Theories and concepts in the composition of Chinese herbal formulas
Chinese herbs are not used singly in treatment, but in combinations known as herbal formulas. This is because herbal combinations have several advantages compared to the use of single herbs. First of all, herbal combinations may have wider applications than single herbs. For instance, when pathogenic heat accumulates in the Lung and Stomach, and the Qi of these two organs is deficient, a single herb can hardly treat this syndrome completely whereas a herbal combination can achieve an effective therapeutic result. Second, a herbal combination can reduce the side effects of individual herbs. Each single herb has its specific characteristics, which bring a unique effect to treatment, but these characteristics may also become a weak point. For example, Shu Di Huang ( Rehmanniae radix praeparata) is an excellent herb to tonify the blood and Kidney-essence but its cloying nature places an extra burden on the Stomach, which may impair its tonifying action. However, if it is used with Sha Ren ( Amomi xanthioidis fructus), which promotes Qi movement and removes any accumulation of dampness, this side effect can be reduced. Third, a herbal combination can have a much stronger effect than that of individual herbs, and may even induce a new effect. For example, Huang Qi ( Astragali radix) is able to tonify and raise the Spleen-Qi and increase muscular strength. Chai Hu ( Bupleuri radix) and Sheng Ma ( Cimicifugae rhizoma) have an ascending property but neither of them can tonify the Qi nor strengthen muscular contraction. However, if these three herbs are used together, the effect of raising the Qi and strengthening muscular contraction becomes much stronger. This combination can be used to treat weakness, heaviness of muscles and prolapse of internal organs due to Spleen-Qi deficiency.
1. Common types of herbal combination
Since a herbal combination has obvious advantages in treatment, the relationships between the herbs used in traditional Chinese medicine (TCM) have been carefully studied and certain types of relationship are identified. They are called the seven relations between herbs, e.g. mutual accentuation, mutual enhancement, mutual counteraction, mutual suppression, mutual antagonism, mutual incompatibility and single effect. Some of these are very useful in treatment, but some are harmful and therefore must be avoided.
1.1. Mutual accentuation (Xiang Xu  )
)
In this type of combination, two herbs with similar functions are used together to increase the therapeutic effect, achieving a safer and more effective therapeutic result than the use of a larger dosage of a single herb. For instance, Jing Jie ( Schizonepetae herba) and Fang Feng ( Saposhnikoviae radix) can expel wind and release the exterior much more strongly when they are used together. Jin Yin Hua ( Lonicerae flos) and Lian Qiao ( Forsythiae fructus) can more effectively reduce heat-toxin if they are used together. Da Huang ( Rhei rhizoma) and Mang Xiao ( Natrii sulfas) can promote bowel movement to treat severe constipation more effectively and safely than the use of Da Huang ( Rhei rhizoma) alone.
1.2. Mutual enhancement (Xiang She  )
)
This type of combination involves two herbs that have different functions. The first directly targets the pathological condition and the second increases the therapeutic effect of the first. For instance, Zhi Mu ( Anemarrhenae rhizoma) nourishes the Yin of the Kidney and clears heat in the Lower-Jiao, while Huang Bai ( Phellodendri cortex) reduces empty-heat in the Lower-Jiao and is therefore able to enhance Zhi Mu’s function of nourishing the Yin.
In addition, this type of combination is widely used to correct the side effects of a particular herb, to prolong the action of a herb in a steady way, to moderate the movement of Qi and to harmonize the internal organs. In this type of combination, the first herb treats the main disorder and its dosage and function are larger and stronger than those of the second herb. The second herb serves to reduce the side effects and to moderate the speed and the temperature of the first. For example, sweet Zhi Gan Cao ( Glycyrrhizae radix preparata) can moderate the speed of hot Fu Zi ( Aconiti radix lateralis preparata)* and can also reduce the harsh purging effect of Da Huang ( Rhei rhizoma).
Moreover, some special strategies have been developed from this type of combination to achieve efficient therapeutic effects. For example, upward-moving and downward-moving herbs, and dispersing and restraining herbs may be used at the same time. The first herb treats the disorder and the second herb, which has different or opposite properties, directional tendency and functions, serves as its assistant. In this way, it keeps the action of the first herb steady and moderate. For instance, when the aim of treatment is to strengthen the exterior, the sweet and warm Huang Qi ( Astragali radix) is used to tonify and stabilize the Defensive-Qi. It is combined with a small amount of Fang Feng ( Saposhnikoviae radix), which is pungent and warm, and which is used to disperse wind from the exterior, thereby ensuring that Huang Qi does not trap the wind in the superficial region of the body. Fang Feng thus enables Huang Qi to achieve the desired therapeutic outcome without any side effects.
Another example is when one wants to strengthen the Heart-Qi and treat restlessness and palpitations. Here Ren Shen ( Ginseng radix) is often selected as it directly tonifies Heart-Qi. Ren Shen is combined with a small amount of Wu Wei Zi ( Schisandrae fructus) which is very sour and has a stabilizing and binding ability. It can stabilize the Heart-Qi which Ren Shen generates. Moreover, when the Heart-Qi is weak, it may find it hard to accept strong tonifying action and Ren Shen used on its own may lead to restlessness and palpitations at the start of treatment and may further consume Heart-Qi. In this condition, Wu Wei Zi can reduce the harsh effects of Ren Shen and make its action more moderate and longer lasting.
There are many examples that illustrate the benefits of this type of herbal combination. Huang Lian ( Coptidis rhizoma) descends and clears fire from the Stomach, but it may also suppress Stomach-Qi and cause discomfort in the Stomach. If Sheng Ma ( Cimicifugae rhizoma) is prescribed at the same time, it can ascend and disperse the Stomach-Qi constraint and Stomach-fire, thereby reducing the side effects of Huang Lian.
1.3. Mutual counteraction (Xiang Wei  )
)
In this combination, the characteristic side effects or toxicity of a single herb can be minimized or neutralized by another. This combination strategy is often used when processing harsh and toxic herbs. For example, the toxic effects of Ban Xia ( Pinelliae rhizoma) can be reduced by Sheng Jiang ( Zingiberis rhizoma recens).
1.4. Mutual suppression (Xiang Sha  )
)
In this type of combination, the first herb suppresses or minimizes the toxicity of the second herb. For instance, Lü Dou ( Phaseoli radiati semen) can reduce the toxicity of Ba Dou ( Crotonis fructus)*, while Ge Hua ( Puerariae flos) can reduce the toxic effects of alcohol.
1.5. Mutual antagonism (Xiang Wu  )
)
In this type of combination, some herbs can reduce the therapeutic effect of others. For instance, Lai Fu Zi ( Raphani semen) can reduce the ability of Ren Shen ( Ginseng radix) to tonify the Qi. This type of herbal combination and effect should be avoided in treatment. The Chinese medical tradition has identified 18 antagonistic substances:
• Liu Huang ( Sulfur)* antagonizes Po Xiao ( Glauberis sal)
• Shui Yin ( Hydrargyrum)* antagonizes Pi Shuang ( Arsenicum)*
• Lang Du ( Euphorbiae Fischerianae radix)* antagonizes Mi Tuo Seng ( Lithargyrum)*
• Ba Dou ( Crotonis fructus)* antagonizes Qian Niu Zi ( Pharbitidis semen)*
• Wu Tou ( Aconiti radix)* antagonizes Xi Jiao ( Rhinoceri cornu)**
• Ya Xiao ( Nitrum) antagonizes San Leng ( Sparganii rhizoma)
• Ding Xiang ( Caryophylli flos) antagonizes Yu Jin ( Curcumae radix)
• Ren Shen ( Ginseng radix) antagonizes Wu Ling Zhi ( Trogopterori faeces)
• Rou Gui ( Cinnamomi cassiae cortex) antagonizes Chi Shi Zhi ( Halloysitum rubrum).
1.6. Mutual incompatibility (Xiang Fan  )
)
In this type of relationship, as soon as the two herbs are used together, a dangerous effect can arise so the use of this type of combination is absolutely forbidden. Traditionally there are 19 substances involved:
• Wu Tou ( Aconiti radix)* is incompatible with Chuan Bei Mu ( Fritillariae cirrhosae bulbus), Gua Lou ( Trichosanthis fructus), Ban Xia ( Pinelliae rhizoma), Bai Lian ( Ampelopsitis radix) and Bai Ji ( Bletillae tuber)**
• Li Lu ( Veratri nigri radix et rhizoma) is incompatible with Ren Shen ( Ginseng radix), Sha Shen – Bei Sha Shen ( Glehniae radix)/Nan Sha Shen ( Adenophorae radix), Ku Shen ( Sophorae flavescentis radix), Xuan Shen ( Scrophulariae radix), Dan Shen ( Salviae miltiorrhizae radix), Xi Xin ( Asari herba)*, Shao Yao – Chi Shao Yao ( Paeoniae radix rubra)/Bai Shao Yao ( Paeoniae radix lactiflora).
1.7. Single effect (Dan Xing  )
)
This is a special pattern in herbal relationships. Some herbs can be used alone to treat a simple syndrome or to achieve special effects based on their characteristics. Some herbs can be used alone because they have reasonably balanced properties and functions. For instance, in critical conditions, Ren Shen ( Ginseng radix) can be used on its own in a large dosage to rescue the Yang and Qi from collapse. Dan Shen ( Salviae miltiorrhizae radix), which can cool the blood, clear heat and promote blood circulation, is often used alone in conditions where heat is consuming the Yin and blood, leading to blood stagnation. Dang Gui ( Angelicae sinensis radix) can also be used alone as it has a moderate action in promoting blood circulation and tonifying the blood.
Of the above seven types of relationship, those of mutual accentuation and mutual enhancement are commonly used in treatment; mutual counteraction and mutual suppression can also be used, especially to reduce herbs’ side effects or toxicity. The single herb effect is only used in a limited number of disorders; relations of mutual antagonism and mutual incompatibility should be avoided in treatment.
In addition to these relationships, there is another kind of relationship between herbs in treatment. In this type of combination, two herbs work as one unit although they have different properties and functions, and in this case they are equally important. Together they treat a condition with which a single herb would not be able to deal. For example, to treat warm and cold coexisting in one syndrome, where Yang and Qi deficiency generate cold while stagnation of Qi generates heat, the patient may, on the one hand, have a cold, weak and sensitive Stomach and prefer warm drinks and compresses; on the other hand, the patient may have a dry mouth with a bitter taste and heartburn. In this situation, the pungent and warm Ban Xia ( Pinelliae rhizoma) which can disperse cold is used with the bitter and cold Huang Qin ( Scutellariae radix) which can reduce the accumulated heat. Without this combination, it is almost impossible to treat this syndrome effectively. Another example is when one needs to regulate the Lung-Qi, clear heat and relieve shortness of breath. The pungent and hot Ma Huang ( Ephedrae herba)* is used to stimulate the Yang and disperse the Lung Qi; the sweet and cold Shi Gao ( Gypsum) is used to descend the Lung-Qi and clear the heat of the Lung. This combination can regulate the Qi and smooth the breath.
(See Figure I.1 on page 34.)
2. The process of formula composition
With this knowledge of herbal combinations, a herbal formula can be composed. The purpose of prescribing formulas in clinical practice is to achieve maximum therapeutic effect with minimum side effects. To practice traditional Chinese herbal medicine, practitioners are required to be able to compose formulas by themselves for treating different syndromes.
Composing a formula is a process where several conditions must be fulfilled. First, one must make a clear syndrome differentiation, establish the treatment principles, select treatment methods and figure out the most suitable strategies. One should then follow the model of formula structure, selecting appropriate herbs to play specific roles in the formula and ensuring that treatment strategies are fully expressed.
2.1. Syndrome differentiation
Clear and correct syndrome differentiation is very important for selecting a suitable treatment method and creating an effective formula. Detailed differentiation of a syndrome should include the following parts.
Principal syndrome and main symptoms
The principal syndrome where the main pathological development is identified manifests through a series of main symptoms. For example, the main symptoms indicating an exterior wind-cold syndrome are chills and fever, headache and generalized body pain. These result from the invasion of wind and cold at the superficial region of the body, the failure of the Defensive-Qi to spread, and obstruction in the blood circulation.
Secondary syndrome and secondary symptoms
A secondary syndrome develops from the principal syndrome and manifests in a series of secondary symptoms. When the principal syndrome is treated, the secondary syndrome may disappear as well. For example, in an exterior wind-cold syndrome, since the superficial region is obstructed, the Lung-Qi is unable to disperse so the nose may be blocked and there may be shortness of breath. As soon as the wind-cold is expelled from the superficial region of the body, the Lung-Qi obstruction disappears and the secondary symptoms disappear too.
A secondary syndrome might be a coexisting syndrome that is less important at the time of treatment. For example, in an acute condition of Liver-Yang ascending and generating Liver-wind, the patient may also have a syndrome of Spleen-Qi deficiency but this is less important for treatment in this acute condition.
Secondary symptoms are accompanying symptoms that are not key symptoms in terms of syndrome identification but they should still be treated seriously. For example, in an exterior wind-heat syndrome, although cough is not as important a symptom as sore throat in terms of syndrome identification, it should still be treated as it causes suffering to the patient.
Tongue and pulse
These are essential diagnostic methods for syndrome identification as well as for giving a prognosis regarding the development of and recovery from the disease. A practitioner can obtain objective information from these diagnostic procedures.
2.2. The treatment principle
The treatment principle takes the main syndrome in a complex condition as the target for treatment. In the process of treatment, the syndrome will change and the treatment principle will thus change too. For instance, in a syndrome of Liver-Yang ascending and generating Liver-wind, the treatment principle should be to intensively and quickly descend Liver-Yang and extinguish Liver-wind. Once the Liver-Yang has returned to its original place and the Liver-wind has disappeared, a syndrome of deficiency of Spleen-Qi and stagnation of Liver-Qi may then become the main syndrome. The treatment principle should change to that of spreading the Liver-Qi and strengthening the Spleen.
