CHAPTER 25 Double-Bundle Posterior Cruciate Ligament Reconstruction
Injuries to the posterior cruciate ligament (PCL), although infrequent, often present as complex problems that can result in severe disability because of the relationship between posterior instability and rotatory instability, combined with other ligamentous injury and cartilage degeneration. It is rare that PCL injuries occur in isolation; they frequently present in conjunction with anterior cruciate ligament (ACL) or posterolateral corner injuries.1 Both the rare isolated and concomitant PCL lesions are often misdiagnosed or overlooked altogether because PCL-specific symptoms can be difficult to distinguish or can be confounding when presenting with additional injuries.2
Joint function impairment in PCL-deficient knees correlates positively with chronicity.3–6 A PCL failure over time imposes additional medial compartment forces, resulting in increased pain and joint effusion. Functional limitations become increasingly frequent, especially with coexisting ligament injuries.7,8 Better understanding of PCL biomechanics has led to improvements in clinical evaluation and resulted in earlier recognition of PCL insufficiency. With earlier diagnoses and improvements in PCL reconstruction techniques, surgical indications for this type of injury have expanded markedly.9–13
ANATOMY
Anatomic descriptions of the PCL vary by degree of detail. The ligament is commonly described as consisting of two fiber bundles, the anterolateral (AL) and posteromedial (PM), with each defined by their relative femorotibial insertion sites, respectively. The anterior section comprises the bulk of the fibers, with the cross-sectional mass almost four times larger than the posterior section. The AL bundle is taut in flexion and becomes lax when approaching extension, whereas the significantly smaller PM bundle is tight in extension (Figs. 25-1 and 25-2) and relaxes toward flexion.14
In close conjunction with the PCL, two meniscofemoral ligaments can be present in some knees. Although their presence can vary, their attachments are uniform. Both ligaments attach distally to the posteromedial aspect of the lateral meniscus. The anterior meniscofemoral ligament (ligament of Humphry) passes diagonally anterior to the PCL and inserts on the lateral aspect of the medial femoral condyle in the roof of the intercondylar notch. The posterior meniscofemoral ligament (ligament of Wrisberg) passes at almost the same angle posterior to the PCL to the femur, blending with the attachment of the posterior longitudinal group of PCL fibers. Literature reviews15–17 have shown that Humphry ligaments are present alone in 25% to 38%, Wrisberg ligaments present alone 39% to 50%, both present in 17% to 20%, and neither in 3% to 8% of knees. Both meniscofemoral ligaments have roles as secondary restraints to posterior tibial translation, which has been noted subsequent to complete transection of the PCL.18,19 With their cross-sectional area at about 10 mm2 and each ligament comprising an estimated 22% of the PCL cross section, the extent of any ligament function potential will vary by the comparative size of the PCL and the presence or absence of either meniscofemoral ligament.
Functional Biomechanics
When the knee is flexed and approaches 45 degrees, the AL bundle fibers tighten and are aligned to resist posterior tibial force. In contrast, the PM bundles exhibit reciprocal behavior, are tight in extension and, when the knee is flexed, begin to slacken. The angle of the PM bundle is not suitable to resist posterior tibial force while tight during knee extension and only provides secondary restraint to resist hyperextension. Once flexion meets or exceeds 120 degrees, the PM bundle femoral attachment moves anteriorly in relation to the tibia so that it is tight and aligned to resist posterior tibial forces, which illustrates its function in deep knee flexion. As complete knee flexion is approached, the AL fibers wrap against the intercondylar notch roof, becoming almost vertical to the tibial plateau, and are thus poorly aligned to control posterior tibial translation. In the presence of collateral ligament and posterolateral corner pathology, PCL injuries have additional rotatory laxity, valgus instability, and posterior tibial translation.20,21
PATIENT EVALUATION
Clinical Assessment
Note that some normal laxity is seen in patients with physiologic genu recurvatum. If posterior translation is normal at 90 degrees but slightly increased at 30 degrees, a PLC injury is likely. Not all patients with PCL tears have a positive posterior drawer test on physical examination.22 Although the PCL is commonly evaluated by performing the posterior drawer test at 90 degrees,23–26 it can also be assessed by other methods, including the dynamic posterior shift test,27 the quadriceps active test, the posterior sag sign, the prone posterior drawer test, and the reverse pivot-shift test.28 Using the quadriceps active test in the presence of a PCL tear, the active contraction of the quadriceps muscle with the knee from 60 to 90 degrees of flexion produces anterior tibial movement and a posterior tibial sag is eliminated.
