation is the first priority. Maintaining perfusion to reverse the metabolic consequences of acidosis is a close second. The airway should be protected from aspiration by placing the patient in a lateral recumbent (i.e., recovery) position if possible. Vomiting is common with submersion incidents, and aspiration can worsen lung injury. Measures should be taken to prevent hypothermia and shivering. Rescuers must maintain vigilance and treat cardiac dysrhythmias that may arise as a result of hypoxemia. The management actions listed in Table 50-1 can then be considered. If cervical spine injury is suspected, use an extrication collar and an immobilization device. Routine cervical spine immobilization is unnecessary and should be reserved for patients with a known or suspected significant mechanism of injury.
Table 50-1
Prehospital Management and Classification of Drowning Patients
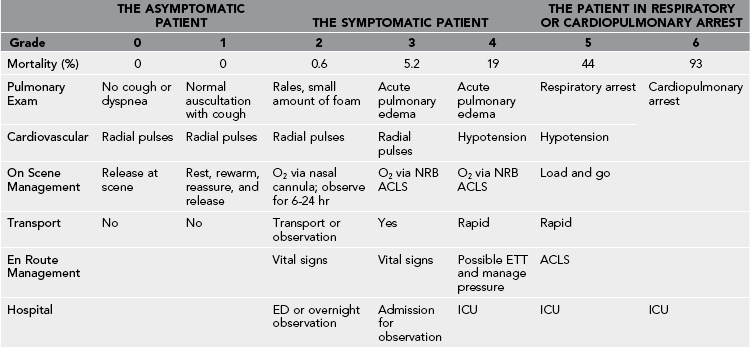
Courtesy Justin Sempsrott, MD. Modified from Szpilman D: Near-drowning and drowning classification: A proposal to stratify mortality based on the analysis of 1831 cases, Chest 112:660, 1997.
The Patient in Respiratory or Cardiopulmonary Arrest: Grades 5 and 6
Initiation of immediate ventilatory support and early CPR, if indicated, results in a better prognosis and outcomes. Initiation of chest compressions while the patient remains in the water is ineffective, delays extrication, and may further endanger the patient and rescuer. Alternatively, rescue breathing should be initiated as soon as the subject’s airway can be opened, even if in the water (see Fig. 50-3).
Should vomiting occur, roll the patient onto his or her side or turn his or her head to the side and remove the vomitus with a cloth or finger-sweep maneuver. If spinal injury is of concern, the patient should be logrolled, maintaining linear alignment of the head, neck, and torso. Because most beaches, riverbanks, boat ramps, and other waterway access points are sloped, patients should be placed perpendicular to the incline so that head and feet are level. When the subject is out of the water and airway and breathing are addressed, the presence or absence of adequate circulation should be ascertained. In cases of hypothermia or hypotension a pulse may be difficult to identify. If ventilation or cardiac function is impaired, chest compressions should be initiated as soon as the patient is removed from the water. For patients who are more than 1 year old, an automated external defibrillator may be used to evaluate heart rhythm. If the field rescue team is capable of advanced life support, cardiac monitoring, and intravenous or intraosseous access, fluids and medications should be administered according to advanced life support protocols. Basic life support or advanced cardiac life support should continue until the patient’s core body temperature is more than 30° C (86° F). See Table 50-1 for a classification scheme for drowning field assessment and management.
Prognosis and Termination of Resuscitation
Factors known to be useful for predicting outcomes in drowning are listed in Box 50-1. In the absence of profound hypothermia, the neurologic status of a patient on admission to the emergency department is of paramount importance for predicting survival with intact neurologic function. Persons who are alert when admitted seldom die.