2.3. The structure of a formula
Following the treatment principle, which is established in accordance with the syndrome differentiation, a formula can be composed. A formula is neither a group of herbs that treat all symptoms nor a combination that only treats the main syndrome. It has a structure where herbs are organized in order to meet the needs of the treatment. The structure of a formula contains four parts, namely: the chief, the deputy, the assistant(s) and the envoy. Each of these has specific functions in the formula.
Chief (Zhu  , Jun
, Jun  )
)
The chief is the ingredient that directly treats the principal syndrome, which is manifested by the main symptoms.
The chief can be one ingredient, but it can also be a herbal combination. Generally speaking, the chief has a relatively large dosage within the formula as a whole, and it enters the meridians where the pathological changes are manifest.
Deputy (Fu  , Chen
, Chen  )
)
• The deputy is the ingredient that has the function of accentuating and enhancing the effect of the chief ingredient to treat the principal syndrome.
• The deputy serves as the main ingredient acting directly against a coexisting syndrome.
The deputy can be one herb, a herbal combination, or several groups of herbal combinations, according to the needs of treating the principal syndrome and the coexisting syndromes.
Assistant (Zuo  )
)
• The assistant accentuates and enhances the therapeutic effect of the chief or deputy ingredients, or directly treats secondary symptoms. The ingredient that has this function can be considered a helping assistant.
• The assistant moderates or eliminates the toxicity or harsh properties of the chief or deputy ingredients. The ingredient that has this function can be considered a corrective assistant.
• The assistant has a function or a moving tendency which goes against the chief ingredient but which is helpful in fulfilling the therapeutic effect and which may be used in complicated and serious conditions. The ingredient that has this function can be considered a strategic assistant.
Since this role may require a range of actions, there are often several herbs or herbal combinations acting as assistants in any one herbal formula.
Envoy (Shi  )
)
The envoy serves as a guide to bring the rest of the herbs into the meridian or region where the main pathological change exists, allowing their actions to focus on this specific region. In most cases, the chief carries out this function as it must enter the place where the pathological change is located.
The envoy harmonizes and integrates the actions of the other ingredients in order to balance the action, temperature, speed and direction of the formula.
(See Figure I.2 on page 34.)
2.4. Principles, methods and strategies of selecting appropriate herbs when composing a formula
In order to compose effective formulas, the principles, methods and strategies of selecting herbs are very important. They enable a practitioner to compose formulas to treat a variety of syndromes. The principles, methods and strategies introduced in each chapter of this book are abstracted from a large number of formulas, integrating the knowledge of single herbs, herbal combinations, syndrome differentiation, treatment methods and treatment sequence. They are the essential part of this book.
Before composing a formula, the relevant syndrome is first identified. The syndrome is analyzed and divided into the principal syndrome and the secondary syndrome, which are manifested in the main symptoms and the secondary symptoms, with specific signs on the tongue and the pulse. These are the first steps in selecting the appropriate herbs to fulfill different roles in the formula. Moreover, the syndrome analysis evaluates the development of the disorder of the internal organs with regard to the pathological change. This provides another clue to assist the selection of the herbs in the formula. For instance, if Liver-Qi stagnation is diagnosed, it follows that the Liver can easily attack the Spleen, so in the formula some herbs that strengthen the Spleen should be prescribed. Similarly, if the patient has a Yang constitution, the stagnation of Liver-Qi can quickly generate Liver-fire, so some herbs that prevent the generation of fire or prevent the heat becoming strong should be added as well. In a condition of excess heat in the Lung, one should be aware that strong fire can easily consume both the Yin and the Qi, so one should not only prescribe herbs to reduce fire, but also herbs that nourish the Yin and tonify the Qi.
Next, an appropriate treatment principle to treat the presenting syndrome is established. For example, to treat an excess heat syndrome in the Lung, the treatment principle is to reduce the heat, nourish the Yin, regulate the Lung-Qi and, at a later stage, strengthen the Lung-Qi.
As soon as a treatment principle is established, the composition plan and treatment strategies can be arranged. For instance, to treat the syndrome of excess heat in the Lung and Stomach, one would first prescribe herbs that have sweet-cold, bitter-cold or salty-cold properties, and which have the functions of clearing heat and reducing fire in the Lung and Stomach. Second, herbs that are sweet and cold and that can nourish body fluids and protect the Yin, which has been severely consumed by the excess heat, should be selected. Herbs that can tonify the Qi should be selected if the Qi is weakened severely by the heat. Herbs that moderate the actions of the harsh herbs in the formula, and reduce their side effects, should also be added.
The composition plan and the treatment strategies are effected by appropriate herbs, which are selected carefully according to their properties, functions and characteristics. Take again the treatment of excess heat in the Lung and Stomach as an example. Shi Gao ( Gypsum) is selected as the chief in the formula because it has cold, sweet and pungent properties, enters the Lung and Stomach meridians and can directly and intensively reduce excess heat in the Lung and Stomach. Zhi Mu ( Anemarrhenae rhizoma) is selected as deputy because it is moistening and cold. On the one hand it can accentuate the function of Shi Gao to reduce the excess heat; on the other hand it can nourish the Yin, which has been badly damaged by the heat, thereby directly treating the secondary syndrome. Gan Cao ( Glycyrrhizae radix) and Jing Mi (non-glutinous rice) are selected as assistants to tonify the Qi of the Spleen and to protect the Stomach from injury by the pathogenic heat and the bitter, cold and heavy herbs.
3. Dosages for individual herbs
3.1. Standard dosages for individual herbs
Generally speaking, the most common dosage for most crude herbs in Chinese texts is about 3–9 g orally per day. Modern concentrated herbal powder is six times stronger than crude herb, thus the common dosage for most single herbs is 0.5–1.5 g per day. According to my own experience, this dosage can be reduced to 0.2–0.5 g. A list specifying the dosages for individual herbs can be found in Appendix I.
3.2. Exceptions
Minerals
Minerals can be used at 30 g per day in traditional decoctions. Examples are Shi Gao ( Gypsum), Ci Shi ( Magnetitum), Long Gu ( Mastodi fossilium ossis), Mu Li ( Ostrea concha), Zhen Zhu Mu ( Concha margaritifera usta), Shi Jue Ming ( Haliotidis concha) and Wa Leng Zi ( Arcae concha). If concentrated powder is prescribed, the dosage should be about 1–2 g.
Lightweight herbs
Herbs that are light in weight should be prescribed at lower dosages, 0.5–3 g for crude herbs and 0.1–0.5 g for concentrated powders. Examples are Tong Cao ( Tetrapanacis medulla), Deng Xin Cao ( Junci medulla), Ma Bo ( Lasiosphaera) and Chan Tui ( Cicadae periostracum).
Poisonous herbs
Dosages for all poisonous herbs should be learned by heart. Since the toxic dose varies for each individual, the therapeutic range for these herbs is small and only experienced doctors should prescribe them.
Poisonous herbs in reasonably common use are Fu Zi ( Aconiti radix lateralis preparata)*, Wu Tou ( Aconiti radix)*, Xi Xin ( Asari herba)*, Ma Huang ( Ephedrae herba)*, Yang Jin Hua ( Daturae flos)*, Lei Gong Teng ( Tripterygii wilfordii caulis)*, Wu Gong ( Scolopendra)*, Quan Xie ( Scorpio)*, Bai Hua She ( Agkistrodon acutus)*, Mang Chong ( Tabanus)*, Zhe Chong ( Eupolyphaga seu opisthoplatia)*, Shan Dou Gen ( Sophorae tonkinensis radix)*, Ban Xia ( Pinelliae rhizoma), Tian Nan Xing ( Arisaematis rhizoma), Bai Fu Zi ( Typhonii rhizoma praeparatum)*, Wei Ling Xian ( Clematidis radix), Xian Mao ( Curculinginis rhizoma), Wu Zhu Yu ( Evodiae fructus), Hua Jiao ( Zanthoxyli fructus) and Yuan Zhi ( Polygalae radix).
Poisonous substances that are suitable for special pathological situations but which are rarely used are Ku Lian Pi ( Meliae cortex), He Shi ( Carpesii fructus), Gua Di ( Pedicellus cucumeris), Li Lu ( Veratri nigri radix et rhizoma), Chang Shan ( Dichroae febrifugae radix), Gan Sui ( Euphorbiae kansui radix)*, Da  ( Knoxiae radix)* Yuan Hua ( Genkwa flos)*, Shang Lu ( Phytolaccae radix), Qian Niu Zi ( Pharbitidis semen)*, Ba Dou ( Crotonis fructus)* and Zhu Sha ( Cinnabaris)*.
( Knoxiae radix)* Yuan Hua ( Genkwa flos)*, Shang Lu ( Phytolaccae radix), Qian Niu Zi ( Pharbitidis semen)*, Ba Dou ( Crotonis fructus)* and Zhu Sha ( Cinnabaris)*.
 ( Knoxiae radix)* Yuan Hua ( Genkwa flos)*, Shang Lu ( Phytolaccae radix), Qian Niu Zi ( Pharbitidis semen)*, Ba Dou ( Crotonis fructus)* and Zhu Sha ( Cinnabaris)*.
( Knoxiae radix)* Yuan Hua ( Genkwa flos)*, Shang Lu ( Phytolaccae radix), Qian Niu Zi ( Pharbitidis semen)*, Ba Dou ( Crotonis fructus)* and Zhu Sha ( Cinnabaris)*.3.3. Variations from the normal dosage range
Bland herbs, which promote urination and leach out dampness, can be used in relatively large doses; these include Fu Ling ( Poria), Yi Yi Ren ( Coicis semen) and Che Qian Zi ( Plantaginis semen).
Tonifying herbs can also be used in relatively large doses; these include Huang Qi ( Astragali radix), Shu Di Huang ( Rehmanniae radix praeparata), Mai Men Dong ( Ophiopogonis radix) and Bai He ( Lilii bulbus).
Aromatic herbs that open the orifices, expel wind-heat or wind-cold and promote Qi movement should be used in relatively small doses; these include Bing Pian ( Borneol), Su He Xiang ( Styrax), Bo He ( Menthae herba), Chai Hu ( Bupleuri radix), Xin Yi ( Magnoliae flos), Bai Zhi ( Angelicae dahuricae radix), Mu Xiang ( Aucklandiae radix)** and Sha Ren ( Amomi xanthioidis fructus).
Herbs that are used alone should be prescribed in relatively large doses; when they are prescribed as part of a formula, the dosage should be smaller.
4. Dosage in herbal formulas
4.1. General principles
The dosages of herbs in a formula should follow the standard dosages of the individual herbs. However, dosages may be varied within the normal dosage range according to the position each herb occupies in the formula. Generally speaking, a relatively large dose of the chief herb(s) should be prescribed, whereas envoy herbs should be given at small dosages. The dosages of the deputies and the assistants depend on their number and the strength of the functions required of them. In a small formula (i.e. one that contains less than five herbs), the dosages should be relatively large. In a medium-sized formula (containing 9–12 herbs), medium-sized dosages should be used. In a large formula (containing more than 20 herbs), the dosages should be low.
4.2. Adjusting dosage to reflect the presenting syndrome
The dosages of the individual herbs in a formula should be varied according to the presenting syndrome. For instance, the usual dosage for Chai Hu ( Bupleuri radix) is 6–9 g per day. It is pungent and neutral, and can effectively ascend and spread the Liver-Qi. It is very often used as the chief herb in formulas to treat Liver-Qi stagnation. However, in situations where Liver-Qi stagnation is accompanied by blood deficiency, a smaller dosage of Chai Hu (e.g. 6 g), should be prescribed to ensure that its Qi dispersing effect does not consume or weaken the blood. If the presenting condition features Liver-Qi stagnation with Spleen-Qi deficiency and an accumulation of dampness in the Upper- and Middle-Jiao, Chai Hu should be prescribed at a relatively large dosage, such as 9 g, because it needs more strength to disperse in order to overcome the dampness. In a case with Liver-Qi stagnation, Liver-Yin deficiency and Liver-Yang rising, Chai Hu should be prescribed at a very low dose, such as 3 g, or even removed from the formula altogether to prevent its ascending property from exacerbating the tendency of Liver-Yang to rise.
4.3. Adjusting dosage during the course of the treatment
When treating acute diseases, or the active stage of chronic diseases, the dosages of herbs in a formula should be large. When the disorder is under control, the dosages should be reduced. Formulas that open the orifices, induce sweating, vigorously purge accumulation by promoting bowel movement and induce vomiting are used only once. Afterwards, the dosage must be adjusted according to the patient’s condition. For instance, to treat severe constipation due to severe obstruction of food, Qi, blood and fire-toxin in the abdomen, a vigorously purging formula should be given to eliminate accumulation. But only a single dose should be given. If the condition of the patient does not improve and the syndrome remains the same, this formula should be given again. As soon as the patient has a bowel movement, use of the formula should cease, and a gentle formula to regulate the Qi, moisten the intestines and protect the Spleen should be prescribed.
Formulas that contain strong herbs to treat acute and excess syndromes should not be used at high dosages for more than 4 weeks. These include formulas that:
• disperse the Lung-Qi
• disperse wind, cold and dampness
• strongly reduce heat-toxin
• purge and drain downward
• break up Qi stagnation
• remove congealed blood
• remove food stagnation
• sedate the Heart-shen and descend the Liver-Yang.
In treating chronic diseases, or after intensive treatment for acute disorders lasting 1–4 weeks, the herbs in a formula should be prescribed at lower dosages. Herbs that tonify or harmonize the functions of the internal organs should be added.
Intensive treatment can be repeated, according to the disease and the patient’s condition.
Gentle tonifying herbs can be used for months or even years at low doses to keep the patient’s condition stable, to strengthen the body’s resistance and to maintain a good health.
It is good to have breaks in long-term treatment of chronic disorders. The best time to do this is in the summer because summer-heat or damp-heat may weaken the function of the Spleen at this time, and the herbs may overburden the Spleen and cause digestive disorders.