Diagnostic Imaging
To characterize PCL injury by magnetic resonance imaging (MRI), three planes should be used—axial, coronal, and sagittal. The use of a dedicated knee coil improves signal-to-noise ratio and a small field of view (10 to 14 cm) helps improve spatial resolution.29 The most sensitive views for evaluating the PCL are obtained with the sagittal oblique plane. With MRI, evaluations of PCL tears can be delineated into intrasubstance, partial, complete, or avulsion. Hemorrhage and edema are evident interstitially in intrasubstance tears. Partial tears are evident by interruption of a portion of one of the margins of the ligament and may present a circumferential ring of hemorrhage or edema (halo sign) around the margins. Complete tears have portions of the ligament that are completely absent and may include hemorrhage and edema blurring the margins or in focal areas in lieu of the ligament at tibial or femoral attachments. Avulsions are usually at the tibial insertion and the PCL will retract away with its bone fragment.
Isolated Posterior Cruciate Ligament Injuries
When isolated PLC injury occurs, the following conditions are typically found:
TREATMENT
Conservative Management
In the past, it was assumed that patients with an isolated PCL rupture did well with nonoperative treatment.30,31 Shelbourne and colleagues32 have studied chronic PCL injury nonoperated patients; 170 patients were untreated for their grade II or lower acute isolated PCL injuries. They stated that “…their conditions didn’t deteriorate over time as a group.” However, 20% reported giving way with activities of daily living, 26% reported giving way with strenuous activity, and 54% reported that they did not experience any instability. It is important to note that isolated PCL grade II or lower injuries are atypical. Nonoperative management for isolated PCL injuries (rarely occurring) is not a standard that should be applied universally to multiple ligament injuries.
Arthroscopic Technique
Most single-strand techniques attempt to reconstruct the larger anterolateral bundle.33,34 The posteromedial bundle, and the stability it provides in extension, is ignored. Double-bundle techniques have arisen in an attempt to address both the anterolateral and posteromedial bundles.35–37 In vitro research36,38 has suggested that these double-bundle reconstructions can eliminate joint laxity in flexion and extension.
Graft Preparation
Prepare a double-bundle Achilles tendon allograft at a side table. Divide the tendinous portion of the graft into two 7- × 250-mm bundles. Place a 5-cm long series of whipstitches at the end of each bundle to provide for advancement of the graft. The bony portion of the graft is typically trimmed to a length of 25 mm and sized to fit a 12-mm tunnel. Once trimmed, attach a wire suture to the bone plug to allow for positioning and tensioning (Fig. 25-3).
Portal Establishment and Posterior Cruciate Ligament Resection
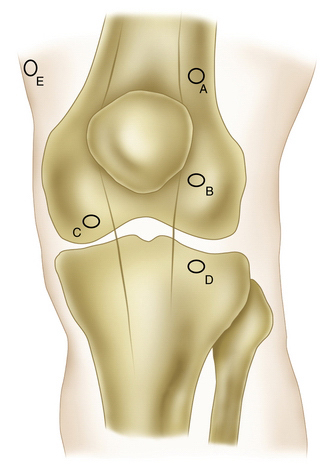
Establish standard anteromedial, proximal anterolateral, and midanterolateral arthroscopic portals initially. The distolateral and posteromedial arthroscopic portals are added later (Fig. 25-4). The midanterolateral portal must be placed sufficiently proximal and near the patella to allow for arthroscope access to the posterior medial compartment. Improper placement of this portal will also interfere with arthroscope placement while drilling the femoral tunnels through the distolateral portal.
