CHAPTER 26 Displaced Intra-articular Distal Radius Fractures
PATIENT EVALUATION
Diagnostic Imaging
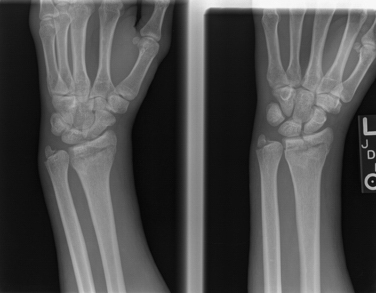
Displaced intra-articular fractures of the distal radius are a unique subset of distal radius fractures. These fractures are traditionally unstable and not amenable to traditional methods of closed manipulation and casting. It is important when evaluating a radiograph of a distal radius fracture to understand fracture patterns that may be unstable and require internal fixation. Lafontaine describes several radiographic features that signify unstable fractures of the distal radius.1 They include dorsal comminution with more than 20 degrees of dorsal tilt, extensive dorsal comminution, an associated ulnar styloid fracture, and significant intra-articular involvement in patients older than 60 years. Additional radiographic parameters include extensive dorsal comminution volar to the midaxle line of the distal radius and initial shortening greater than 4 mm of the distal radius compared with the ulna.
Arthroscopic management can further delineate these fracture lines and any associated soft tissue injuries that may involve the distal radioulnar joint and particularly the pathology of the triangular fibrocartilage complex.
Assessment of Associated Soft Tissue Injuries
Several studies have found a high incidence of intra-articular soft tissue injuries associated with displaced intra-articular fractures of the distal radius. Mohanti and Kar2 and Fontes and colleagues,3 in two separate wrist arthrography studies, identified a high incidence of injury to the triangular fibrocartilage complex associated with fractures of the distal radius.2,3 Mohanti and Kar reported a 45% incidence of tears to the triangular fibrocartilage complex in 60 patients.2 In a similar study, Fontes and coworkers found a 66% incidence of tears of the triangular fibrocartilage complex among 58 patients.3
Other arthroscopic studies have demonstrated a high incidence of injury to the triangular fibrocartilage complex. Geissler and colleagues reported their experience with 60 patients with displaced intra-articular fractures of the distal radius.4 In the series, 49% of the patients had a tear of the triangular fibrocartilage complex, most of which were peripheral and reparable. Injury to the scapholunate interosseous ligament was identified in 32%, and tears of the lunotriquetral interosseous ligament were reported in 15% of the patients.4 Landau and coworkers, in a similar arthroscopic study of 50 patients, found tears of the triangular fibrocartilage complex were the most common type and occurred in 78% of patients.5 Tears of the scapholunate interosseous ligament were identified in 54%, and tears of the lunotriquetral interosseous ligament were found in only 16% of the patients. In an arthroscopic study, Hanker reported that tears of the triangular fibrocartilage complex were present in 55% of the 65 patients in his series.6 Common in all three studies were injuries of the triangular fibrocartilage complex in which ulnar-sided pathology was most commonly associated with displaced intra-articular fractures of the distal radius.
Geissler and associates described an arthroscopic classification of interosseus ligament injuries based on their experience with the arthroscopic management of intra-articular distal radius fractures.4 They observed that a spectrum of interosseous ligament injury occurred. The interosseous ligament stretches and attenuates, and it eventually tears from a volar to dorsal direction from increased rotation between the carpal bones. The classification of carpal instability is based arthroscopic observation of the interosseous ligament from the radiocarpal and midcarpal spaces, and it evaluates injuries to the scapholunate and lunotriquetral interosseous ligaments (Table 26-1).