4.4. Adjusting dosage to take account of the patient’s constitution and diet
Relatively large dosages can be prescribed for young people, people with good constitutions and people in good physical condition when they suffer from acute excess syndromes. Small dosages are prescribed for elderly people, people with weak constitutions and people who suffer from chronic diseases.
Foodstuffs and drinks possess warm or cold properties which may influence the action of herbs. Generally speaking, coffee, spices, mutton, liver, fat, oil and nuts can easily generate heat. Most fruit, vegetables and cold beverages have a cold nature and can bring cold into the body. Milk products and fat may generate phlegm. This should be taken into consideration when prescribing the herbs in a formula.
4.5. Adjusting dosage according to the patient’s age
The elderly
In elderly people, the Qi, blood and essence are no longer strong, the movement of Qi and the circulation of blood are not smooth, the digestion of food and the metabolism of water become slow, and the mood is often unstable. Consequently, herbs should be prescribed with extra care.
• Herbs should be prescribed at lower dosages within the normal range.
• Gentle tonifying herbs can be used at low dosages for a long period of time to strengthen the body’s resistance or to maintain good health.
• Tonifying herbs should initially be prescribed at low dosages because their cloying nature may cause indigestion. If all is well, the dosages may be gradually increased.
• Herbs that promote digestion, calm the mind and spread the Liver-Qi should be used in chronic disorders and when the patient is recovering from disease.
Children
Children have special physiological and pathological characteristics. As their internal organs, muscles and bones are delicate and their physiological functions are not fully developed, children become ill more easily than adults, and their diseases develop quickly. Therefore, the proper formula with suitable dosages of herbs should be given at the appropriate time.
The common daily dosage of individual herbs for children is as follows:
• infant: 1/10 of the adult dosage
• infant–1 year old: 1/6 of the adult dosage
• 1–2 years old: 1/4 of the adult dosage
• 2–4 years old: 1/3 of the adult dosage
• 4–6 years old: 1/2 of the adult dosage
• 6–14 years old: 2/3 of the adult dosage.
Note
• The adult dosage referred to here is the average adult dosage.
• The dosage given is for children with a normal weight and height for their age.
• The dosage can be varied within the normal range according to the disease and the patient’s constitution as well as the experience of the practitioner.
Children who are thin and weak
• Herbs should be given in dosages at the lower end of the normal dose range.
• Gentle herbs that tonify the Spleen and Kidney can be used at low dosages for a long period of time to support the child’s development.
• Tonifying herbs should initially be given at low doses, and then gradually increased, because their cloying nature may cause indigestion. Herbs that promote digestion should be prescribed at the same time.
• Herbs that calm the mind and spread the Liver-Qi should be used when treating stressed and sensitive children.
Obese children
• Dosage should be at the upper end of the normal dose range for children. It should not be the same as the dosage for an adult with the same weight.
• Use herbs that reduce phlegm, food stagnation and dampness. Herbs that tonify the Qi and activate the Qi movement can be used if necessary.
• Sport and a healthy diet should be recommended as part of the treatment.
4.6. Adjusting dosage according to the season and climate
In addition to the nature of the presenting disorder and the patient’s constitution, seasonal and climatic factors should also be considered.
In summer or in places with a warm dry climate, pungent, warm and bitter herbs should not be used at high doses because the pores of the body are not tightly closed and so the body fluid can easily be consumed by heat. This precaution relates to herbs that induce sweating, expel wind and cold, disperse the Lung-Qi, dry dampness and increase urination.
In winter or in cold places, cold, bitter, sour and astringent herbs should be prescribed in a relatively low dose. This precaution relates to herbs that clear heat, cool blood and drain downward. In humid places, herbs that transform dampness, activate the Qi movement and promote digestion should be used in relatively large doses because the herbs need extra strength to overcome the dampness.
4.7. Adjusting dosage to reflect particular times in the patient’s life
At times of great stress and high emotion, or of severe physical exertion and tiredness, the body becomes more sensitive, and herbs should be prescribed at lower dosages than normal. For instance, to treat severe tiredness due to Spleen-Qi and Heart-blood deficiency, herbs that tonify the Qi and blood should be used in the formula but their doses should be very low because any strong stimulation and tonification may cause further disorder in the body. If the patient suffers from insomnia and anxiety, formulas that calm the mind and sedate the Heart-spirit should be used first. At the time of menstruation, or if the patient has a bleeding wound, or immediately after surgery, herbs that promote Qi and blood should be prescribed at low dosages. If the patient is breast-feeding, herbs that are very warm or cold or that have harsh properties should not be used or only prescribed in low doses.
4.8. Adjusting dosage in light of the patient’s medical history
The dosages prescribed should take proper account of the patient’s medical history.
When patients suffer from chronic liver or kidney disease, the selection of the herbs and their dosages should be determined carefully to avoid placing an unnecessary workload on these weakened organs. At the same time, herbs that protect these organs and promote their function should also be included. For instance, acute or chronic liver diseases are mainly differentiated into a syndrome consisting of Spleen-Qi deficiency, damp-heat and heat-toxin accumulation, and herbs that treat this syndrome can be used. Chronic kidney diseases are mainly differentiated as Kidney-Yang and Spleen-Yang deficiency, dampness accumulation and heat-toxin in the blood. Herbs that treat this syndrome should be used in appropriate doses to help restore kidney function.
If a patient has recently undergone surgery, the Qi and blood need time to get strong again, so pungent, very warm or very cold herbs should only be used in low doses.
In situations where western drugs are used together with herbs and have similar functions, such as inducing sweating, stimulating blood circulation, removing congealed blood, purging the intestines and sedating the mind, the dosage of the drug or the herbs should be reduced.
5. Form of administration, preparation methods and their applications
5.1. Decoctions
Preparation
Place the dry herbal ingredients in an earthenware or stainless steel pot and add cold water until the water level is 3–4 cm above the herbs. Leave the herbs to soak in the water for at least 1 hour. Place the pot on the cooker and apply strong heat to bring it to the boil. Once the liquid is boiling, turn the heat down, simmer the herbs for 20 minutes, and then strain the decoction from the pot into a receptacle.
Pour another 200 ml of cold water onto the herbs in the pot and cook for a further 20 minutes. Strain the resulting liquid into the receptacle holding the first decoction, thus mixing the two decoctions together. The total liquid obtained should be about 200–250 ml. (Herbs that expel wind-cold or wind-heat should be cooked for 10 minutes less and tonifying herbs should be cooked for 10 minutes longer each time.)
Finally, divide the decoction into two or three doses and take these over the course of the day, warming each dose before drinking it.
Special preparation procedures
Because some herbs have particular properties, special procedures are required for their preparation.
Decocting first: Some substances are heavy and do not readily release their active ingredients into the decoction. They therefore need to be cooked for 30 minutes before adding the other herbs. Most of these ingredients are mineral substances, such as Ci Shi ( Magnetitum), Long Gu ( Mastodi fossilium ossis), Mu Li ( Ostrea concha), Shi Jue Ming ( Haliotidis concha) and Shi Gao ( Gypsum). Some toxic herbs, such as Fu Zi ( Aconiti radix lateralis preparata)* and Wu Tou ( Aconiti radix)*, should also be cooked for longer to reduce their toxicity.
Decocting later: Some aromatic or pungent herbs have active ingredients that will be destroyed by long cooking and these should be added to the pot 5 minutes before the end of cooking. Examples are Bo He ( Menthae herba), Qing Hao ( Artemisiae annuae herba), Huo Xiang ( Agastachis herba) and Xiang Ru ( Moslae herba). Also, in order to increase certain actions, some herbs are cooked for less time than normal. For instance, Da Huang ( Rhei rhizoma) can be cooked for a shorter time to increase its purgative action.
Some rare, expensive herbs, such as Ren Shen ( Ginseng radix), should be prepared separately. Herbs that are traditionally used in powder form should be added to the prepared decoction without cooking; an example is San Qi ( Notoginseng radix) powder. Gels and syrups such as E Jiao ( Asini corii colla), Yi Tang ( Maltose), honey and egg yolks, should be dissolved in the prepared decoction without cooking.
Applications
Decoction is the most common form of administration of Chinese herbal medicine. Decoctions are usually taken orally. They can be absorbed quickly and have the strongest action of all of the traditional types of preparation.
Formulas can be varied according to clinical need. The decoction method is used particularly for serious and acute conditions. Decoctions can also be used topically as herbal baths for the whole body or for the affected regions of the body.
Decoctions do, however, have some obvious drawbacks. They need a reasonable amount of time to prepare, especially in chronic diseases; they do not always taste pleasant; they are not easy to transport or to store. Nowadays, some herbal pharmacies have made some improvements in this respect, offering to cook decoctions for their patients and delivering the herbal medicine in sealed vacuum-packed bags that may be stored in a refrigerator for a few days.
5.2. Powders
Preparation
The dry raw herbal ingredients are ground into coarse or fine powders. Coarsely ground powders can be prepared in the same way as decoctions, though they require a shorter cooking time. Finely ground powders can be prepared by simply adding boiling water at the time of administration. Some fine powders can be applied topically for skin disorders, muscle strains and wounds.
Applications
Powders can be used in small dosages. They are easy to prepare, administer, transport and store. Powders are less wasteful than decoctions. Their main drawback is that their action is not as strong as decoctions. They are often used for sub-acute, chronic and mild cases.
5.3. Pills
Preparation
The dry raw herbs are ground into powder and are mixed either with water or with a viscous medium and shaped into pills. These may be of different sizes, depending on the practitioner’s specification.
Applications
Generally speaking, pills are used for chronic conditions and for reasonably stable conditions where frequent changes of formula are unnecessary. Pills are convenient to use, transport and store. Moreover, ingredients that should not be cooked at high temperature (e.g. aromatic ingredients) can be prepared in this way. Since the weight of each pill is the same, the herbal dosage can be managed more easily by patients than when they are taking decoctions or powders. Furthermore, the pill form is an ideal solution for herbs that have a strong smell and/or an unpleasant taste, or which bring irritation to the stomach. Pills can reduce wastage compared with decoctions, especially for expensive and rare herbs. The disadvantage of pills is that, because their ingredients are fixed, they cannot readily be adjusted to match change in the presenting syndrome.
• Pills made with honey: Honey is often used as the binding agent when making pills. Its sweetness moderates the tastes of the herbal ingredients while also moderating and stabilizing the effects of the herbs in the formula. Pills made with honey are especially suitable for chronic conditions.
• Pills made with water, alcohol or vinegar: Pills made with water are easier to absorb than other types of pill because there is no viscous medium. They are small in size and are easy to swallow. As alcohol or vinegar brings a dispersing or softening action, pills made in this way are used for specific therapeutic purposes. Generally speaking, pills processed with alcohol may bring stronger and quicker therapeutic effects, while pills processed with vinegar guide the herbal ingredients specifically to enter the Liver meridian.
• Pills made with paste: Because the herbal ingredients are mixed with paste (made from rice or wheat flour), this type of pill is absorbed slowly and is especially suitable for ingredients that are toxic or have harsh actions which can easily irritate the stomach. This type of pill is also used for chronic conditions when gentle and steady effects are required.
5.4. Syrups
Preparation
Syrups are made by adding cane sugar to a liquid herbal decoction.
Applications
Sugar has moistening and tonifying properties. Herbal syrups are often used for mild cases, such as to moisten the Lung. Because they taste sweet, they are more readily accepted by patients, especially by children.
5.5. Herbal teas
Preparation
The dry raw herbs are cut into small pieces and made into a tea by infusing in boiling water. The herbal tea is drunk from time to time over the course of the day just like drinking normal tea.
Applications
Herbal teas are used for mild disorders such as the common cold, sore throat or indigestion.
5.6. Distilled medicinal liquids
Preparation
The distilled liquid is collected after the aromatic, fresh herbs are cooked.
Applications
Distilled medicinal liquids are light in smell, taste and function. Fresh herbs that clear heat and nourish the body fluids are often used in this form, especially in the summer.
5.7. Medicinal alcohol drinks
Preparation
The herbs are soaked in alcohol made from rice or sorghum for at least 1 month.
Applications
Since alcohol has dispersing and fast moving properties, it can increase the effect and speed of the herbs. Medicinal alcohol drink is often used for chronic disorders. Herbs that tonify the body, such as Ren Shen ( Ginseng radix) and Gou Qi Zi ( Lycii fructus), and herbs that disperse wind, damp and cold to treat Bi syndrome, such as Wu Jia Pi ( Acanthopanacis cortex), are often prepared in this way. Herbal alcohol drink is usually taken once a day in small amounts of 10–20 ml.
5.8. Special pills (Dan)
Preparation and application
Dan originally referred to the sublimated mineral ingredients containing mercury and sulfur for topical and oral use. Some expensive, concentrated and especially effective herbal pills made with paste for oral use may also be called Dan.
5.9. Injections
Preparation
These are made by extracting the active ingredients of herbs, and preparing and sterilizing them to modern pharmaceutical standards for subcutaneous, intramuscular or intravenous use.
Applications
Injections rely on small but precise doses of herbal extracts. They have rapid effects on the body and, unlike orally administered medicines, their therapeutic action is not dependent on the condition of the stomach and intestines.
5.10. Medicinal lotions and creams
Preparation
The herbal ingredients are ground into a fine powder and mixed with water, Vaseline or other media.
Applications
These are applied topically to the affected area and are often used for skin disorders, ulcers, infections and trauma. They work directly on the focus of the disease. They work constantly and are steadily absorbed by the body.
5.11. Plasters
Preparation
The herbal ingredients are cooked with water, strained and heated until a paste is formed. This paste is then smeared onto strips of plaster and stored ready for use when needed.
Applications
Plasters are applied topically to affected muscles and joints. Herbs that promote blood circulation, expel wind, dampness and cold to treat trauma and Bi syndrome are often prepared in this way. Plasters work directly on the focus of the disease, and are slowly absorbed by the body. The disadvantage of plasters is that skin irritation may arise if they are used frequently.