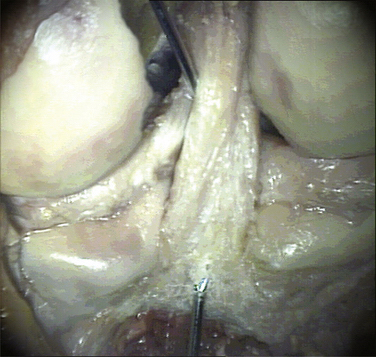
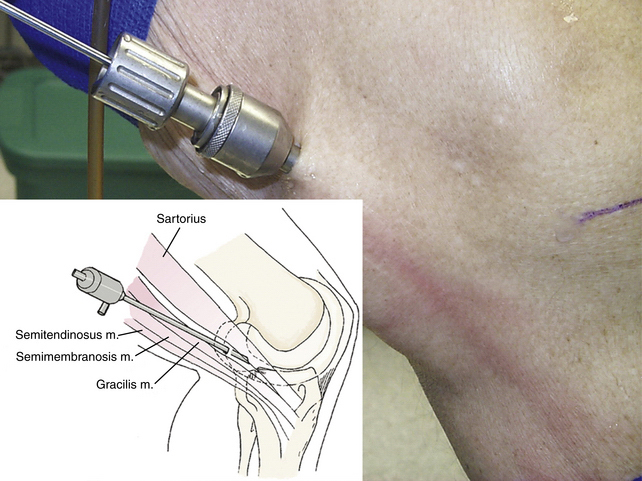
Resect the torn PCL using an arthroscopic shaver. Then position the posteromedial portal approximately 13 to 15 cm proximally to the joint line and anterior to the hamstring tendons at the posterior margin of the vastus medialis muscle. From this position, direct the portal toward the tibial PCL attachment (Fig. 25-5). Begin by inserting a spinal needle, observing its position with the arthroscope. Once positioned properly, follow the needle with a scalpel to make space for switching stick insertion. Place a 10-mm cannula over the switching stick through the posteromedial portal. This portal provides access to the PCL tibial fovea for the arthroscope or rotary shaver, as required. Place the shaver through the posteromedial portal and débride the stump of the PCL.
Drill the Tibial Tunnel
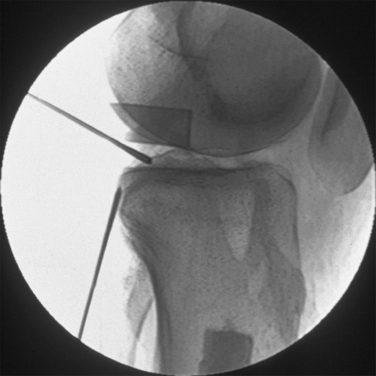
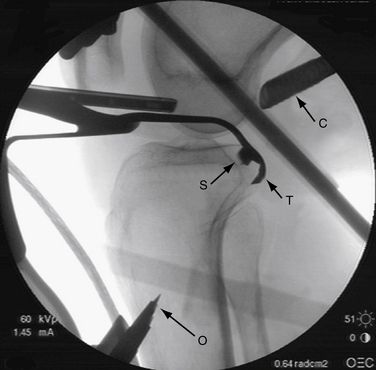
Make a 2.5-cm vertical incision 1 cm medially and 3 to 4 cm distally to the crest of the tibial tubercle and extend it distally (Fig. 25-6). Use the Tundra PCL drill guide (Smith & Nephew) to place the tibial tunnel. With the Tundra guide body and PCL arm assembly adjusted to the closed (smallest angle) setting, insert the drill guide through the anteromedial portal and direct it to the anatomic insertion of the PCL on the posterior tibia. Once in this position, readjust the arm to a larger angle setting to achieve the maximum possible between the 54- and 57-degree marks on the arm. Position the distal end of the drill guide over the medial tibial incision and lock it firmly in place by adjusting the force on the outriggers. Using fluoroscopic visualization, verify the correct guide position (Fig. 25-7). Advance the trephine until it exits through the tibia posteriorly and contacts the backsplash (Fig. 25-8).

