Distal Pancreatectomy
Preoperative Evaluation
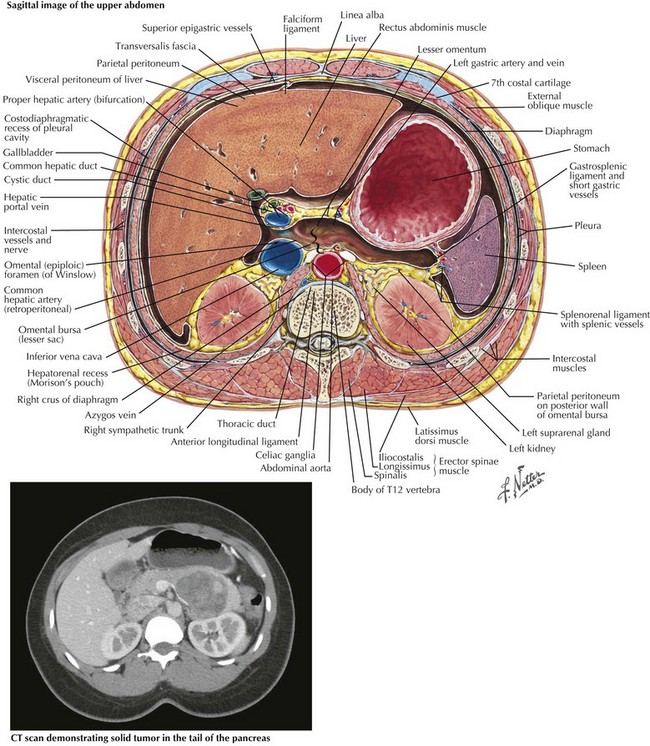
The indication for distal pancreatectomy will dictate preoperative workup and also influence surgical decision making. Multidetector, dynamic, contrast-enhanced computed tomography (CT) is the preoperative imaging modality of choice for all indications and is essential to surgical planning. CT provides detailed images of the pancreatic pathology and its relationship to surrounding organs, major vasculature, and pancreatic ducts, as well as the presence of metastatic disease (Fig, 15-1). Other modalities, such as endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS), may also be helpful when a definitive mass is not well visualized.
Surgical Approach
Open Retrograde Distal Pancreatectomy with Splenectomy
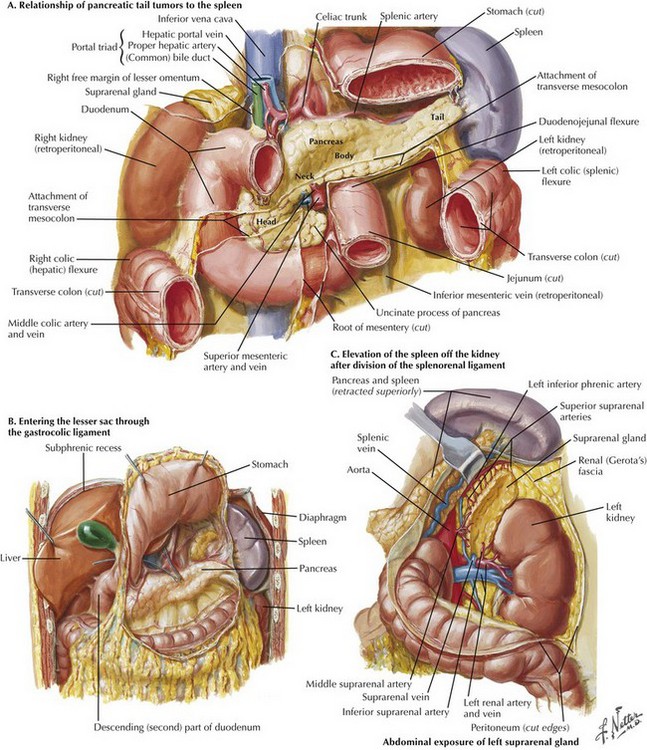
Retrograde distal pancreatectomy with splenectomy is the standard procedure for management of proven or suspected cancers in the body and tail of the pancreas, to ensure the adequacy of the lymph node dissection, or with tumors when the anatomic constraints dictate sacrificing the spleen (Fig. 15-2, A).
The pancreas is approached by opening the lesser sac through the gastrocolic ligament below the gastroepiploic vessels (Fig. 15-2, B). The peritoneum overlying the inferior border of the pancreas is divided lateral to the superior mesenteric vessels toward the tail. The splenocolic and splenorenal attachments are divided to mobilize the spleen anteriorly and to the right, separating it from splenic flexure of the colon and from Gerota’s fascia (Fig. 15-2, C).