5.12. Lozenges
Preparation
Lozenges are taper-shaped pills. They are made from herbal powders with the addition of a viscous medium.
Applications
Lozenges are used orally or topically. In the latter case, they should be diluted with water and applied to the affected area. Herbs that promote blood circulation and treat trauma are often used in this form. They are easy to transport and store.
5.13. Powdered herbal extracts
Preparation
Using modern techniques, the ingredients are extracted at high or low temperatures, concentrated, combined with certain media and turned into powders.
Applications
They are prepared by adding boiling water at the time of administration. They are taken in small dosages and are easy to transport and store. They can be used for a range of disorders, in both acute and chronic conditions. The composition of formulas can be varied easily.
5.14. Pills, tablets and capsules made from powdered herbal extracts
Preparation
Pills, tablets and capsules can be made from the powdered herbal extracts described above.
Applications
They are taken in small doses and are quick and strong acting. They are easy to administer, transport and store.
6. Administration
The administration of herbal medicine should take into account the following principles.
6.1. Taking herbal medicine warm
Herbal medicine that is administered orally should always be taken warm. If the herbal medicine is a decoction, it should be taken when it is warm; herbal medicines that expel wind-cold are better taken hot. If the medicine is a powdered herbal extract, it should be dissolved in boiling water and taken once it has cooled down slightly.
Herbal pills, tablets or capsules should generally be taken with warm water. However, an exception is made to these two principles if the patient suffers from an excess heat syndrome in which the heat is so strong that it is impossible to accept any warm drinks. In this case, since the administration of warm fluids may cause vomiting, herbal medicines can be taken cool.
6.2. Appropriate frequency
Usually, herbal medicine is taken three times a day – in the morning, afternoon and evening.
• In acute and critical conditions, the herbal medicine should be taken every 4 hours, even during the night.
• When treating chronic diseases, herbal medicine can be taken twice a day, in the morning and in the evening. Once the patient’s condition improves, the frequency may be reduced and the herbal medicine can be taken once a day, every other day, or even twice a week to maintain the condition of the patient.
• The frequency of administration should be adjusted in some conditions; these include herbal medicines which induce sweating or which have a purgative action.
• Herbal medicines that eliminate parasites should be taken only once a day for a maximum of 3 days.
• Herbal medicines that reduce swelling, pain and irritation in the mouth, gums or throat should be retained in the mouth as long as possible before swallowing; they may be swilled around the mouth or gargled.
6.3. Timing of the administration
To maximize absorption of the herbs, herbal medicines are usually taken 1 hour before or after meals when the stomach is relatively empty. However, there are some exceptions:
• Tonifying herbs are best taken 1 hour before meals.
• Herbal medicines that promote digestion and strengthen the Stomach should be taken directly after meals.
• Herbal medicines that irritate the stomach should be taken after meals.
• Herbal medicines that drain downwards or eliminate parasites should be taken in the morning on an empty stomach.
• Herbal medicines that calm the mind and improve sleep should be taken before going to bed.
• Herbal medicines that control the attack of diseases such as asthma and malaria should be taken 1–2 hours before an attack.
7. Treatment principles and their sequence
In traditional Chinese herbal medicine, the treatment strategy and the composition of herbal formulas should follow a certain sequence, taking into account the following principles.
7.1. Regarding the human body, the body and the mind, and the body and the environment as integral parts
In treatment, pay attention to the relationships between:
• the internal organs, and between the internal organs and their related structures and orifices
• the body and the mind, the patient’s mental state, emotions, life experience and personality
• the body and the environment, which includes the climate, season and time, as well as the person’s working and private life, and the culture and society in which they live.
Regard each individual as unique in terms of their constitution, age, physical condition, diet and lifestyle.
7.2. Making a clear differentiation of the relevant syndrome(s)
Before commencing treatment, make a differentiation of the relevant syndrome(s) from the symptoms and signs so as to clarify the cause, location and nature of the pathogenic factors involved, and assess the relative strength of the body’s resistance and the pathogenic factors.
7.3. First making clear the relationship of Ben (the root or cause) and Biao (the manifestation)
Ben is more important than Biao, but the concepts are relative. In syndrome differentiation:
• the state of the body’s resistance is the Ben; the pathogenic change is the Biao
• the cause of the disease and the main pathological changes are the Ben; the symptoms are the Biao
• Zang organs and basic material substances of the body are the Ben; the orifice, structures and functions are the Biao
• the original, primary disease is the Ben; secondary diseases are the Biao.
7.4. Treat the Ben first and the Biao later
As a general rule, treat the Ben first and the Biao later. In an acute condition, however, treat the Biao first if it is pronounced as otherwise it may quickly cause further pathological change. Once the acute stage has passed, treat the Ben. When it is impossible to choose between the two, treat the Ben and the Biao together.
7.5. Eliminating exogenous pathogenic factors
Exogenous pathogenic factors should always be eliminated from the body. Once that has been accomplished, focus on restoring the healthy balance of the body.
When exterior pathogenic factors are com-plicated by interior pathogenic factors, treat the exterior factors first or treat both at the same time; do not treat only the interior pathogenic factors.
If an exterior syndrome arises during the treatment of a chronic disorder, the exterior syndrome should be dealt with first. For example, if a patient contracts an acute wind-heat invasion while having treatment for blood deficiency syndrome, the wind-heat invasion should be prioritized and treated first.
7.6. Strengthening the body’s resistance
The purpose of treatment is not only to eliminate pathogenic factors, but also to strengthen the body’s resistance, to maintain and improve the physical condition and constitution, to harmonize the Yin, Yang, Qi and blood, to re-establish the balance of the body, and to achieve a healthy mind and body. For example, to treat a bacterial infection, which often infers a damp-heat syndrome in TCM differentiation, the aim of treatment is not to kill the bacteria, but to eliminate damp-heat, promote the function of the Spleen and fortify the body’s resistance, thereby restoring health.
7.7. Treating complicated syndromes
In a condition where a deficiency syndrome is complicated by an excess syndrome, treat the excess syndrome first; if the excess is caused by the deficiency, treat both the excess and deficiency. Never treat only the deficiency because the cloying nature of the tonifying herbs may prevent the proper elimination of the pathogenic factors. For example, if accumulation of damp-phlegm in the Lung coexists with Spleen deficiency, the phlegm should be eliminated first; after that, the Spleen can be tonified. If the phlegm accumulation is caused by weakness of the Spleen (failing to transform dampness and phlegm), treatment should aim to tonify Spleen-Qi and remove phlegm at the same time.
7.8. Stopping treatment in time
During the course of treatment, be sure to strengthen the condition of the body so as to enable it to cure the disorder and restore internal equilibrium. Once the therapeutic effect has been achieved, treatment should stop.
7.9. Paying close attention to protect the Stomach and Spleen
During treatment, pay close attention to protect the Stomach and Spleen. Not only are these organs the source of the body’s Qi and blood, they are also responsible for the absorption of the herbal medicines (when these are administered orally). If the Stomach and Spleen are too weak and sensitive, treatment is more difficult.
7.10. Paying attention to special groups of patients and their physical characteristics
Women
Women have special physiological characteristics which should be considered when composing herbal formulas. First of all, blood is considered more important for women because they experience menstruation, pregnancy, delivery and breast-feeding, and these directly draw on the blood. When treating women, it is important to consider the changes in the blood and to tonify the blood at the appropriate time. Before menstruation, the blood is flourishing and Qi and blood stagnation can easily arise, so priority should be given to spreading the Liver-Qi. During and after menstruation, the blood is weakened but has a tendency to grow again, so the aims of treatment should be firstly to tonify the blood, and secondly to nourish the Yin and spread the Liver-Qi.
In a normal pregnancy, the Qi and blood are flourishing in the Chong and Ren meridians. This can often give rise to heat so cold herbs that reduce heat and soothe the Stomach-Qi are often used. After delivery, and while the mother is nursing the newborn baby, the Qi and blood are often weakened, therefore warm herbs that tonify the blood and Qi tend to be used.
Children
Children have special physiological characteristics. Their internal organs and structures are tender and fragile, the Qi and blood are not yet strong and their physiological functions are not fully developed. As such, they are easily attacked by exogenous pathogenic factors and disorders can develop quickly. In treatment, herbs that act quickly against the pathogenic factors and stop their development should be used promptly and in sufficient dosage. However, as soon as the therapeutic effect is achieved, the herbal treatment should be stopped since children generally recover quicker than adults as they have less medical history, stress and emotional disturbance. With proper diet, rest, exercise and care, children can recover completely.
When treating chronic conditions in children, pay special attention to tonifying the Kidney in order to support their physical and mental development.
Use small dosages of effective herbs which are mild in taste and smell as some children have difficulties taking herbs that have an unpleasant smell and taste.
The elderly
Generally speaking, the Qi and blood of elderly people are not as strong as they once were, and their bones and tendons are no longer firm. Their metabolism and digestion are slow. Furthermore, many of them become fragile mentally, especially when they have lost their loved ones or if they suffer from illness and social isolation. When treating elderly people, use herbs that promote digestion, tonify the Kidney, calm the mind and spread the Liver-Qi.
Postoperative patients and patients with chronic diseases
In the course of chronic disease, or after surgical operations, the Qi and blood are weakened. Dampness, phlegm and food tend to accumulate in the body because the Qi is too weak to eliminate them. Treatment therefore needs to tonify the Qi and promote digestion, eliminating any accumulation of dampness, phlegm or food.
Patients with special eating habits
Food can directly influence a person’s physical condition and constitution. Spicy and fatty foods, coffee and alcohol bring warmth to the body. If they are consumed in large amounts, they may generate heat and consume the Yin of the body. Most vegetables, fruits and cold drinks may bring cold and fluid to the body. If they are consumed in large amounts, the Yang of the body can be injured. Vegetarians should pay close attention to the nutritional value of the food they eat and should prepare their meals properly, otherwise their Qi and blood may be weakened, and malnutrition and illness may occur. The consumption of excessive amounts of sweet, fatty foods and dairy products may give rise to the accumulation of dampness or damp-heat in the body. All of the above factors should be considered when prescribing herbal medicine.
Patients suffering from stress, insomnia, emotional disturbance and exhaustion
At certain times, patients may experience extreme stress, anxiety, insomnia, tiredness and exhaustion, and at these times the body becomes very sensitive because the balance of Yin and Yang, and the normal relationship between the internal organs, are disturbed. In treatment, it is important to take into account all the relevant factors, such as how the Qi and the blood tend to move, the sensitivity of the body and the mind, and the possible coexistence of heat and cold, as well as weakness and excess. Herbal formulas should be gentle and balanced, and their administration should be carefully considered, as any strong reaction to the treatment may cause more disturbance to the patient’s condition.
8. Commonly used treatment methods and their applications
8.1. Inducing sweating
This method is used particularly to treat exterior syndromes. In Chinese herbal medicine, pungent and warm ingredients which enter the Bladder and Lung meridians, and which directly stimulate the Yang and Qi, are combined with herbs that stimulate the circulation of Qi and blood. By stimulating the Qi and Yang, opening the pores and inducing sweating, one can expel wind and cold from the superficial region of the body.
8.2. Purgation
This method is used to treat excess interior syndromes involving accumulations of food, toxic substances, feces or fluid. In Chinese herbal medicine, purgation is carried out by using herbs that enter the Large Intestine and which stimulate the intestine, move downwards and promote bowel movement, or by using herbs that enter the Lung and Kidney meridians and which promote urination. Ingredients that activate Qi movement in the Stomach, Liver and Lung are often used at the same time so as to enhance the purgative action. The strength of the purgative action can be adjusted so as to treat severe or mild, acute or chronic conditions.
8.3. Inducing vomiting
This method is used to remove poison from the Stomach. In Chinese herbal medicine, this method is carried out by using ingredients that enter the Stomach meridian, move upwards and directly induce vomiting so as to eliminate the toxic substance from the Stomach. This method is only used for acute conditions.
8.4. Harmonizing
This method is used to treat disharmony between internal organs, and between Qi and blood. It is also used to treat syndromes in which warm and cold pathological factors coexist, and syndromes in which deficiency coexists with excess. This method is carried out by combining upward- and downward-moving ingredients, dispersing and restraining ingredients, warm and cold ingredients, and tonifying and reducing ingredients. Ingredients that regulate Qi are always important here.
8.5. Warming the interior
This method is used to treat internal cold syndromes. It is carried out by using pungent and hot ingredients that enter the Heart, Spleen and Kidney meridians, disperse cold, warm the interior, open up the meridians and promote Qi movement. Herbs that are sweet and slightly warm, enter the Spleen and Kidney, tonify the Qi of the internal organs and gently promote the function of the Yang are also selected since Yang and Qi are closely related.
8.6. Clearing internal heat
This method is used to treat internal heat syndromes. In Chinese herbal medicine, cold ingredients that enter the regions where heat exists are applied. These ingredients have the functions of reducing heat, relieving fire-toxin, cooling the blood and generating body fluids.
8.7. Reducing
This method is used to reduce and soften accumulations of food, masses and nodules that are formed by phlegm and congealed blood. This method is carried out by using salty, bitter and pungent ingredients, which can soften hardness or break up accumulations. These should always be combined with herbs that promote Qi and blood circulation.
8.8. Regulating Qi
This method is used to treat syndromes of Qi stagnation. It involves the use of pungent and aromatic ingredients that enter the Liver, San Jiao, Lung, Stomach and Large Intestine meridians. These ingredients can directly stimulate Qi movement, smoothing its flow or spreading it through these organs and regions. They are often combined with purgative herbs and herbs that reduce accumulations of food and/or phlegm so as to assist the function of regulating the Qi.
8.9. Regulating blood
This method is used to treat blood stagnation. It is carried out by using pungent, aromatic herbs that enter the Heart, Pericardium, Liver and Gall Bladder meridians. These ingredients can directly stimulate blood circulation. To enhance their effect, they are combined with herbs that activate the Qi.