TABLE 26-1 Geissler Arthroscopic Classification of Carpal Instability
| Grade | Description | Management |
|---|---|---|
| I | Attenuation or hemorrhage of the interosseous ligament is seen from the radiocarpal joint. There is no incongruence of carpal alignment in the midcarpal space. | Immobilization |
| II | Attenuation or hemorrhage of interosseous ligament is seen from the radiocarpal joint. Incongruence or step-off is seen from the midcarpal space. A slight gap (less than width of a probe) between the carpal bones may be present. | Arthroscopic reduction and pinning |
| III | Incongruence or step-off of carpal alignment is seen in the radiocarpal and midcarpal spaces. The probe may be passed through the gap between the carpal bones. | Arthroscopic or open reduction and pinning |
| IV | Incongruence or step-off of carpal alignment is seen in the radiocarpal and midcarpal spaces. Gross instability with manipulation is identified. A 2.7-mm arthroscope may be passed through the gap between the carpal bones. | Open reduction and repair |
TREATMENT
Management of Carpal Instability
Geissler grade I injuries are consistent with a typical wrist sprain, and these tears respond to a short period of immobilization. Geissler grade II and III injuries may be easily arthroscopically reduced and stabilized in an acute situation. Anatomic reduction of the carpal interval is best viewed with the arthroscope in the midcarpal space opposite to the tear. For example, correction of the rotation to scapholunate instability is best viewed with the arthroscope in the ulnar midcarpal portal. For lunotriquetral instability, the reduction is best viewed with the arthroscope in the radial midcarpal portal. The carpal interval is reduced, and Kirschner wires are placed across the involved interval in oscillation mode to protect the cutaneous nerves. Geissler grade IV injuries have complete detachment of the interosseous ligament, and open repair is recommended for the best prognosis in acute situations.
Arthroscopic Techniques
A patient who sustains a fracture of the distal radius usually presents with a swollen wrist. Because of the swelling, it is usually difficult to palpate the extensor tendon landmarks traditionally used for arthroscopy. However, the bony landmarks are usually easily palpated, and they include the bases of the metacarpals, the ulnar head, and the dorsal lip of the radius.7
Intra-articular fractures of the distal radius are usually associated with abundant fracture hematoma and debris.8 Thorough irrigation of the fracture hematoma is required to evaluate the fracture fragments and to improve the field of view to judge rotation to the fracture fragments. Inflow may be provided through the wrist arthroscopic cannula or through a 14-gauge needle inserted into the 6-U portal. The small cannula used in wrist arthroscopy does not allow much space between the cannula itself and the arthroscope to allow fluid irrigation into the wrist joint. Because of this, separate inflow through the 6-U portal is recommended. Outflow is provided through the arthroscopic cannula with, intervenous extension tubing that drains into a basin on the hand table so the fluid does not go into the surgeon’s lap or onto the floor. Separate inflow and outflow cannulas limit fluid extravasation into the soft tissues.
The ideal timing for arthroscopically assisted reduction of intra-articular distal radius fractures is usually between 3 and 10 days.9 Other attempts at arthroscopic fixation may result in troublesome bleeding, which may obscure visualization. Fractures more than 10 days old may be difficult to disimpact and mobilized percutaneously.
Indications and Operative Setup
Intra-articular fractures of the distal radius without extensive metaphysial comminution are best for arthroscopically assisted management.10 They include radial styloid fractures, die-punch fractures, and three- and four-part fractures.
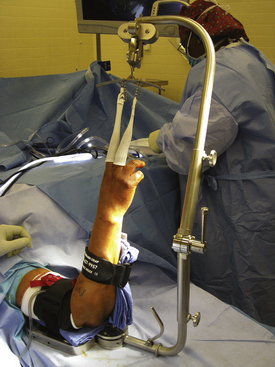
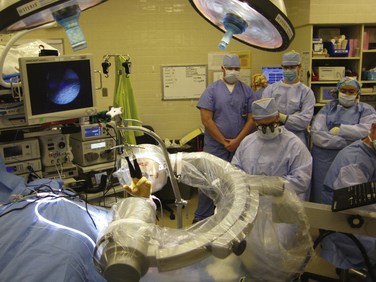
A traction tower is very useful in arthroscopic management of distal radius fractures. The traction tower allows the surgeon to flex, extend, and radial and ulnar deviate the wrist to facilitate reduction of the fracture fragments while maintaining constant traction for visualization. Previous towers suspended the wrist using a traction bar and extended the forearm and hand, which made simultaneous fluoroscopic evaluation of the reduction very difficult. A newer traction tower design allows the surgeon to simultaneously arthroscopically reduce the intra-articular fracture of the distal radius and monitor the reduction fluoroscopically. The traction bar is uniquely placed at the side of the wrist rather than at the center, so it does not block fluoroscopic visualization. The wrist can be manipulated in traction to help reduce the fracture fragments. The tower may be flexed to allow the surgeon to perform wrist arthroscopy in the vertical or horizontal plane, depending on the surgeon’s preference. If a traction tower is not available, the wrist may be suspended with finger traps in a shoulder holder or over the end of a hand table. A small bump may be placed in the volar aspect of the wrist to help maintain slight wrist flexion when weights are being used over the end of the hand table.