FIGURE 25-6 A vertical incision provides access for the distal tibial tunnel (T). The proximal point is positioned 1 cm medially and 3 to 4 cm distally to the crest of the tibial tubercle and extended distally. This incision, and the tunnel placed through it, are sufficiently distal to permit another incision placed more proximally to accommodate an ACL reconstruction. Note that the midanterolateral portal (B) must be placed sufficiently proximal and near the patella to allow for proper access. Improper placement of this portal will cause problems with arthroscope access to the posteromedial compartment and will also interfere with femoral tunnel drilling through distolateral portal.
Drill the Femoral Tunnels
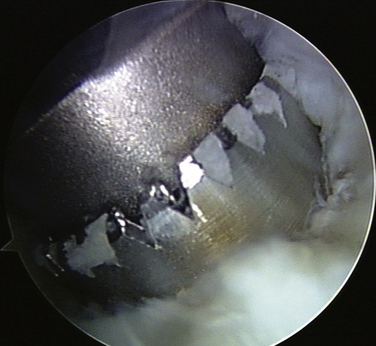
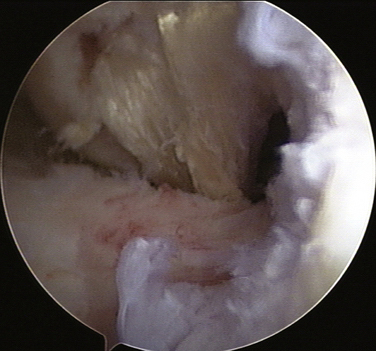
Flex the knee to 90 degrees. Débride the femoral stump and use its margins as a reference for Beath pin placement. Approach through the distolateral portal and place two chisel-point, slot-eyed Beath pins near the distal and proximal margins of the femoral footprint of the PCL (posterior and anterior margins when the knee is extended; Fig. 25-9). The slot in the eye of the pins permit graft suture placement without threading sutures through the eyelet. Direct the pins proximally and medially so that they exit the thigh medially, approximately 7 to 10 cm proximal to the joint line. Advance a cannulated 7-mm trephine over the previously placed slot-eyed pins. Beginning with the posterior tunnel (for the PM tendon bundle), drill it through the medial femoral cortex. Use the grasper to hold the slot-eyed pin in place while backing out the trephine. Repeat the procedure for the anterior femoral tunnel (for the AL tendon bundle), leaving both pins in place.
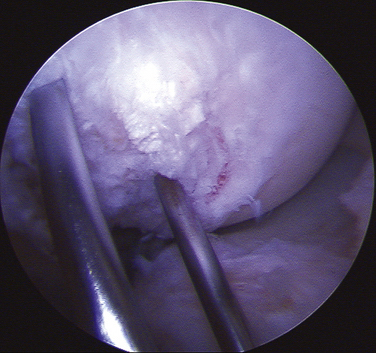
FIGURE 25-9 The lateral aspect of the medial femoral condyle with both slot-eyed Beath pins inserted into their anterior and posterior positions within the femoral footprint is shown. The pins are placed at least 4 mm from the medial femoral condyle articular margins so that the 7-mm tunnels drilled over them are close to the articular margins without encroaching into the articular cartilage.