8.10. Reducing dampness
This method is used to treat syndromes involving dampness. When dampness is in the Upper-Jiao and in the superficial region, pungent or aromatic ingredients which enter the Lung, Spleen and Bladder meridians, and which can disperse dampness are used. When dampness is in the Middle-Jiao, bitter-warm and pungent-warm ingredients which enter the Spleen meridian and which can dry, dissolve and transform dampness are used. This method can also be effected by using bland and bitter ingredients that enter the Bladder meridian. These ingredients can dissolve and leach out dampness from the Lower-Jiao. Ingredients that promote digestion, regulate the Qi and tonify the Spleen are often selected to assist in the treatment of dampness.
8.11. Eliminating phlegm
This method is used to treat syndromes involving phlegm by transforming, drying and eliminating it. This method is carried out mainly by using pungent and bitter ingredients that enter the Spleen, Stomach and Lung meridians. These ingredients have dispersing and ascending, as well as reducing and descending abilities; they can directly transform and dissipate phlegm. This method can also be effected by using bitter and warm ingredients that can dry dampness.
Bland ingredients that can leach out water by increasing urination, ingredients that promote food digestion and purge accumulations, and ingredients that regulate the Qi are also used so as to prevent the formation of phlegm, thereby assisting the ingredients that directly dissolve, dry or eliminate the phlegm.
8.12. Tonifying
This method is used to treat different kinds of deficiency syndromes. It is carried out by using sweet, slightly warm ingredients that enter the five Zang organs. These ingredients tonify the Qi, blood, Yin and Yang of these organs. Ingredients that regulate the Qi and promote digestion are also used to assist the tonifying ingredients.
8.13. Stabilizing and binding
This method is used to treat any abnormal discharge of the essential substances of the body (i.e. essence, blood and body fluids). It also treats any abnormal consumption of the Qi, or any slippage of structures or organs from their original positions due to Qi deficiency. However, as this method does not treat the cause of these disorders, it should be used only for a short period of time and in acute conditions. This method is carried out by using sour, astringent, calcined substances that can directly stabilize the Qi, blood and body fluids, stop discharge and prevent further leakage. Herbs that can tonify and stabilize the Qi, blood, Yin and Yang are used at the same time in order to treat the cause of the problem.
8.14. Calming the mind
This method is used to sedate the spirit, calm the mind and regulate the function of the Heart in order to treat anxiety, restlessness, palpitations and insomnia. This may be achieved by using salty and cold herbs, especially minerals, which enter the Heart, Liver and Kidney meridians. These ingredients can sedate the Heart-spirit and descend the Yang of the Liver in acute, severe and excess conditions.
The method may also be carried out by using sweet, cold or warm ingredients that can nourish the Yin and tonify the Qi and blood, so as to treat chronic syndromes. Alongside these ingredients, some other herbs are also used, including pungent herbs that enter the Heart, Pericardium, Liver and Gall Bladder meridians and that can circulate the Qi and blood, and/or pungent and bitter ingredients that can remove phlegm in order to re-establish the connection between the Heart and Kidney and calm the mind.
8.15. Extinguishing wind
This method is used to treat internal wind syndromes. It is effected by using minerals and herbs which enter the Liver and Heart meridians and which can strongly and directly anchor Liver-Yang and subdue Liver-wind in order to treat severe and acute conditions when the Liver-Yang arises quickly and stirs up wind. Herbs that nourish Liver-Yin and enable it to control Liver-Yang are used in sub-acute or chronic conditions featuring Liver-Yang ascending with underlying Liver-Yin deficiency.
8.16. Opening the orifices and reviving the Shen (Heart-spirit)
This method is used to treat locked-up syndrome, an acute, severe and excess syndrome, which may occur on its own or develop from some severe diseases. The pathological change in this case is a sudden disturbance of Qi and blood, resulting in the obstruction and blockage of the sense orifices and of the associations between the internal organs by rebellious Qi, blood, phlegm and ascendant Yang. Characteristic symptoms in this syndrome show obvious signs of blockage of the orifices and a locked body, such as loss of consciousness, locked jaw, clenched fists, rigid limbs and the stoppage of urination and bowel movements.
The method is carried out by using very pungent or aromatic ingredients that can move quickly, activate the Qi movement, open up the blockage and reconnect the sensory orifices with the Shen and the internal organs, opening the orifices and reviving the Shen. Herbs that intensively eliminate phlegm are often administered at the same time, as phlegm can easily be formed in this disturbed state and may directly obstruct and block the orifices.
8.17. Moistening dryness
This method is used to treat syndromes of dryness that can be caused either by exogenous dryness or through the depletion of body fluids during the course of certain diseases, or through excessive use of certain drying medicines, herbs or spicy food. The etiology may also involve long-term stress which generates heat that in turn consumes the Yin and body fluids.
This method is carried out by using herbs to gently disperse dryness, regulate the Lung-Qi, transform phlegm, clear heat and moisten the Lung in exogenous dryness syndromes, and by using herbs to nourish the Yin and fluid of the Lung, Kidney, Stomach and Large Intestine in endogenous dryness syndromes.
9. Commonly used treatment strategies
9.1. Antagonistic treatment
This is a basic, regular treatment strategy used in most common cases. It infers an antagonistic therapy, which directly fights against the cause of the disorder and the main pathological changes. These include treating:
• a cold syndrome by warming
• a warm syndrome by cooling
• weakness by tonifying
• excess by reducing
• stagnation by activating the movement of the Qi
• scattered essential substances of the body by binding-up and stabilizing.
9.2. Following the symptoms while giving the treatment
The treatment strategy here partially follows the symptoms of the disease. This strategy is only used in extreme cases and is used together with the antagonistic method. For example, when there is extreme heat in the body, cold herbs are needed, but they may not be readily accepted by the body because of the tension created by the antagonistic nature of heat and cold. In these circumstances, a small amount of warm herb can be added to a formula consisting predominantly of cold herbs in order to help the body accept the cold herbs. Similarly, when extreme cold accumulates in the body, it may be hard for it to take hot herbs so a small amount of cold herb can be added to a formula in which warm herbs predominate in order to reduce the antagonism between the medicine and the syndrome. Other methods of reducing this tension include using sweet herbs and taking the herbal decoction at a cooler temperature.
9.3. Using ‘shortcuts’ to eliminate pathogenic factors
This is a strategy that considers the location of the pathogenic factors and takes the shortest route to eliminate them from the body. By using such ‘shortcuts’, pathogenic factors can be eliminated easily, quickly and effectively, with minimal harm being done to the body. For instance, when the disorder is located in the superficial aspect of the body, the method of inducing sweating should be used. When the poisoning substance is in the Stomach, the vomiting method can be used. If there is an accumulation in the Large Intestine, the method of purging the intestines can be applied.
9.4. Indirect tonification
To tonify the body, besides using the antagonistic method to directly tonify deficient organs or substances, there are other strategies which are said to be indirectly tonifying. These strategies are often used in a formula alongside the direct tonifying method.
The strategy of indirect tonification is based on the relationship between Qi and blood, and between Yin and Yang, as well as by the idea that the Qi is the commander of the blood, that the blood is the carrier of the Qi; that the generation of Yin depends on the stimulation of the Yang, and that the generation of Yang depends on the nourishment of the Yin. The following methods may all be considered examples of indirect tonification.
• According to Five-Element theory, when the ‘child’ organ is weak, one can tonify its ‘mother’ organ to strengthen it. For instance, when the Lung-Qi is weak, one can tonify the Spleen in order to strengthen the Lung-Qi.
• When blood is weak, first tonify the Qi in order to accelerate the function of blood production, and, at the same time, tonify the essence as essence and blood can transform into each other. As Yin is a part of blood, one can tonify the Yin when there is dryness and heat in the blood. This method is also used in critical situations where the patient has lost a large amount of blood in a short period of time, and it is impossible to generate the blood quickly, even with blood transfusion. At this time, Ren Shen and Huang Qi should be used first to strengthen the Qi in order to control and generate the blood.
• When the Yin is deficient, the Qi can be tonified in order to accelerate the generation of Yin. When Yang is deficient, the Qi can be tonified in order to strengthen the Yang because Qi is a part of Yang in a broad sense. This strategy often brings quick results.
• To tonify either the Kidney-Yin or the Kidney-Yang, a large amount of herbs that tonify the Kidney-essence should be applied as Kidney-essence is the fuel for the Yang and a substantial source of the Yin. When Kidney-essence is sufficient, the Yang acts on the Yin and generates the Kidney-Qi.
• When Kidney-Yang is weak, the Kidney-Yin should be tonified in order to assist the long-term generation of the Yang. In the formula, herbs that tonify Kidney-essence (from which the Yang is generated) are used along with the hot and pungent Yang tonic herbs.
• When Kidney-Yin is weak, the Kidney-Yang should be tonified. In the formula, herbs which tonify Kidney-essence are used to tonify the Yin, the material part of the body. In addition, a very small amount of hot and pungent herbs is used to activate the Kidney-Yang and thereby stimulate the growth of the Yin.
• When the Qi is deficient in general, the Spleen-Qi can be tonified first in order to generate the Qi of the other organs.
9.5. Paying special attention to protect and strengthen the Spleen
In TCM, the Spleen and Stomach are considered as the principal organs in strengthening the physical condition and are called the foundation of life. The concept of the earth being the center can be found in classical Chinese texts on philosophy and agriculture.
Postnatal growth and development depend on our digestion. The Spleen and Stomach are responsible for receiving, digesting and transforming food and drink into essence, Qi, blood and fluid, so they are very important organs. The Lung-Qi, generated from the Spleen-Qi, disperses the essence, Qi, blood and body fluids throughout the entire body, accelerates the function of the intestines and eliminates waste from the body.
Furthermore, as the Spleen and Stomach are located in the Middle-Jiao, which, by ascending and descending the water and the Qi, connects the Upper- and Lower-Jiao, they are in a key location to control the body’s physiology and pathology. Moreover, in practice, it is easier and quicker to strengthen the body through the Spleen than through other approaches, because it is easier to restore and tonify the post-heaven essence and Qi than it is to strengthen the pre-heaven essence and Qi which are stored in the Kidney.
9.6. Paying special attention to tonify the Kidney
The Kidney plays a key role in the body because the Yin, Yang, Qi and essence of the Kidney are the principal substances of life, and the Kidney determines the constitution and vitality of each individual. Moreover, the Yin, Yang, Qi and essence of the Kidney are the origin of the Yin, Yang, Qi and essence of the other organs, so the condition of the Kidney determines the condition of the whole body.
There are many very effective methods to treat Kidney deficiency based on the understanding of the relationship between the Yin, Yang, Qi and essence of the Kidney, and a series of strategies have been created. For instance, when treating Kidney-Yin deficiency, a small amount of herbs that tonify the Yang is added to a large amount of herbs that tonify the Yin. The aim of this is to warm and activate the Yang so as to power the generation of the Yin. Conversely, when treating Kidney-Yang deficiency, some herbs that tonify the Yin are added to the herbs that tonify the Yang because the Yin is regarded as the root of the Yang. When tonifying either the Yin or the Yang, a large amount of herbs that tonify the Kidney-essence is applied; this is because the Kidney-essence provides the fuel for the Yang and the substance for the Yin. When the Kidney-essence is sufficient, the Yang acts on the Yin, and then generates the Kidney-Qi.
As the Kidney is regarded as the root of life, many methods to indirectly strengthen the other organs through tonifying the Kidney have been created. For instance, when treating Spleen-Yang and Qi deficiency, herbs that tonify the Kidney-Yang and Qi are used in order to warm and generate the Spleen-Yang and Qi. When treating cough, shortness of breath and asthma caused by Lung-Qi deficiency, herbs that tonify the Kidney are applied in order to grasp the Qi and regulate breath. When treating chronic cough, thirst, rapid hungering, dry eyes and blurred vision caused respectively by deficiency of Lung-Yin, Stomach-Yin and Liver-Yin, herbs that first tonify the Kidney-Yin are applied in order to generate the Yin of these organs. To treat many emotional disorders, such as fear, anxiety, restlessness, poor memory and poor concentration, the method of tonifying the Kidney is also often used.
Since the Kidney-Qi and essence determine the development of the body, the method of tonifying the Kidney plays an important role in the treatment of retardation in children, menstruation disorders and learning difficulties in young people, infertility and menopause syndrome in adults, and declining function in the elderly.
Since the Kidney-Qi and essence are inherited from our parents and do not increase after we are born, tonifying the Kidney cannot be achieved in a short period of time. However, with this idea in mind, we can take steps to conserve our Kidney-Qi and essence throughout our lifetime. There are many ways to tonify and protect the Kidney, such as Chinese herbal therapy, Qi Gong exercise, Chinese dietary therapy and a healthy lifestyle. All of these can prevent disease, maintain health and ensure longevity. By this means, a person with a weak constitution can live a happy and healthy life, and someone with a strong constitution can live longer than average.
9.7. Strong tonification and gentle tonification
In strong tonification, either herbs with strong tonifying properties or large doses of herbs that are gentle in action are used to tonify severe weakness of Qi, blood, Yin and Yang. This method can generally be divided into strong tonification of the Yang and Qi, and strong tonification of Yin and blood.
Strong tonification of the Yin and blood is used for severe weakness of the blood and essence, such as in conditions of advanced wasting in diabetes, or starvation and dyscrasia in advanced cancer. Strong tonification is a particularly relevant therapeutic approach for young patients and for patients whose Spleen and Stomach are not impaired as the strong tonic herbs tend to be rich, sweet and cloying, and hence not easily digested.
In gentle tonification, either herbs that have gentle tonic properties or small doses of herbs with strong tonifying action are used to gradually tonify the Qi, blood, Yin and Yang in order to treat deficiency syndromes. This method is used much more often than the strong tonification method as deficiency syndromes tend be chronic conditions, and cases involving chronic deficiency are more often seen in clinical practice than acute cases.