Injuries Treated Arthroscopically
Three-Part Fractures without Metaphysial Comminution
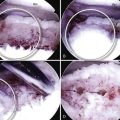
Displaced three-part fractures involve radial styloid and lunate facet fracture fragments (Fig. 26-1). The radial styloid fragment usually can be reduced by closed manipulation (Fig. 26-2). The radial styloid fragment is reduced and provisionally stabilized with Kirschner wires inserted by an oscillating drill, thereby stabilizing the styloid fragment back to the radial shaft. The wrist is then suspended in a traction tower, and the fracture debris and hematoma are evacuated (Figs. 26-3 to 26-5). The reduced radial styloid fragment may be used as a landmark to reduce the depressed lunate facet fracture fragment (Fig. 26-6). The arthroscope is placed in the 3-4 portal, and an 18-gauge needle is placed percutaneously into the radiocarpal space over the depressed lunate facet fragment. A large Kirschner wire may then be placed about 2 cm proximal to the previously placed 18-gauge needle, and it is used to elevate the depressed lunate facet fragment (Fig. 26-7). A bone tenaculum can further reduce the fracture gap between the fragments. Guidewires are placed transversely from the radial styloid just beneath the articular surface into the lunate facet fragment after the fracture fragments are anatomically reduced, as confirmed arthroscopically (Figs. 26-8 to 26-10). If a dorsal die-punch fragment is present, it is important to aim the transverse wires dorsally to capture and stabilize this dorsal fragment.

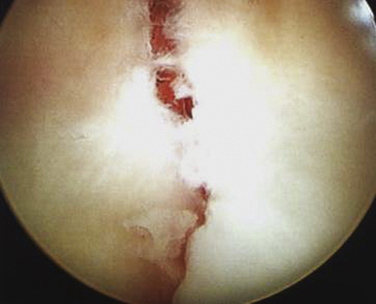
FIGURE 26-5 Washing out the fracture hematoma and debris can improve visualization. A separate inflow is provided through a needle through the 6-U portal, and outflow is provided through an extension through the arthroscopic cannula.
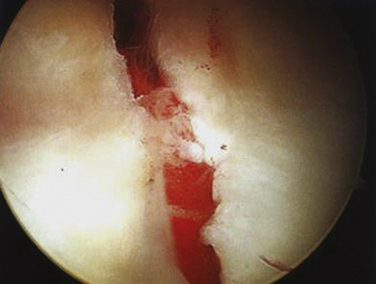
FIGURE 26-6 The depressed lunate facet fragment is identified with the arthroscope in the 3-4 portal.
After placement of the transverse guidewires, the forearm is pronated and supinated to ensure the guidewires have not violated the distal radioulnar joint. Headless cannulated screws may then be placed over the guidewires to stabilize the radial styloid fragment and the impacted lunate facet fragment. Typically, one headless screw is used to stabilize the radial styloid fragment (Figs. 26-11 and 26-12). One or two headless screws placed volar and dorsal to the radial styloid screw may then be placed to stabilize the lunate facet fragment. Further stabilization of the lunate facet fragment may be performed by adding bone graft through a small incision placed between the fourth and fifth dorsal compartments to avoid late settling of the fracture fragments. Cancellous allograft bone chips or bone substitutes may be used.