Graft Insertion and Fixation
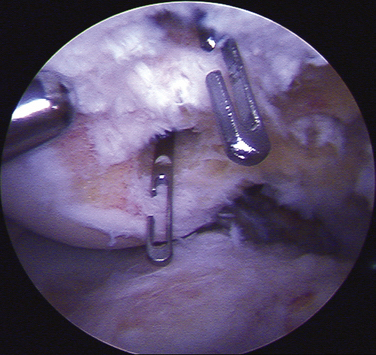
Advance each pin until its slotted eye is drawn into the joint space and protrudes slightly from its respective femoral tunnel (Fig. 25-10). Reposition the graspers flush with the skin to prevent the slot-eyed pins from shifting or falling out while the sutures are threaded. Débride the soft tissue from the orifice of each tunnel. Orient the graft so that the tendinous side of the bone block is posterior, with one bundle exiting medially and one bundle laterally. Pass the PM tendon bundle sutures into the tibial tunnel with a grasper and transfer them to a ringed grasper just proximal to the posterior tunnel aperture (Fig. 25-11). Draw the sutures anterior with the ring grasper and remove the ring grasper out of the anteromedial portal. Using a grasper, insert it into the anteromedial portal, grasp the sutures, and lay them into the slot eye of the Beath pin (Fig. 25-12). Advance the pin to bring the sutures medially to exit the skin and release the sutures being held with the tibial tunnel grasper to allow tension to be applied to the graft (Fig. 25-13). Transfer the Kocher clamp from the pin to the tensioned sutures. Repeat the process with anterolateral bundle sutures to the slot-eyed pin in the anterior femoral tunnel until they exit the skin medially; transfer the Kocher clamp from that pin to those sutures.
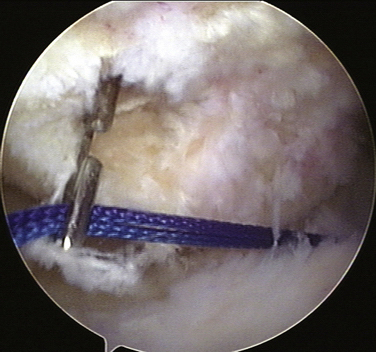
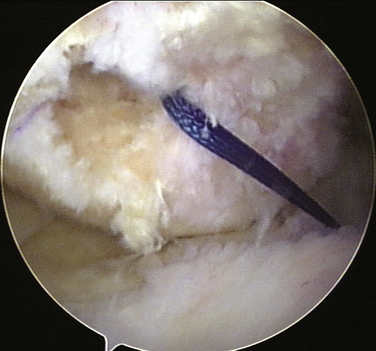
FIGURE 25-12 The posteromedial tendon bundle sutures are both laid into the slot of the slot-eyed Beath pin.
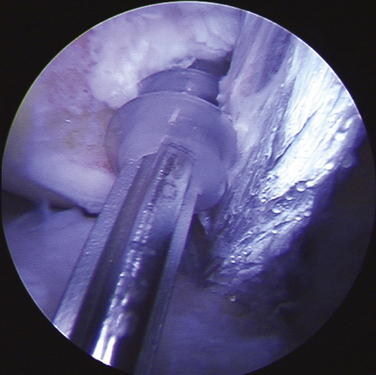
Advance the tendinous portion of the Achilles allograft through the tibial tunnel simultaneously (Fig. 25-14). Apply tension on the tendon bundle sutures. Avoid advancing either bundle significantly further than the other (Fig. 25-15). Adjust the distal-proximal position of the graft so that the proximal end of the bone block is flush with the posterior aperture of the tibial tunnel. Advance a guide wire anteriorly within the tibial tunnel, positioning it between the cancellous side of the bone block and tibial tunnel wall. Advance a 7- × 25-mm cannulated bioabsorbable screw along the guide wire until the screw makes solid purchase with the bone block and tibial tunnel wall (Fig. 25-16). This maneuver can be fluoroscopically monitored.