Also, in chronic cases, all the organs and their functions are impaired and this makes it difficult for the body to tolerate strong tonifying herbs which are sweet, rich and cloying and often bring about digestive disorders, or which may be harsh in action and lead to new disturbances of Yin and Yang, Qi and blood. For example, if patients with dyscrasia are prescribed rich, sweet herbs that are too heavy to be digested by those whose digestive function is compromised, they can actually lose their appetite instead of putting on weight. A gentle method is thus more suitable for syndromes involving chronic deficiency.
9.8. Strategies for reducing interior excess heat
Besides the method of directly reducing excess heat in the related organ, there are other strategies to reduce it.
• According to Five-Element theory, when there is an excess condition in the ‘mother’ organ, the ‘child’ organ can be reduced or cleared. For instance, to reduce heat in the Liver, herbs that reduce Heart-fire can be used.
• When there is heat in the Zang organs, the corresponding Fu organ can be reduced. For example, by clearing and leaching out heat in the Small Intestine, Heart-fire can be reduced.
• When heat is intense in many organs and places, first the heat in the Yang Ming organs (the Stomach and Large Intestine) should be reduced as these organs are the ‘sea of heat’. Once the heat is reduced in the Yang Ming organs, the heat in the entire body can be reduced more quickly and effectively.
• To reduce excess heat in the entire body, Heart-fire, which is often generated by different emotions, can be reduced directly.
9.9. Strategies for treating Qi stagnation
Stagnation of Qi exists either alone or in many pathological conditions. There are a range of different strategies to treat Qi stagnation.
Spreading Liver-Qi, or regulating Liver-Qi, is the primary treatment for Qi stagnation, especially when the Qi stagnation is directly caused by emotional disturbance. This is because the Liver-Qi, as well as the Qi of the San Jiao and Gall Bladder, can accelerate the Qi movement in the entire body. Regulating the movement of Qi in the Lung, Stomach and intestines is important as the physical functions of these organs depend on the movement of the Qi.
It is also important to re-establish the proper direction of Qi movement between the internal organs. For instance, the Spleen-Qi should ascend and Stomach-Qi should descend; the Kidney-Qi should ascend and Lung-Qi should descend; the Kidney-water should ascend and Heart-fire should descend. Regulating the Qi of these organs may assist the normal Qi movement of the body.
Lastly, eliminating the stagnation of blood, food, dampness and phlegm may also assist the movement of the Qi and reduce Qi stagnation.
9.10. Strategies for treating internal dampness and water
Accumulations of dampness and water are not just pathological products arising from certain bodily disorders, they are also pathogenic factors in their own right and can cause further pathological change. There are different strategies to treat accumulations of dampness and water in the body, as follows.
• Activate the Qi movement, accelerate water metabolism and eliminate dampness.
• Use warm and pungent herbs to disperse the dampness.
• Use aromatic herbs which have a unique dispersing and transforming action to penetrate the dampness in the Upper- and Middle-Jiao and eliminate it.
• Warm the interior in order to dry dampness.
• Leach out dampness by using bland herbs that promote urination.
• Tonify the Kidney-Yang and strengthen the Spleen-Qi to accelerate water metabolism and transform dampness.
9.11. Strategies for treating heat and cold coexisting in one syndrome
When pathogenic heat and cold coexist in one syndrome, the treatment is difficult as warming the interior may increase the heat, and clearing heat may add to the cold. However, there is a special treatment strategy for dealing with this complicated condition, i.e. using pungent-warm herbs and bitter-cold herbs together. The pungent and warm properties can disperse cold, while bitterness and cold can clear heat. At the same time, the pungent herbs can lift the Qi upwards and the bitter herbs can direct the Qi downwards. These two groups of herbs can reduce the conflict between cold and heat, open up obstruction, and separate and eliminate both the cold and heat.
9.12. Strategies for harmonizing Ying and Wei
In conditions of deficiency and disharmony between the Defensive (Wei) aspect and the Nutritive (Ying) aspect, warm sweet herbs, which can strengthen the Yang and stimulate the Defensive-Qi in the superficial region of the body, are used. At the same time, sour and cold herbs that can nourish the Nutritive-Ying are also used. When these two groups of herbs are used together, harmony between the Defensive-Qi and the Nutritive-Yin aspects can be restored. At the same time, sweet warm herbs that enter the Spleen meridian are deployed to tonify the Spleen and strengthen the source of the Nutritive-Yin and Defensive-Qi. With this combination, the Ying and Wei become strong and balanced.
9.13. Strategies for tonifying the entire body in a balanced way
In many chronic diseases, deficiency often exists in more than one organ and the Qi, blood, Yin and Yang are all involved. Since patients with chronic disease are generally weak and their digestive function often impaired, they are unable to tolerate strong tonification or large numbers of herbs that tonify different organs at the same time. In these cases, it is wise to use small amounts of herbs to get the maximum effect. The herbs should be gentle and able to strengthen the body in a slow but balanced way. To achieve this goal, some strategies need to be applied.
First of all, choose sweet warm herbs that enter the Spleen meridian and tonify weakness in general, without consuming or injuring the Qi, blood, Yin or Yang. Herbs that regulate the Spleen and promote digestion are deployed at the same time so as to strengthen the source of Qi and blood and to ensure that the tonic herbs are properly absorbed. When the Spleen is strong, it can support other organs and improve the patient’s overall condition. One also needs herbs that are sweet, pungent and warm to gently and steadily tonify the Qi and Yang. Their sweet taste, together with the first group of sweet herbs, will minimize the possibility of injury to the Yin of the body. Sour and cold herbs that nourish the blood and Yin are also used, along with herbs that integrate and stabilize the actions of the whole formula.
10. Contraindications and cautions in the use of Chinese herbal medicine
10.1. Contraindications and cautions relating to syndromes
Certain formulas are contraindicated, or should only be used with caution, when patients have certain conditions, even though the formulas contain herbs that make them balanced. After all, each formula has a principal action and a specific application. Therefore, a clear and correct syndrome differentiation will ensure that the practitioner avoids the mistake of making a wrong formula. Specific contraindications and cautions relating to the applications of herbal formulas are discussed separately in each chapter. However, there are some general principles that should be noted here.
• Compose a formula using herbs of appropriate strength to treat the presenting syndrome. In this way, one can treat the syndrome effectively and avoid unnecessarily consuming the Qi and blood.
• When the patient’s Yang is weak, formulas that activate the Qi movement should not be used intensively because the Qi and the Yang have the same origin.
• When Qi, Yang, fire and wind are ascending in an acute pathological condition, herbs that move Qi, blood or Yang upwards and outwards should be used with caution. Relevant formulas here are those which treat Bi syndrome or exterior syndrome caused by wind, damp and cold, formulas that disperse and spread the Liver-Qi and formulas that treat headache caused by Qi and blood stagnation.
• If the Qi and Yang are weak and sinking, formulas that move downwards should be used with caution. The relevant formulas here are those that reduce heat and those that purge or break up accumulation of phlegm, Qi and blood. Since these formulas are very active in stimulating the Qi and blood, they may also consume the Qi. Patients may feel tired, especially if they are already Qi deficient.
• Generally speaking, formulas that release the exterior, warm the interior and expel wind-dampness and wind-cold are pungent or warm in nature. Their energetic tendencies are ascending and dispersing, especially those that contain herbs which can cause sweating. Overdose may disperse the Qi widely, consume the Yin of the body and cause other complications. When treating patients who are deficient in Yin or Qi due to their constitution, chronic disease, stress or dietary habits, these formulas should be used with caution.
• If there is an acute exterior syndrome, formulas that tonify the body and formulas that stabilize and bind the Qi, blood and essence should not be used because they will retain the pathogenic factors in the body. If the patient’s body resistance is weak, a small amount of herbs that tonify the Qi can be used in a formula with herbs that expel exogenous pathogenic factors in order to assist the expulsion of these pathogenic factors.
• Formulas that drain downwards are, in principle, not suitable for patients who suffer from exterior syndromes. It is better first to treat the exterior condition and then to drain downwards. Otherwise, the treatment may lead the exogenous factors into the deeper regions of the body.
• When a patient who has Qi deficiency suffers from constipation, formulas that tonify and ascend the Qi should be used with caution as they can worsen the constipation.
• If the patient sweats easily, which suggests that pores are open at that time, formulas that induce sweating should not be used because they are so strong that they may cause overdispersion of Qi and body fluids.
• When dampness occupies the superficial region of the body, it may be helpful to induce a mild sweat as this will open the pores and expel the dampness there. However, heavy sweating is not helpful as dampness tends to linger, and heavy sweating can injure the Yin of the body.
• If there are accumulations of phlegm, water, food, fire, Qi and blood in the body, formulas that tonify the body and formulas that stabilize and bind the Qi, blood and essence should not be used because they will retain the pathogenic factors in the body and lead to more complicated conditions. The correct procedure is to remove the pathogenic factors (and especially the substantial pathogenic factors) first, and then to begin treatment with tonic herbs. If the accumulations are caused by deficiency of Qi, blood, Yin or Yang, it will not be possible to remove these pathogenic factors completely without adding tonifying herbs to formulas that reduce accumulations. The ratio of the two types of herb must be varied in accordance with the relative strength of the pathogenic factors and the body’s resistance.
• Sweetness may cause retention of dampness in the Middle-Jiao. When treating phlegm and dampness, which are excessive lingering pathogenic factors, formulas that contain herbs that are sweet or sour in taste may cause retention of dampness and phlegm and so should be avoided or used with other herbs to reduce these undesirable effects.
• Formulas that actively and intensively remove phlegm, especially invisible phlegm, may cause unpleasant feelings and sensations at first because they provoke the movement of phlegm in the body. The practitioner should warn the patient about this in advance.
• When using mineral substances that can suppress Stomach-Qi, Lung-Qi and Kidney-Qi, causing Qi stagnation and constipation, one should exercise caution in treating patients who suffer from disorders that involve the aforementioned organs.
• The stomach is considered as the first step on the way to achieving therapeutic results when herbs are taken orally. If the stomach of the patient is weak or sensitive, strong formulas with harsh and cloying herbs and mineral substances should not be chosen. Moreover, formulas that promote blood circulation are also quite strong in action and have strong smells and tastes that can easily overburden the stomach. Consequently, they should be used with caution. When prescribing these formulas for patients who have weak stomachs, it is advisable to use low dosages and short courses of treatment, or to add herbs specifically to protect the stomach. In this way, it will be possible for the herbs to be absorbed by the body.
• Formulas that drain downward, promote Qi movement and blood circulation, remove or break up accumulations can also drain and stimulate Qi and blood. As such, they are not suitable for use in conditions involving bleeding.
• Formulas that cool the blood and stop bleeding may cause blood stagnation as many herbs are cold, astringent or partially charred. As soon as the bleeding stops, herbs that prevent congealed blood should be used.
10.2. Contraindications relating to herbal combinations which have dangerous or antagonistic effects
In classical texts, three groups of herbs are identified which are forbidden to be used together, otherwise toxicity and side effects may occur.
1. Gan Cao ( Glycyrrhizae radix) is incompatible with Gan Sui ( Euphorbiae kansui radix)*, Da  ( Knoxiae radix)*, Yuan Hua ( Genkwa flos)* and Hai Zao ( Sargassum).
( Knoxiae radix)*, Yuan Hua ( Genkwa flos)* and Hai Zao ( Sargassum).
 ( Knoxiae radix)*, Yuan Hua ( Genkwa flos)* and Hai Zao ( Sargassum).
( Knoxiae radix)*, Yuan Hua ( Genkwa flos)* and Hai Zao ( Sargassum).2. Wu Tou ( Aconiti radix)* is incompatible with Chuan Bei Mu ( Fritillariae cirrhosae bulbus), Gua Lou ( Trichosanthis fructus), Ban Xia ( Pinelliae rhizoma), Bai Lian ( Ampelopsitis radix) and Bai Ji ( Bletillae tuber)**.
3. Li Lu ( Veratri nigri radix et rhizoma) is incompatible with Ren Shen ( Ginseng radix), Sha Shen – Bei Sha Shen ( Glehniae radix)/Nan Sha Shen ( Adenophorae radix), Ku Shen ( Sophorae flavescentis radix), Xuan Shen ( Scrophulariae radix), Dan Shen ( Salviae miltiorrhizae radix), Xi Xin ( Asari herba)*, Shao Yao – Chi Shao Yao ( Paeoniae radix rubra)/Bai Shao Yao ( Paeoniae radix lactiflora).
As Gan Cao and Wu Tou are very commonly used, the first two groups of these herbs should be learned by heart.
There are nine pairs of herbs that are traditionally forbidden to be used together as it is believed that these combinations can minimize or neutralize their therapeutic effects:
• Liu Huang ( Sulfur)* antagonizes Po Xiao ( Glauberis sal)
• Shui Yin ( Hydrargyrum)* antagonizes Pi Shuang ( Arsenicum)*
• Lang Du ( Euphorbiae Fischerianae radix)* antagonizes Mi Tuo Seng ( Lithargyrum)*
• Ba Dou ( Crotonis fructus)* antagonizes Qian Niu Zi ( Pharbitidis semen)*
• Wu Tou ( Aconiti radix)* antagonizes Xi Jiao ( Rhinoceri cornu)**
• Ya Xiao ( Nitrum) antagonizes San Leng ( Sparganii rhizoma)
• Ding Xiang ( Caryophylli flos) antagonizes Yu Jin ( Curcumae radix)
• Ren Shen ( Ginseng radix) antagonizes Wu Ling Zhi ( Trogopterori faeces)
• Rou Gui ( Cinnamomi cassiae cortex) antagonizes Chi Shi Zhi ( Halloysitum rubrum).
Among these nine pairs, the first five are rarely used in clinical practice because their functions are so different that they can hardly be combined to treat one syndrome and some of them are so poisonous that they are rarely used nowadays. However, as the last four pairs can be used to treat the same syndrome, they must be memorized by heart.