Division of Splenic Artery and Vein
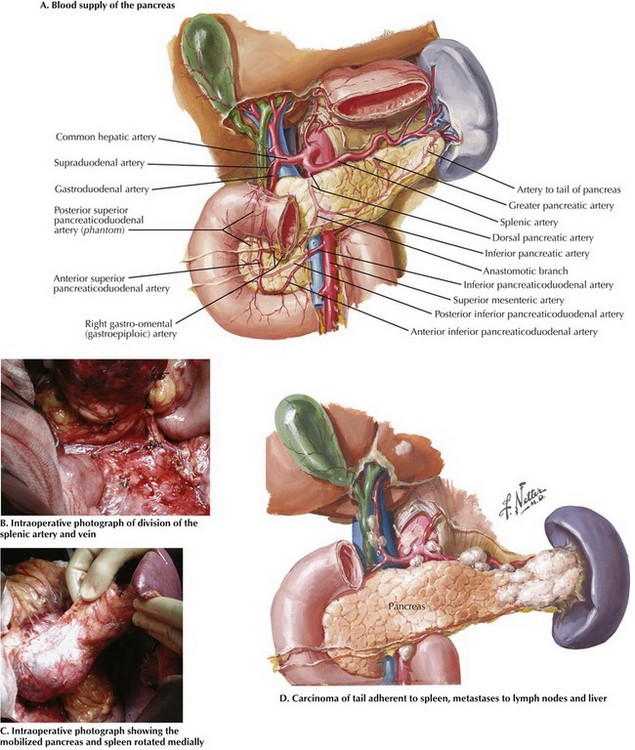
Understanding the vascular anatomy of the pancreas is essential to safe technique (Fig. 15-3, A). The splenic artery is identified at its origin from the celiac trunk and traced distally along the posterosuperior border of the pancreas. It is divided just distal to its origin. The splenic vein is then isolated and divided just proximal to its confluence with the portal vein, preserving the inferior mesenteric vein if possible (Fig. 15-3, B).
Division of Pancreas
The pancreas is rotated medially and the point of transection determined based on the location of the tumor. The pancreatic parenchyma may be divided using one of several techniques, including a gastrointestinal stapler or electrocautery. If well visualized, the pancreatic duct is oversewn (Fig. 15-3, C and D).
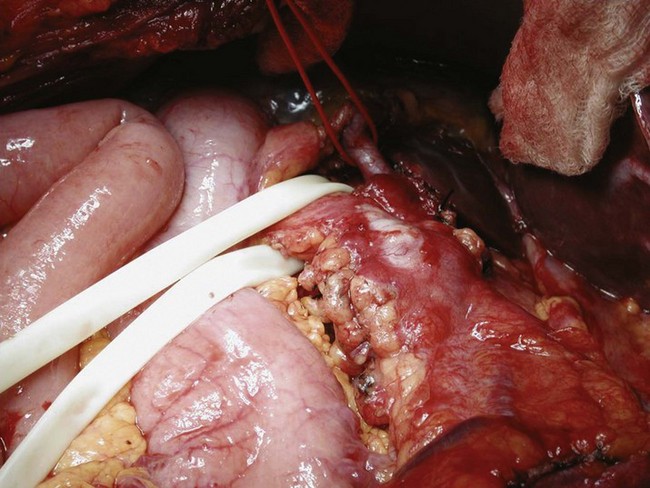
Radical Antegrade Modular Pancreaticosplenectomy
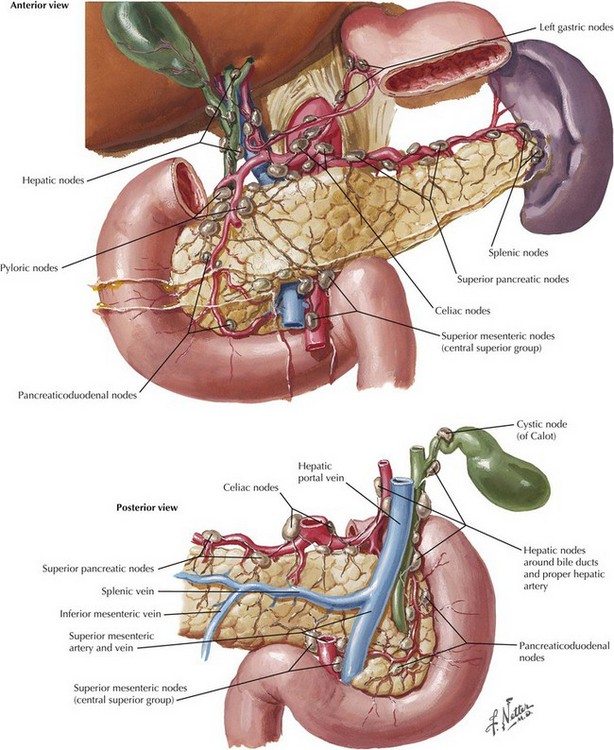
The goals of pancreatic resection for cancer should be to perform a complete resection with clear margins and resection of regional lymph nodes (Fig. 15-4). Radical antegrade modular pancreaticosplenectomy (RAMPS), described by Strasberg in 2003, is a modified technique of distal pancreatectomy developed to allow for en bloc resection of the pancreas with an N1 lymphadenectomy. With this approach, dissection proceeds from medial to lateral (right to left), removing all nodal tissue surrounding the body and tail of the pancreas.