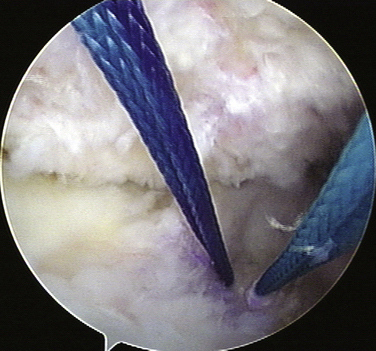
FIGURE 25-14 Shown is a posterior view of the two graft bundles and their passing sutures. Proper sizing permits light tension to draw the graft bundles to exit the tibial tunnel posteriorly and be drawn over the “killer turn” and across the knee compartment into place. The sutures on the posteromedial bundle have been colored dark blue for identification.
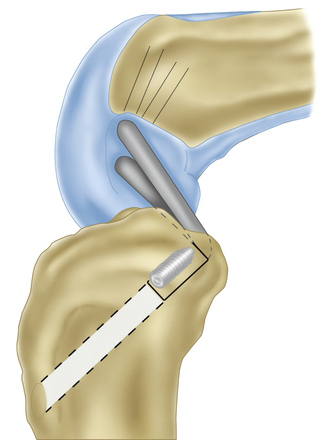
FIGURE 25-16 The 7- × 25-mm HCIS is in position with the bone plug and screw at the posterior aperture of the tibial tunnel.
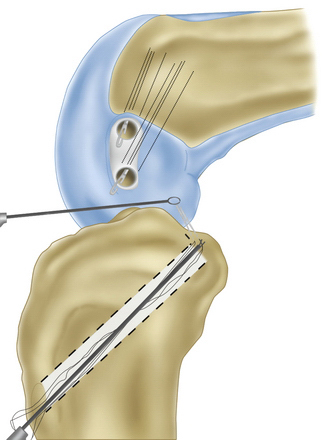
Manipulate the knee vigorously and apply anterior force to the tibia, with traction maintained on both bundles. The PM bundle is tensioned and secured with interference screw fixation near extension, typically in 20 degrees of flexion (Fig. 25-17). Direct a guide wire through the distal anterolateral portal and position it anterior to the bundle in the distal femoral tunnel. With traction applied to the PM bundle located in the posterior femoral tunnel, advance a 7- × 25-mm cannulated bioabsorbable screw over the guide wire through the distal anterolateral portal alongside the graft until it is seated completely within the tunnel, thereby providing direct tendon to bone fixation. The AL bundle, located in the anterior femoral tunnel, is tensioned and secured in 90 degrees of flexion. Fixation is accomplished with a 7- × 25-mm cannulated bioabsorbable screw also directed through the distal anterolateral portal over its respective guide wire.
PEARLS& PITFALLS
1. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11:526-529.
2. Pearsall AW, Hollis JM. The effect of posterior cruciate ligament injury and reconstruction on meniscal strain. Am J Sports Med. 2004;32:1675-1680.
3. Parolie JM, Bergefd JA. Long-term of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35-38.
4. Logan M, Willians A, Lavelle J, et al. The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med. 2004;32:1915-1922.
5. Clancy WG. Repair and reconstruction of the posterior cruciate ligament. In: Chapman M, editor. Operative Orthopedics. Philadelphia: JB Lippincott; 1998:1651-1665.
6. Hughston JC, Bowden JA, Andrews JR, Norwood LA. Acute tears of the posterior cruciate ligament: results of operative treatment. J Bone Joint Surg Am. 1980;62:438-450.
7. Clancy W, Shelbourne D, Zoellinger G. Treatment of knee joint instability secondary to rupture of posterior cruciate ligament. J Bone Joint Surg Am. 1983;65:310-322.
8. Keller PM, Shelbourne KD, McCarroll JR, Retting AC. Non-operatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 2004;12:420-428.
9. Dandy D;Pusey R. The long-term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg Am. 1982;64:92-94.
10. Covey DC, Sapega AA, Marshall RC. The effects of varied joint motion and loading conditions on posterior cruciate ligament fiber length behavior. Am J Sports Med. 2004;32:1866-1872.
