Chapter 54 Distraction osteogenesis and obstructive sleep apnea syndrome
Maxillofacial skeletal deficiency in the sagittal and frontal plane has been shown to be a major contributing factor in obstructive sleep apnea syndrome (OSA). Despite the success of conventional surgical procedures in maxillofacial skeletal expansion, increasing interest has been generated in the use of distraction osteogenesis for skeletal expansion for the management of OSA. This chapter will discuss the method as well as relevant results.
1 INTRODUCTION
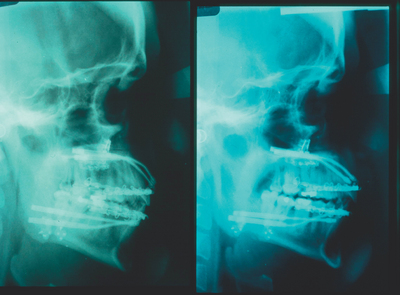
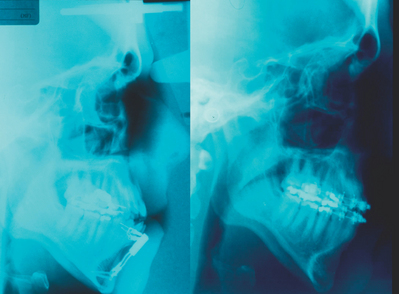
Maxillofacial skeletal abnormality is a well-recognized predictor in OSA. Maxillomandibular deficiency results in diminished airway dimension which leads to nocturnal obstruction.1,2 Currently, the most effective surgical procedure in the management of OSA is the expansion of facial skeleton by advancing the maxilla and mandible, i.e. maxillomandibular advancement (MMA). MMA achieves enlargement of the pharyngeal and hypopharyngeal airway by physically expanding the skeletal framework. In addition, the forward movement of the maxillomandibular complex improves the tension and collapsibility of the suprahyoid and velopharyngeal musculature. Lateral pharyngeal wall collapse, which has been shown to be a major factor in airway obstruction,3 is also shown to be lessened following MMA.4 The current MMA technique involves the use of maxillary Le Fort I osteotomy and mandibular sagittal split osteotomy to facilitate the forward movement of the maxillomandibular complex followed by the application of rigid fixation.5
Since the early recognition of the role of maxillofacial skeletal deformity in OSA, all of the emphasis of deformity recognition and treatment has been primarily limited to the sagittal plane. The transverse deficiency of the maxilla and/or mandible as a potential contributor and treatment of OSA has received little attention. Recently, the constriction of the maxilla has been suggested as a possible risk factor of OSA. In a comparative study between OSA and control subjects by Seto et al.,6 OSA subjects were found to have narrower, more tapered and shorter maxillary arches. Kushida et al.7 found that the intermolar distance of the maxilla is related to the presence of OSA. Cistulli et al.8 have reported that patients with Marfan’s syndrome, in which maxillary constriction is a common finding, have increased incidence of OSA and elevated nasal resistance. The relationship of nasal resistance and maxillary morphology has long been suggested in the orthodontic literature.
2 DISTRACTION OSTEOGENESIS IN THEMAXILLOFACIAL REGION
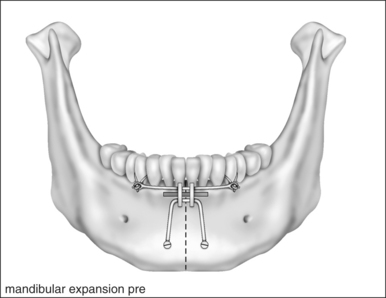
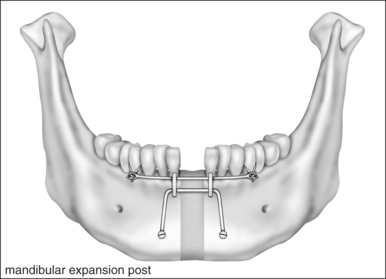
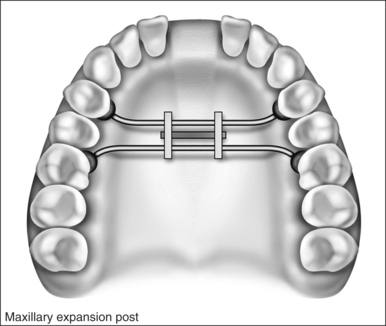
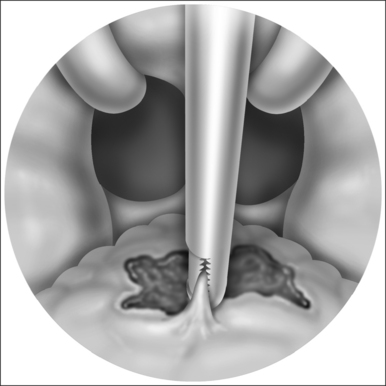
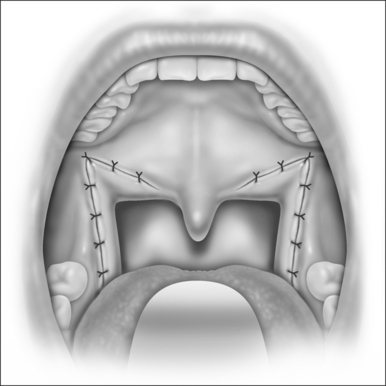
Skeletal expansion by slow osseous distraction (distraction osteogenesis) is not new and has been previously studied extensively in orthopedic surgery. It has demonstrated acceptable feasibility, efficacy, safety, and reproducibility of its treatment results. In its simplest form, distraction osteogenesis (DO) describes the generation of new bone in the stretched fracture callus. A screw-driven appliance that is firmly attached to the bone fragments slowly pulls apart the cut/or fractured bony edges, and new bone can fill in the stretched callus tissue. DO was first described by Alessandro Codvilla in 1905, who first published the use of this technique in lengthening the long bone.9 However, it is Ilizarov who is credited with developing the current methods of DO.10 DO in the maxillofacial region was first investigated by Snyder et al.11 in the canine mandible. Karp et al.12 demonstrated that bone formation during DO in the maxillofacial region is similar to that of long bones, which is predominantly by intramembranous ossification. Surgical lengthening by DO in sagittal plane was first described by McCarthy, who reported on the application of DO of the human mandible in pediatric patients in 1992.13 The surgical expansion of the maxilla and mandible to increase the width by distraction osteogenesis was reported by Bell and Epker14 and Guerrero,15 respectively.