10.3. Cautions relating to dietary habits
Cautions relating to dietary habits mean, on the one hand, that certain kinds of food should not be taken in certain syndromes or diseases; on the other hand, certain kinds of food should not be taken when certain herbs or formulas are used.
Generally speaking, during herbal treatment, patients should avoid cold, raw, heavy and spicy food. It is wise to suggest that patients drink light tea instead of coffee, that they should not take fresh drinks and fruit directly from the refrigerator and that they should eat vegetables cooked for a short time instead of salads.
If patients have had a heavy meal, it is good to take some tea or orange juice afterwards to help remove fat. They should also be encouraged to avoid heavy meals, to take semi-skimmed instead of whole milk, and to minimize their intake of candy, sugar, chocolate and alcohol as these may increase dampness in the body.
For patients who suffer from a cold syndrome, raw and cold food should be avoided. For patients who suffer from a heat syndrome or a syndrome where the Liver-Yang is ascending, spicy, heavy food, coffee and alcohol should be avoided. For patients who suffer from syndromes of damp-phlegm or damp-heat accumulation, sweet heavy food, milk products, nuts and alcohol should be avoided. Patients who suffer from skin disorders or have wounds which are characterized by itching, oozing and redness should avoid seafood, spicy food and alcohol.
Some herbs mentioned in classical texts are contraindicated with certain foods. For instance, all of the substances that tonify the blood should not be taken with strong tea. In addition:
• Dan Shen ( Salviae miltiorrhizae radix) and Fu Ling ( Poria) should not be taken with vinegar
• Sheng Di Huang ( Rehmanniae radix), Shu Di Huang ( Rehmanniae radix praeparata) and He Shou Wu ( Polygoni multiflori radix) are contraindicated with onion, garlic and radish
• Gan Cao ( Glycyrrhizae radix), Huang Lian ( Coptidis rhizoma), Jie Geng ( Platycodi radix) and Wu Mei ( Mume fructus) are contraindicated with pork
• Tu Fu Ling ( Smilacis glabrae rhizoma) and Shi Jun Zi ( Quisqualis fructus) are contraindicated with tea
• Chang Shan ( Dichroae febrifugae radix) is contraindicated with onion.
10.4. Cautions during pregnancy
During pregnancy, herbs can influence physiological changes in both the pregnant woman and the fetus, especially during the first 3 months. Generally speaking, it is better to keep the pregnancy natural, avoiding all kinds of treatment if they are not really necessary at that time.
• With regard to the strength and characteristics of herbs, formulas that contain poisonous or harsh herbs should not be used. Examples are Ba Dou ( Crotonis fructus)*, Qian Niu Zi ( Pharbitidis semen)*, Da  ( Knoxiae radix)*, Shang Lu ( Phytolaccae radix), Ban Mao ( Mylabris)* and She Xiang ( Moschus)**.
( Knoxiae radix)*, Shang Lu ( Phytolaccae radix), Ban Mao ( Mylabris)* and She Xiang ( Moschus)**.
 ( Knoxiae radix)*, Shang Lu ( Phytolaccae radix), Ban Mao ( Mylabris)* and She Xiang ( Moschus)**.
( Knoxiae radix)*, Shang Lu ( Phytolaccae radix), Ban Mao ( Mylabris)* and She Xiang ( Moschus)**.• Formulas that break up congealed blood should not be used in pregnant women. They may contain herbs such as Tao Ren ( Persicae semen), Hong Hua ( Carthami flos), San Leng ( Sparganii rhizoma), E Zhu ( Curcumae rhizoma), Shui Zhi ( Hirudo) and Mang Chong ( Tabanus)*.
• Formulas that promote blood circulation should be used with caution. If they really need to be used in treating disorders such as tumor, bleeding and severe pain due to blood stagnation in pregnancy, herbs that promote blood circulation can be used at low doses and the treatment course must be controlled carefully. An example is using Gui Zhi Fu Ling Wan (Cinnamon Twig and Poria Pill).
• Formulas that sedate Liver-Yang and calm the Heart-shen containing minerals such as Ci Shi ( Magnetitum), Shi Jue Ming ( Haliotidis concha) and Mu Li ( Ostrea concha) move downwards. They should be used with caution in pregnant women.
• Formulas that treat dampness should be used with caution in pregnant women as these formulas often contain herbs that have aromatic, pungent and bitter properties, which can easily move Qi and blood and drain dampness, and may endanger the fetus.
• Formulas that promote Qi movement, reduce food accumulation, and remove and break up phlegm accumulation can drain and stimulate Qi so they are not suitable for use in pregnancy. Examples include formulas that contain Mu Xiang ( Aucklandiae radix)**, Qing Pi ( Citri reticulatae viride pericarpium), Bing Lang ( Arecae semen), Zhi Shi ( Aurantii fructus immaturus), Lai Fu Zi ( Raphani semen), Zhe Bei Mu ( Fritillariae thunbergii bulbus) and Ban Xia ( Pinelliae rhizoma).
• Formulas with very pungent and warm herbs such as Fu Zi ( Aconiti radix lateralis preparata)*, Gan Jiang ( Zingiberis rhizoma) and Rou Gui ( Cinnamomi cassiae cortex) to warm the Lower-Jiao should be used with caution.
• Formulas that contain mineral substances are heavy for the stomach. If they are prescribed for pregnant women who are weak in the Stomach, they should be taken after meals.
10.5. Cautions during breast-feeding
The quality of the mother’s milk can directly influence the health of the baby. Generally speaking, the milk of a mentally and physically healthy mother nourishes and promotes the development of her baby. A mother who breast-feeds her baby should be aware of the following points:
• When she takes food or herbal formulas that contain very hot, spicy and pungent ingredients, these properties may be passed on to the baby via the breast milk and bring certain problems. Hot, spicy and pungent ingredients will tend to make the baby restless, and cause crying at night, skin rashes and eye infections.
• When she takes food or herbal formulas that contain very cold and pungent ingredients, these properties may cause the baby to have abdominal cramps and diarrhea, as well as restlessness and crying at night.
• If the nursing mother is in poor health or if she is poorly nourished, the quantity and quality of her milk can be insufficient for the baby’s development.
• When she is under strong emotions and stress, the baby may suffer abdominal cramps and poor digestion, and may easily get ill and cry in the night.
10.6. Cautions relating to the use of herbal formulas alongside western drugs
Quite commonly, when patients seek Chinese herbal medicine treatment, they have already been prescribed western medicines. A TCM practitioner should be aware of this and should use herbal formulas with consideration for the effects of the western drugs.
Although herbal formulas have not yet been analyzed from the perspective of modern pharmacodynamics and pharmacokinetics, and the interactions between drugs and herbs seem more complicated than can be revealed by the linear analytical models of pharmacology, one can study the actions of the western drugs from a TCM perspective and make a differentiation. For example, drugs that bring stimulating, exciting effects and promote metabolism have Yang characteristics while drugs that bring inhibiting, tranquilizing, narcotic effects and slow down the metabolism have Yin characteristics. Drugs that stimulate the function of the sympathetic nervous system belong to the Yang and those that stimulate the function of the parasympathetic nervous system belong to the Yin. As the effects of stimulants and inhibitors can be complicated, it is important to consider the effect of drugs on the body as a whole in order to make a differentiation, just as one considers the diet, the mental state and climate.
Cautions relating to western drugs and herbal formulas with similar effects
• If patients are on drugs for hypertension, tachycardia, anxiety and insomnia, herbs that strongly sedate Heart-shen and descend the Liver-Yang should be used with caution in the herbal formula.
• If patients are on antibiotics, which are considered cold substances that reduce heat and heat-toxin, formulas which strongly reduce fire and which are cold and bitter in nature should be used with caution.
• If patients are on prednisone or other adrenocortical hormones, herbal formulas that contain hot herbs which stimulate Kidney-Yang and Heart-Yang should be used with caution.
• If patients are on antidepressants or antipsychotics which are considered to slow down the movement of Qi, herbal formulas containing sweet, astringent and sour herbs that stabilize and bind the Qi, fluid and blood, and that suppress the Qi movement should be used with caution.
• If patients are on anticoagulants, herbal formulas that promote blood circulation and break up congealed blood should be used with caution.
• If patients are on drugs to stop pain, herbal formulas that treat Bi syndrome, which contain warm, pungent and dispersing herbs, should be used with caution.
• If patients are having radiotherapy or chemotherapy to treat cancer, formulas that strongly soften hardness, reduce accumulation, and activate Qi and blood circulation should be used with caution.
• If patients are on diuretic drugs, herbal formulas that promote urination and drain dampness should be used with caution.
• If patients are on antispasmodic drugs, formulas that stabilize and bind should be used with caution.
Cautions relating to western drugs and herbal formulas with antagonistic effects
• If patients are on sleeping pills, tranquilizers or beta-blockers, all of which have sedative effects, herbal formulas that stimulate the Qi and excite the Yang should be avoided. Formulas that strongly tonify the Qi should be used with caution.
• If patients are on anti-allergic and anti-asthmatic drugs, herbal formulas that stimulate the Qi and excite the Yang should not be used. Formulas that contain sweet and sour herbs that can slow down the Qi movement should also be avoided.
• If patients are on antispasmodic drugs, formulas that stimulate and tonify the Qi and Yang should not be used.
• If patients are undergoing a course of radiotherapy or chemotherapy, herbal formulas that quickly promote blood circulation and stimulate the Qi should not be used to avoid bleeding and metastasis. Formulas that strongly tonify the Qi should not be used on their own in order to minimize the possibility of promoting the growth of the tumor.
• If patients are on drugs that suppress the body’s immune system, formulas that strongly tonify the Qi and stimulate the Yang should be used with caution.
11. Combining western medicine with Chinese herbal formulas
The possibility of combining western drugs with Chinese herbal formulas or single herbs is based on clinical reality. Quite often patients who look to Chinese herbal medicine for treatment have already been prescribed western drugs. On the one hand, it is very necessary to use these drugs for treating certain diseases that cannot be adequately treated by Chinese herbal medicine. On the other hand, western drugs may be unable to adequately treat the disease, and may even have strong side effects, so Chinese herbal medicine may also be necessary. In this situation, the effects of western medicine on the body should be considered in the differentiation and treatment with Chinese herbal medicine. There is much evidence to show that Chinese herbal medicine can assist western drugs in the treatment of certain diseases, making them more effective while at the same time reducing their side effects.
To ensure that Chinese herbal formulas which are prescribed for use alongside western drugs are composed correctly, it is necessary to have a general idea of the main effects of western drugs on the body from the perspective of TCM. There are several examples, as set out below.
11.1. Antibiotics
Antibiotics are applied for treating bacterial infections. In TCM, infections are considered to be syndromes of heat, heat-toxin or damp-heat and antibiotics are considered as bitter and cold substances that can strongly and quickly reduce heat and heat-toxin, but that often injure the Qi and Yang of the Spleen and Stomach and may cause nausea, diarrhea and unpleasant sensations in the body. At the same time, they often suppress fire and cause Qi stagnation, leading to a hidden fire in the body.
Quite often, after patients finish their course of antibiotics, the infection recurs and even becomes chronic. In this case, a formula should be composed using low doses of cold bitter herbs which have similar functions to the antibiotics but with a broader spectrum, along with herbs that can strengthen the Middle-Jiao, transform the dampness and promote digestion as well as dispersing the constrained Qi and heat. In this way, infections can be cured with minimal side effects from the antibiotics.
11.2. Drugs for treating hypertension
Before receiving drug treatment, patients with hypertension often have a syndrome of Liver-Yang ascending with Kidney-Yin and Liver-Yin deficiency. The drugs for treating hypertension can quickly descend the Qi and Yang of Liver, but they may suppress the Liver-Qi. They may also slow down water metabolism and blood circulation. Therefore the syndrome can change into one of Liver-Qi stagnation with Kidney-Yin and Liver-Yin deficiency, or Liver-Qi stagnation with dampness accumulation in the Middle-Jiao.
Once they have started using western medicine, patients’ symptoms may change from irascibility, headache and dizziness to tiredness, irritability and frustration. Sometimes, the blood pressure cannot be controlled in a stable way using drugs, and the syndrome of Liver-Yang ascending with deficiency of the Liver-Yin and Kidney-Yin continues to prevail. This is because patients often instinctively want to overcome the unpleasant sensations and feelings that occur when the Liver-Yang suddenly descends as a result of the drug treatment, so they try to feel fit and active and thereby force the Qi and Yang to move upwards. In this process, constrained heat can be generated. This constrained Qi and heat may lead to therapy-resistant hypertension. This can obviously be found in the pulse diagnosis.
Since the syndrome has changed, the herbal formulas should be created using herbs that spread the Liver-Qi and promote blood circulation. Herbs that nourish the Kidney-Yin and Liver-Yin, reduce constrained heat and improve sleep should be prescribed at the same time.
11.3. Anticoagulants
Anticoagulants are used to prevent cardiovascular and cerebrovascular accidents. Most patients who are on anticoagulants are elderly people with chronic heart and vascular diseases. From a TCM perspective, the blood becomes thicker and tends to coagulate when heat (often generated by stress and emotional disturbance) consumes the blood, or when phlegm accumulates as a result of Spleen deficiency. Kidney deficiency is a potential cause of this as the Kidney-Qi weakens with age and is unable to maintain the proper functioning of the Spleen and Liver.
After using anticoagulants, although the blood becomes thinner, the patient’s pulse is still wiry and the tongue is often red with a sticky coating. These signs indicate that there is still heat and phlegm accumulation in the body. In the treatment, herbs should be used to tonify the Kidney, strengthen the Spleen, spread the Liver-Qi and calm the mind. These herbs will prevent heat generation and phlegm accumulation. Meanwhile, pungent ingredients that can quickly promote Qi movement and blood circulation should be used with caution.