11. Park SE, Stamos BD, DeFrate LE, et al. The effect of posterior knee capsolotomy on posterior tibial translation during posterior cruciate ligament tibial inlay reconstruction. Am J Sports Med. 2004;32:1514-1519.
12. Chen CH, Chou SW, Chen WJ, Shih CH. Fixation strength of three different grafts used in posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:371-375.
13. Zaffagnini S, Martelli S, Garcia L, Visani A. Computer analysis of PCL during range of motion. Knee Surg Sports Traumatol Arthrosc. 2004;12:420-428.
14. Amis AA. Anatomy and biomechanics of the posterior cruciate ligment. Sports Med Arthrosc Rev. 1999;7:225-234.
15. Makris CA, Georgoulis AD, Papageordiou, et al. Posterior cruciate ligament architecture: Evaluation under microsurgical dissection. Arthroscopy. 2000;16:627-632.
16. Heller L, Langman J. The menisco-femoral ligaments of the human knee. J Bone Joint Surg Br. 1964;46:307-313.
17. Yamamoto M, Hinohara K. Anatomical study on the meniscofemoral ligaments of the knee. Kobe J Med Sci. 1991;37:209-226.
18. Gergis FG, Marshall JL, Monajem ARS. The cruciate ligaments of the knee joint. Anatomical functional and experimental analysis. Clin Orthop Relat Res. 1975;(106):216-231.
19. Harner JD, Höher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26:471-482.
20. Nielsen S, Helmig. The static stabilizing function of the popliteal tendon in the knee. An experimental study. Arch Orthop Trauma Surg. 1986;104:357-362.
21. Nielsen S, Ovesen J, Rasmussen O. The posterior cruciate ligament and rotatory knee instability. An experimental study. Arch Orthop Trauma Surg. 1985;104:53-56.
22. Hughston JC. The absent posterior drawer test in some acute posterior cruciate ligament tears of the knee. Am J Sports Med. 1988;16:39-43.
23. Noyes FR, Stowers SF, Grood ES, et al. Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro sectioning study in cadaveric knees. Am J Sports Med. 1993;21:407-414.
24. Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233-242.
25. Grood E, Stowers S, Noyes F. Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70:88-97.
26. Henry MH, Berend ME, Feagin JAJr. Clinical diagnosis of acute knee ligament injuries. Ann Chir Gynaecol. 1991;80:120-126.
27. Covey DC, Sapega AA, Sherman GM. Testing for isometry during reconstruction of the posterior cruciate ligament. Anatomic and biomechanical considerations. Am J Sports Med. 1996;24:740-746.
28. Jakob RP, Hassler H, Stäubli HU. Observations on rotatory instability of the lateral compartment of the knee: experimental studies on the functional anatomy and pathomechanism of the true and reverse pivot shift sign. Acta Orthop Scand Suppl. 1981;191:1-32.
29. Grover JS, Bassett LW, Gross ML, et al. Posterior cruciate ligament: MRI imaging. Radiology. 1990;174:527-530.
30. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35-38.
31. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989;(133):208-216.
32. Shelbourne KD, O’Shea JJ, Patel DV. The natural history of nonoperatively treated posterior cruciate ligament injuries. Am J Sports Med. 1999;27:276-283.
33. Furie E. Risk factors of arthroscopic popliteal artery laceration. Arthroscopy. 1995;11:324-327.
34. Veltri DM, Warren RF, Silver G. Complications in posterior cruciate ligament surgery. Oper Tech Sports Med. 1993;1:154-158.
35. Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy. 1995;11:69-76.
36. Border PS, Nyland JA, Caborn DNM. Posterior cruciate ligament reconstruction (double bundle) using anterior tibialis tendon allograft. Arthroscopy. 2001;17:e14.
37. Campbell RB, Jordan SS, Sekiya JK. Arthroscopic tibial inlay for posterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1356.
38. Chen CH, Chen WJ, Shih CH. Arthroscopic double-bundled posterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy. 2000;16:780-782.