5 DISCUSSION
DO offers several advantages over the conventional techniques by eliminating the need for bone grafting, and it involves less surgical dissection because bone lengthening is the result of natural bone healing in a gap created by a simple osteotomy. The incremental skeletal movement allows accommodation of the soft tissue, thus enabling large skeletal movement that usually cannot be achieved by conventional techniques. The gradual soft tissue accommodation also improves the stability of the new skeletal position.
The major advantage in the application of DO for maxillofacial skeletal expansion is in the pediatric population where access for the conventional procedure is limited, the volume of bone is insufficient for conventional procedure, there is a need for much greater skeletal expansion than the conventional technique can provide and the potential for surgical scarring by conventional procedure due to the extensiveness of the operation, which can negatively impact future facial growth. Both advancement and widening of the maxilla and mandible have been shown to improve OSA. Maxillary widening improves nasal airway resistance,16,17 although the beneficial effect of maxillary expansion on nasal resistance may not be uniformly achieved in all patients. It appears that patients with greater degrees of nasal resistance tend to have greater improvement after maxillary expansion.18,19 Nocturnal enuresis is improved in children.20,21 Cistulli et al.22 performed maxillary expansion on 10 OSA patients with maxillary constriction and improvement was achieved in nine of the 10 patients. The mean Apnea/Hypopnea Index (AHI) was reduced from 19 events per hour to seven events per hour, and the mean maxillary expansion achieved was 12.1 mm. It is unknown whether mandibular expansion can be performed with maxillary expansion, and if simultaneous maxillary and mandibular expansion can improve OSA. Pirelli et al.23 treated 31 children with orthodontic maxillary expansion. Nasal resistance was improved in all patients. The AHI was reduced from 12.2 events per hour to less than one event per hour. The mean expansion was 4.32 mm.
There is extensive literature support for the application of DO to advance the maxilla or the mandible. Since the initial report by McCarthy et al.13 mandibular advancement by DO in the pediatric population has gained increasing popularity. The majority of the studies have demonstrated impressive success in the management of OSA in pediatric patients with craniofacial syndromes.24–27 It has become the preferred management in patients who are tracheotomy dependent and the majority of the patients can be decannulated following DO. Contrarily, DO to achieve maxillary or mandibular advancement in the adult population has not gained significant acceptance. Only two centers have reported their experience of DO in the management of adult OSA.28,29 This is likely due to the increased treatment time required, the presence of distraction devices which significantly affect the patient’s mastication, aesthetics and speech. These unfavorable factors have limited the patient’s acceptance of DO in the adult population.
1. Jamieson A, Guilleminault C, Partinen M, Quera-Salva MA. Obstructive sleep apneic patients have craniomandibular abnormalities. Sleep. 1986;9:469-477.