Three- and Four-Part Fractures with Metaphysial Comminution
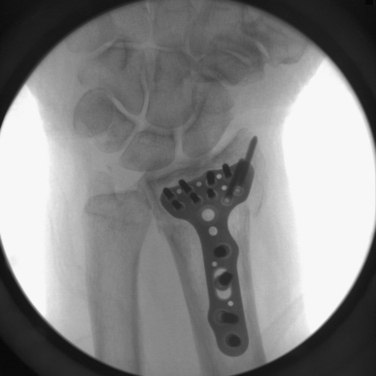
In four-part fractures, the lunate facet is divided into volar and dorsal fragments (Figs. 26-13 and 26-14). The volar ulnar fragment is reduced under direct observation through the volar approach, reducing it back to the shaft into the radial styloid fragment, and it is provisionally pinned (Fig. 26-15). The volar distal radius plate is used to provisionally stabilize the radial styloid and volar ulnar fragments (Figs. 26-16 and 26-17). The wrist is then suspended in the traction tower. With the arthroscope in the 6-R portal, the dorsal lunate fragment is visualized and percutaneously elevated (Fig. 26-18). After the articular surface is anatomic as seen arthroscopically, the provisional fixation is advanced from volar to dorsal aspects to provisionally stabilize the dorsal fragment (Figs. 26-19 and 26-20). The distal screws are then placed in the volar plate (Figs. 26-20 and 26-21).
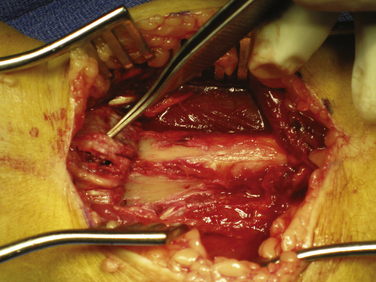
FIGURE 26-15 The intraoperative view shows reduction of the radial styloid and the volar ulnar fragment back to the radial shaft.
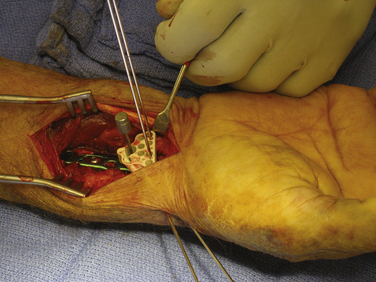
FIGURE 26-16 The Acu-Loc (Acumed, Hillsboro, OR) is placed through the volar incision. The fracture is provisionally stabilized with Kirschner wires placed through the radial styloid and the plate to support the articular surface reduction.
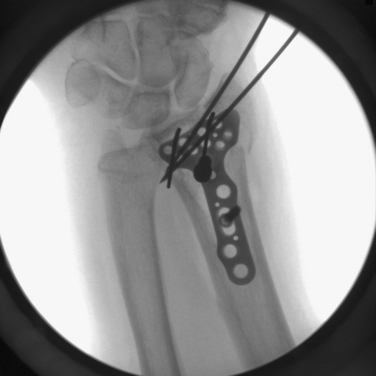
FIGURE 26-17 The fluoroscopic view demonstrates the provisional articular reduction to the distal radius.

FIGURE 26-19 The arthroscopic view with the arthroscope in the 6-R portal shows displacement of the dorsal ulnar fragment.
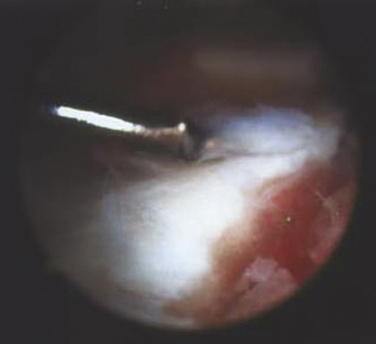
FIGURE 26-20 The arthroscopic view shows reduction of the dorsal ulnar fragment back to the volar ulnar fragment as viewed with the arthroscope in the 6-R portal.
Volar plate stabilization using wrist arthroscopy as an adjunct to view the articular reduction is preferred if metaphysial comminution is present. This produces a very stable construct and enables early range of motion and rehabilitation compared with the use of Kirschner wires or headless screws alone. Late settling of the fracture fragments is likely to be seen with volar plate stabilization compared with percutaneous Kirschner wires or cannulated screws.