11.4. Drugs for treating hyperlipidemia
In TCM, hyperlipidemia is considered to be a syndrome in which an underlying deficiency of the Kidney coincides with Spleen-Qi deficiency and an accumulation of damp-phlegm due to improper diet and poor digestion, along with stagnation of Qi and blood due to a lack of physical exercise and long-term stress – both of which tend to worsen the condition of the Spleen. Western drugs can reduce the hyperlipidemia in a reasonably short period of time but the underlying conditions of Spleen and Kidney have not been changed and the stress is still there. Moreover, this quick change in the body’s metabolism places an extra burden on the Spleen and can eventually worsen the condition of this organ.
In a common case of hyperlipidemia, herbal formulas can be composed and used alongside western drugs. It should be possible to regulate the Liver, Spleen and Stomach, transform dampness and promote digestion, particularly the metabolism of fats. If hyperlipidemia has developed and has resulted in detectable damage to the heart, brain and vascular system, herbs to strongly remove dampness and phlegm, clear heat, stimulate Qi movement and blood circulation, nourish the Yin and pacify the Liver should be added to the formula. In all conditions, herbs that tonify the Spleen and Kidney should be prescribed.
11.5. Drugs for treating diabetes
After using drugs to treat type II diabetes, blood glucose levels usually return to normal and the typical symptoms of hunger and thirst tend to disappear. However, the cracks on the patient’s tongue, which indicate Yin deficiency, remain unchanged. The tongue coating is thicker than it was before using the drugs, indicating the accumulation of dampness and phlegm. The patient’s pulse is often deep and weak, especially in the Spleen and Kidney positions, which indicates that the underlying deficiency has not improved.
In herbal treatment, it is necessary to tonify the Kidney and Spleen-Qi in order to nourish the Yin of the Stomach and the Lung. At the same time, herbs that eliminate dampness or damp-heat should also be used.
11.6. Hypnotic and sedative drugs
Hypnotic and sedative drugs are often used in the treatment of mental disorders. From a TCM perspective, they have the function of sedating the Heart-shen and descending the Liver-Yang. Some of them have an intense sedating action that can directly suppress the Qi and Yang and cause sudden Qi and blood stagnation, especially when the patient first starts taking these drugs. Patients may feel tired and weak; they may also have a heavy or a light sensation in the head, dizziness and poor concentration. When patients instinctively try to overcome these unpleasant sensations and feelings, Qi and Yang try their best to move upwards. In this process, constrained heat can be generated. The constrained Qi and heat may lead to therapy-resistant insomnia and anxiety. From a TCM perspective, when the Qi is not able to accelerate water metabolism and food digestion, phlegm-heat is formed and may occlude the mind, leading to mild but chronic insomnia, restlessness and anxiety. Moreover, if the blood is deficient in the Liver and is unable to house the Hun, the person will not be able to sleep soundly even with the aid of hypnotic drugs.
In these situations, treatment procedures in TCM that are similar in approach to the hypnotic and sedative drugs should not be used, or used only with caution. Instead, procedures that disperse constrained Qi, clear heat, promote digestion, and remove dampness and phlegm should be applied. Herbs and a diet that tonify the blood should be used for a long period of time. All of these can assist western drugs to calm the mind in an effective way and to reduce their side effects. TCM treatment can thus shorten the course of treatment required with hypnotic and sedative drugs and reduce their dosage.
11.7. Antidepressants
Antidepressants are recommended when patients are unable to cope with their depression, anxiety or chronic pain on their own or with the aid of psychotherapy.
From a TCM perspective, tricyclic antidepressants have a descending tendency and a sedating action. They can suppress the Qi and Yang, slow down digestion and water metabolism, cause stagnation of Qi and blood, and the accumulation of dampness and water. Thus patients may put on weight and feel tired and experience a feeling of heaviness in the body. When dampness and phlegm persistently accumulate in the body and block the meridians, depression may get worse in the long term. In TCM treatment, by strengthening the function of the Spleen, removing the dampness and phlegm, and promoting Qi movement, patients can feel much more comfortable.
Some antidepressants such as the monoamine oxidase (MAO) inhibitors can stimulate the Yang of the Kidney and Heart. They are used mainly for treating atypical depression, agoraphobia and social phobia. However, in TCM terms, if there is stagnant heat in the Liver, MAO inhibitors can bring unsatisfactory results in treatment, and may have strong side effects that usually occur before the depression is effectively relieved. Since these drugs may stimulate the Yang of the Kidney and Heart, they can be dangerous if the will-power of the patient is stimulated suddenly and quickly as this may give patients the impulsive mental strength to commit suicide.
For patients who take antidepressants from these last two groups, TCM treatment should be applied according to careful syndrome differentiation, to remove the obstruction, harmonize the Qi and blood, and balance the Yin and Yang in order to prevent and reduce the side effects of the drugs.
St John’s wort and Ginseng are also frequently suggested for treating mild depression. According to syndrome differentiation in TCM, they are only suitable for treating patients who suffer from depression due to deficiency of Qi and Yang. If the patients have a Yin deficiency, internal heat or constrained heat due to stress and anxiety, these herbs may lead to restlessness and insomnia, and may make the condition worse. In this case, a Chinese herbal formula based on syndrome differentiation is more effective than that of using only these herbs.
11.8. Drugs for treating hypothyroidism
In TCM, hypothyroidism is considered a syndrome of Spleen-Qi deficiency and accumulation of dampness or damp-phlegm in the body. Although western drugs may help to keep thyroid hormone levels normal, symptoms such as tiredness, coldness, weight gain and constipation may still exist. In the differentiation of the syndrome, many patients still show signs of Spleen-Qi deficiency and accumulation of dampness in the body, therefore treatment should be given to tonify the Spleen-Qi, activate Qi movement and leach out dampness.
11.9. Radiotherapy and chemotherapy
These therapies are mainly used for cancer treatment and are considered as heat-toxin in TCM. When the cancer cells are killed, the body is severely injured too. The Yin and the Qi in particular are seriously depleted and weakened by the extreme heat. Moreover, these therapies can cause further disturbances in the body such as deficiency of Kidney-essence and blood, blood stagnation, bleeding, empty-heat in the blood or up-flaring of empty-heat. Therefore, during herbal treatment, herbs that nourish the Yin, tonify the Qi and reduce heat-toxin should be used.
Once the course of therapy is completed, it is still necessary to tonify the Yin and the Qi and to reduce the empty-fire. It is recommended that herbs to tonify the Kidney are used for a long period of time.
11.10. UVB phototherapy, psoralen plus UVA photochemotherapy (PUVA)
For treating psoriasis, UVB phototherapy and PUVA are effective treatments that permit rapid control of the disease, but their side effects are similar to those of radiotherapy and chemotherapy. While these treatments can suppress the pathogenic change and rapidly improve the skin lesions, the heat penetrates into the blood, consumes the blood and Yin, and generates heat-toxin. Once the therapy is finished, the heat quickly arises and the skin lesions appear again, even worse than before the treatment, and the skin becomes more sensitive in general. In herbal treatment, one needs to reduce the heat-toxin, cool the blood, promote blood circulation and nourish the Yin.
11.11. Glucocorticoids (adrenocortical hormones)
Glucocorticoids have potent anti-inflammatory and immunosuppressive properties. This is particularly evident when they are administered at pharmacological doses. A variety of synthetic glucocorticoids, some far more potent than cortisol, have been created for therapeutic use, such as hydrocortisone, prednisone, prednisolone, dexamethasone and betamethasone.
Glucocorticoids are widely used as drugs to treat arthritis and dermatitis. In pharmacological doses, they are used to suppress various allergic, inflammatory and autoimmune diseases. They are also administered as post-transplant immunosuppressants. Nevertheless, they do not prevent infection and they also inhibit subsequent regenerative processes. Excessive glucocorticoid levels have side effects on many systems, such as the inhibition of bone formation, delayed wound healing, muscle weakness and an increased risk of infection.
With a very high dose of glucocorticoids, patients become restless and their tongue becomes redder. This empty-heat can further consume the Kidney-Qi, weaken the body’s resistance and eventually leads to an increased risk of new infections. Thus, when composing a herbal formula for a patient who is on glucocorticoids, herbs that can steadily tonify the Kidney-Qi and Kidney-Yin should be prescribed, along with herbs that cool the blood and calm internal wind. Once the dose of glucocorticoids has been reduced or even stopped, herbs that tonify the Kidney-Qi, Kidney-Yin and Kidney-Yang should be given for a long period of time.
12. Substitutions for unavailable, protected and banned herbs
Traditional Chinese herbal medicine has a long history, dating back 5000 years to the beginning of the Chinese civilization. It is the result of people’s effort to utilize nature for survival and is developed on the basis of long-term observation, study and practice under the guidance of ancient philosophy.
However, as the relationship between humans and nature has changed with time, some ingredients in TCM have become unavailable or protected and banned by legislation. Traditional herbal medicine must accommodate such change. Alongside the usage of cultivated herbs and synthetic ingredients in clinical practice, one can also use herbs with similar actions as substitutes. However, one must always bear in mind that, due to the specific function and characteristic of each herb, the therapeutic result of the substituted herb will never be completely the same as the original one.
The suggested substitutes are as follows:
• Xi Jiao ( Rhinoceri cornu)** can be replaced by Shui Niu Jiao ( Bubali cornu). It can also be replaced by Da Qing Ye ( Isatidis folium) and Sheng Ma ( Cimicifugae rhizoma) at a ratio of 10 : 1.
• Hu Gu ( Tigris os)** can be replaced by Qian Nian Jian ( Homalomenae rhizoma) and the bones of cat, pig or ox.
• Ling Yang Jiao ( Antelopis cornu)** can be replaced by Shan Yang Jiao ( Naemorhedis cornu). It can also be replaced by Shi Jue Ming ( Haliotidis concha) and Qing Dai ( Indigo naturalis) with a small amount of Chai Hu ( Bupleuri radix) and Mu Dan Pi ( Moutan cortex).
• Lu Rong ( Cervi cornu)** can be replaced by the combination of Ba Ji Tian ( Morindae radix) and Rou Gui ( Cinnamomi cassiae cortex). It will also be helpful if venison is included in the patient’s diet.
• Gui Ban ( Testudinis carapax)** can be replaced by the combination of Shu Di Huang ( Rehmanniae radix praeparata) and Shan Zhu Yu ( Corni fructus). Meat and bone-marrow are also recommended in the patient’s diet.
• Bie Jia ( Trionycis carapax)** can be replaced by Shu Di Huang ( Rehmanniae radix praeparata) and Sheng Di Huang ( Rehmanniae radix) with Mu Dan Pi ( Moutan cortex).
• She Xiang ( Moschus)** and Niu Huang ( Bovis calculus)** should be replaced by synthetic versions.
• Tian Ma ( Gastrodiae rhizoma)** can be replaced by Gou Teng ( Uncariae ramulus cum uncis), Man Jing Zi ( Viticis fructus), Ju Hua ( Chrysanthemi flos) or Bai Ji Li ( Tribuli fructus) to pacify the Liver and extinguish Liver-wind, or combined with Xia Ku Cao ( Prunellae spica), Di Long ( Pheretima) and Jiang Can ( Bombyx batrycatus) to eliminate wind-phlegm.
• Shi Hu ( Dendrobii caulis)** can be replaced by the combination of Sheng Di Huang ( Rehmanniae radix) and Shu Di Huang ( Rehmanniae radix praeparata).
• Gou Ji ( Cibotii rhizoma)** can be replaced by Gu Sui Bu ( Drynariae rhizoma).
• Bai Ji ( Bletillae tuber)** can be replaced by Zi Zhu Cao ( Callicarpae folium).
• Mu Xiang ( Aucklandiae radix)** can be replaced by Chuan Mu Xiang ( Vladimirae radix), Qing Pi ( Citri reticulatae viride pericarpium) or Sha Ren ( Amomi xanthioidis fructus).
• Hou Po ( Magnoliae cortex) can be replaced by Zi Su Geng ( Perillae caulis et flos) and Chuan Mu Xiang ( Vladimirae radix) to regulate Qi and reduce distension. To direct Qi downward and remove dampness and food stagnation it can be replaced by Cang Zhu ( Atractylodis rhizoma), Zhi Shi ( Aurantii fructus immaturus) and Ban Xia ( Pinelliae rhizoma).
• The use of Zhu Sha ( Cinnabaris)* is forbidden. It can be replaced by Long Chi ( Mastodi fossilia dentis) and Zhen Zhu ( Margarita usta) with Huang Lian ( Coptidis rhizoma) to calm the mind.
• Guan Mu Tong ( Hocquartiae manshurensis caulis)* is a poisonous herb and its use is forbidden. It should be replaced by Chuan Mu Tong ( Clematidis armandii caulis) with careful control of both Chinese name and Latin name, or it can be substituted by Zhi Zi ( Gardeniae fructus) or Tong Cao ( Tetrapanacis medulla) with Huang Lian ( Coptidis rhizoma) or Long Dan Cao ( Gentianae radix).
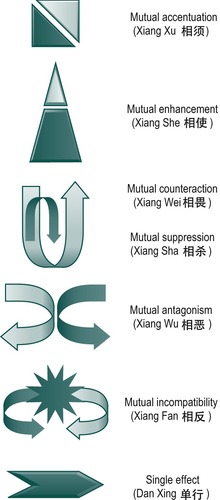 |
| Figure I.1 •. |
| Common types of herbal combination. |
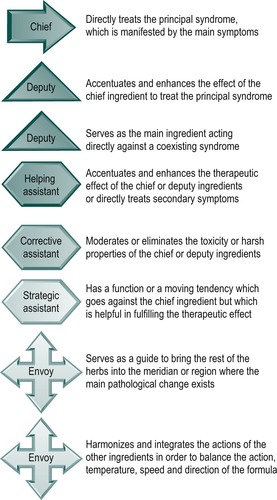 |
| Figure I.2 •. |
| The structure of a formula. |