Distal Pancreatectomy with Splenic Preservation
An incision is then made along the superior edge of the pancreas to the left of the gastroduodenal artery. A plane is then developed between the portal vein and the neck of the pancreas by gentle blunt dissection. Once the opening is complete, a Penrose drain can be passed under the neck of the pancreas for anterior traction (Fig. 15-5). This facilitates mobilization of the splenic vein away from the proximal body of the pancreas. The small, fragile venous branches from the pancreatic parenchyma to the splenic vein should be divided. A distance of 2 to 3 cm is dissected laterally. The neck of the pancreas is divided, sparing the splenic vessels.
Laparoscopic Distal Pancreatectomy
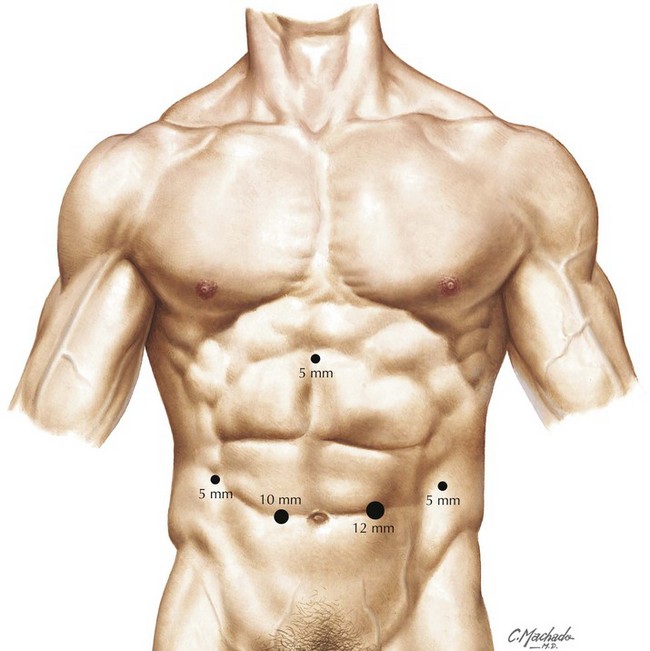
Trocar Placement for Laparoscopic Approach
Five ports are placed (Fig. 15-6); a 10-mm supraumbilical port is placed just to the left of midline. After the abdomen is insufflated, a 10- to 12-mm port is placed in the left midclavicular line, a 5-mm port in the subxiphoid area, a 5-mm trocar in the left anterior axillary line, and a 5-mm port in the right midclavicular line.
Bell, RH, Denham, EW. Distal pancreatectomy. In: Clavien PA, Sarr MG, Fong Y, eds. Atlas of upper gastrointestinal and hepato-pancreato-biliary surgery. Berlin: Springer; 2007:929–947.
Fisher, WE, Andersen, DK, Bell, RH, et al. Pancreas. In Brunicardi FC, ed.: Schwartz’s principles of surgery, 9th ed, New York: McGraw-Hill, 2010.
Lillimoe, KD, Kaushal, S, Cameron, JL, et al. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999;229:693–700.
Napolitano, C, Valvano, L, Grillo, M. Distal splenopancreatectomy: indications for surgery and technical notes. In: Surgical treatment of pancreatic diseases. Milan: Springer; 2009:321–328.
Pierce, RA, Spitler, JA, Hawkins, WG. Outcomes analysis of laparoscopic resection of pancreatic neoplasms. Surg Endosc. 2007;21:579.
Root, J, Nguyen, N, Jones, B, et al. Laparoscopic distal pancreatic resection. Am Surg. 2005;71:744.
Schulick, RD, Cameron, JL, Cancer of the pancreas and other periampullary cancers. Maingot’s abdominal operations, 11th e. McGraw-Hill: New York, 2007.
Strasberg, SM, Drebin, JA, Linehan, D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133:521–527.
Warshaw, AL. Conservation of the spleen with distal pancreatectomy. Arch Surg. 1988;123:550–553.