Information gained from arthroscopic evaluation of the wrist after stabilization of the distal radius fracture provides some rationale about when to stabilize an associated ulnar styloid fragment (Fig. 26-22), although recommendations about the timing are controversial. After anatomic reduction of a distal radius fracture, the tension of the articular disk is palpated with a probe. The arthroscope is placed in the 3-4 portal, the probe is inserted through the 6-R portal, and the tension of the disk is evaluated. Most fibers of the triangular fibrocartilage complex are still attached to the base of the ulnar and not to the displaced ulnar styloid fragment when there is good tension on the articular disk when it is palpated. A peripheral tear of the triangular fibrocartilage complex is suspected if there is loss of tension on the disk when palpated. A peripheral tear often is covered with hematoma or synovitis, and the hematoma must be débrided to obtain direct visualization of the periphery of the articular disk.
PEARLS& PITFALLS
OUTCOMES
Wrist arthroscopy takes advantage of its ability to view the articular surface under bright light and magnified conditions. Two millimeters of articular displacement has become an established criterion for congruency of the distal radius over the past several years. Knirk and Jupiter demonstrated the importance of an articular reduction of the distal radius within 2 mm or less.11 Patients whose articular reduction was greater than 2 mm at the final follow-up visit demonstrated significantly higher incidences of degenerative changes within their wrists. Bradway and Amadio reported similar findings.12
Fernandez and Geissler reported their series of 40 patients and observed that the critical threshold might be 1 mm or less.13 They reported that the complication rate was substantially lower when the articular reduction was 1 mm or less. Trumble and colleagues, in their review of 52 intra-articular distal radius fractures, found that the factors that most strongly correlated with a successful outcome included the amount of residual radial shortening and articular incongruence.14
Edwards and colleagues described the advantage of viewing intra-articular reduction by wrist arthroscopy compared with monitoring by fluoroscopy alone.15 In their series of 15 patients who underwent arthroscopic evaluation of the articular surface after reduction and stabilization under fluoroscopic guidance, 33% of patients still had an articular step-off of 1 mm or more. Frequently, the fracture fragment was rotated. They found that wrist arthroscopy was particularly useful in judging rotation of the fracture fragments, a situation that is not readily identifiable under fluoroscopy alone. It is easy to judge rotation of the fracture fragment by looking across the wrist. For example, to judge rotation of a radial styloid fragment, it is best to place the arthroscope in the 4-5 or 6-R portal. Similarly, to view reduction of a lunate facet fragment, it is best to place the arthroscope in the 3-4 portal to view reduction of the die-punch fragment. Fractures of the dorsal lip may be viewed with the arthroscope in the 6-R portal or the volar portal.
The literature is sparse regarding the results of arthroscopically assisted fixation of displaced intra-articular fractures of the distal radius. Stewart and coworkers compared 12 open and 12 arthroscopically assisted reductions of comminuted AO type C fractures of the distal radius.16 The arthroscopically treated group had five excellent results, six good results, and one fair result. The open group had no excellent results. The investigators found that the arthroscopic group had increased range of motion compared with the group that underwent open stabilization for similar fracture patterns.
Doi and colleagues reported a similar comparison of 38 patients who underwent arthroscopically assisted fixation or open reduction and fixation.17 They reported results similar to those of earlier studies, and they observed that the arthroscopic group had improved range of motion compared with the group that underwent open stabilization.
Ruch and coworkers compared 15 patients who underwent arthroscopically assisted reduction and 15 patients who underwent closed reduction and external fixation.18 Of the 15 patients who underwent arthroscopic reduction, 10 patients had a tear of the triangular fibrocartilage complex, seven of which were peripheral and were stabilized. No patients in the arthroscopic group had any signs of instability of the distal radioulnar joint at the final follow-up visit. In contrast, 4 of the 15 patients who were managed by external fixation alone continued to complain about instability of the distal radioulnar joint. These patients potentially had a peripheral tear of the triangular fibrocartilage complex at the time of fracture that was not repaired.
Geissler and coworkers reported the results of 33 patients who underwent arthroscopically assisted reduction of extra-articular distal radius fractures.10 In their series, 25 patients had anatomic reduction of the articular surface, and 8 patients had a 1-mm step-off. They analyzed the results based on associated soft tissue injuries and found that a Geissler grade II injury of the scapholunate interosseous ligament did not affect the final prognosis. However, for patients with a Geissler grade III or IV tear and an AO type C fracture, the final result was significantly affected by the soft tissue injury.