2. DeBerry-Borowiecki B, Kukwa A, Blanks R. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988;98:226-234.
3. Schwab RJ, Gefter WB, Hoffman EA, Gupta KB, Pack AI. Dynamic upper airway imaging during respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385-1400.
4. Li KK, Guilleminault C, Riley RW, Powell NB. Obstructive sleep apnea, maxillomandibular advancement and the airway:a radiographic and dynamic fiberoptic examination. J Oral Maxillofac Surg. 2002;60:526-530.
5. Li KK. Surgical therapy for adult obstructive sleep apnea. Sleep Med Rev. 2005;9:201-209.
6. Seto BH, Gotsopaulos H, Sims MR, Cistulli PA. Maxillary morphology in obstructive sleep apnea syndrome. Eur J Orthod. 2001;23:703-714.
7. Kushida C, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Int Med. 1997;127:581-587.
8. Cistulli PA, Richards GN, Palmisano RG, Unger G, Berthon-Jones M, Sullivan CE. Influence of maxillary constriction on nasal resistance and sleep apnea severity in patients with Marfan’s syndrome. Chest. 1996;110:1184-1188.
9. Codvilla A. On the means of lengthening, in lower limbs, the muscles and tissues which are shortened through deformity. Am J Orthop Surg. 1905;2:353-369.
10. Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Joint Dis Orthop Inst. 1988;48:1-11.
11. Snyder CC, Levine GA, Swanson HM, Browne EZ. Mandibular lengthening by gradual distraction: preliminary report. Plast Reconstr Surg. 1973;51:506-508.
12. Karp NS, McCarthy JG, Schreiber JS, Sissons HA, Thorne CHM. Membranous bone lengthening: a serial histological study. Ann Plast Surg. 1992;29:2-7.
13. McCarthy JG, Schreiber J, Karp N, Thorne CHM, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992;89:1-10.
14. Bell WH, Epker BN. Surgical-orthodontic expansion of the maxilla. Am J Orthod. 1976;70:517-528.
15. Guerrero CA, Bell WH, Contasti GI, Rodriguez AM. Mandibular widening by intraoral distraction osteogenesis. Br J Oral Maxillofac Surg. 1997;35:383-392.
16. Timms DJ. The effect of rapid maxillary expansion on nasal airway resistance. Br J Orthod. 1986;13:221-228.
17. Timms DJ. The reduction of nasal airway resistance by rapid maxillary expansion and its effect on respiratory disease. J Laryngol Otol. 1984;98:357-362.
18. White BC, Woodside DG, Cole P. The effect of rapid maxillary expansion on nasal airway resistance. J Otolaryngol. 1989;18:137-143.
19. Hartgerink DV, Vig PS, Abbott DW. The effect of rapid maxillary expansion on nasal airway resistance. Am J Orthod Dentofac Orthop. 1987;92:381-389.
20. Timms DJ. Rapid maxillary expansion in the treatment of nocturnal enuresis. Angle Orthod. 1990;60:229-233.
21. Kurol J, Modin H, Bjerkhoel A. Orthodontic maxillary expansion and its effect on nocturnal enuresis. Angle Orthod. 1998;68:225-232.
22. Cistulli PA, Palmisano RG, Poole MD. Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. Sleep. 1998;21:831-835.
23. Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion in children with obstructive sleep apnea syndrome. Sleep. 2004;15:761-766.
24. Cohen SR, Simms C, Burstein FD. Mandibular distraction osteogenesis in the treatment of upper airway obstruction in children with craniofacial deformities. Plast Reconstr Surg. 1998;101:312-318.
25. Monasterio FO, Drucker M, Molina F, Ysunza A. Distraction osteogenesis in Pierre Robin sequence and related respiratory problems in children. J Craniofac Surg. 2002;13:79-83.
26. Williams JK, Maull D, Grayson BH, et al. Early decannulation with bilateral mandibular distraction for tracheostomy-dependent patients. Plast Reconstr Surg. 1999;103:48-57.
27. Mandell DL, Yellon RF, Bradley JP, et al. Mandibular distraction for micrognathia and severe upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2004;130:344-348.
28. Li KK, Powell NB, Riley RW, Guilleminault C. Distraction osteogenesis in adult obstructive sleep apnea surgery: a preliminary report. J Oral Maxillofac Surg. 2002;60:6-10.
29. Wang X, Wang XX, Liang C, et al. Distraction osteogenesis in correction of micrognathia accompanying obstructive sleep apnea syndrome. Plast Reconstr Surg. 2003;112:1549-1557.