CONCLUSIONS
Wrist arthroscopy has proved to be a valuable adjunct in the management of intra-articular distal radius fractures. Wrist arthroscopy allows visualization of the articular reduction under bright light and magnified conditions. Wrist arthroscopy combined with volar plating enables precise reduction of the articular surface, stabilization of the volar plate, and early range of motion. The importance of anatomic restoration of the articular surface has been confirmed by several studies.11,12,14 Arthroscopic lavage of fracture hematoma and debris also can improve the patient’s final range of motion. Studies by Stewart and associates16 and Doi and colleagues17 showed improved range of motion in patients who underwent arthroscopic reduction compared with those who underwent open reduction alone.
Wrist arthroscopy enables detection and management of the soft tissue injuries that frequently are associated with intra-articular fractures of the distal radius.2–6,18,19 Arthroscopic findings can establish the grade of severity of the injury and determine the type of surgical management needed for these soft tissue injuries.
It is much easier to manage an acute soft tissue lesion with a better prognosis than to undertake reconstruction of a chronic injury. Tears of the triangular fibrocartilage complex are the most common type of soft tissue injury associated with fractures of the distal radius.20 This may explain why some patients continue to complain of persistent ulnar-sided wrist pain despite an anatomic articular reduction seen on plain radiographs.
Wrist arthroscopy can help the surgeon in determining when and when not to stabilize a displaced large ulnar styloid fragment. When the articular disk is lax after restoration of the articular distal radius surface and no peripheral tear of the articular disk is identified, consideration should be given to stabilization of a large ulnar styloid fragment.
1. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210.
2. Mohanti RC, Kar N. Study of triangular fibrocartilage of the wrist joint in Colles fracture. Injury. 1979;11:311-324.
3. Fontes D, Lenoble E, DeSomer B, et al. Lesions ligamentaires associus aux fractures distales du radius. Ann Chir Main. 1992;11:119-125.
4. Geissler WB, Freeland AE, Savoie FH, et al. Carpal instability associated with intraarticular distal radius fractures. In: Proceedings of the American Academy Orthopedic Surgeons Annual Meeting. San Francisco, CA: American Academy Orthopedic Surgeons; 1993.
5. Lindau T. Treatment of injuries to the ulnar side of the wrist occurring with distal radial fractures. Hand Clin. 2005;21:417-425.
6. Hanker GJ. Wrist arthroscopy in distal radius fractures. In: Proceedings of the Arthroscopy Association North America Annual Meeting. Albuquerque, NM: Arthroscopy Association; 1993.
7. Geissler WB, Savoie FH. Arthroscopic techniques of the wrist. Mediguide Orthop. 1992;11:1-8.
8. Geissler WB. Arthroscopically assisted reduction of intra-articular fractures of the distal radius. Hand Clin. 1995;11:19-29.
9. Geissler WB. Intraarticular distal radius fractures: the role of arthroscopy. Hand Clin. 2005;21:407-416.
10. Geissler WB, Freeland AE. Arthroscopically assisted reduction of intraarticular distal radial fractures. Clin Orthop Relat Res. 1996;327:125-134.
11. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-658.
12. Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1989;71:839-847.
13. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg. 1991;16:375-384.
14. Trumble TE, Schmitt SR, Vedder NB. Fractures affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19:325-340.
15. Edwards CCIII, Harasztic J, McGillivary GR, Gutow AP. Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am. 2001;26:1036-1041.
16. Stewart NJ, Berger RA. Presented at the 53rd Annual Meeting of the American Society for Surgery of the Hand (Programs and Abstracts), January 11, 1998; Scottsdale, AZ. Comparison study of arthroscopic as open reduction of comminuted distal radius fractures. 1998.
17. Doi K, Hattori T, Otsuka K, et al. Intra-articular fractures of the distal aspect of the radius arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999;81:1093-1110.
18. Ruch DS, Vallee J, Poehling GG, et al. Arthroscopic reduction versus fluoroscopic reduction of intra-articular distal radius fractures. Arthroscopy. 2004;20:225-230.
19. Mudgal CS, Jones WA. Scapholunate diastasis: a component of fractures of the distal radius. J Hand Surg Br. 1990;15:503-505.
20. Hollingworth R, Morris J. The importance of the ulnar side of the wrist in fractures of the distal end of the radius. Injury. 1976;7:263.