Chapter 23. Disorders of the wrist and hand
Rheumatoid arthritis
Wrist
Rheumatoid arthritis affects synovium and the large amount of synovium around the wrist and inferior radioulnar joints makes them especially vulnerable to the disease.
Clinical features
The disease follows the usual pattern. The joint is painful and swollen in the acute attack but then subsides. If the disease cannot be controlled, the mass of synovium on the dorsum of the hand engulfs the extensor tendons and all may rupture (Fig. 23.1).
 |
| Fig. 23.1
Late rheumatoid arthritis of the wrist and carpus. Note that the carpal bones have fused and the wrist is ankylosed in flexion.
|
The tendons which cross the joint also become eroded and eventually rupture. The extensor tendon of the little finger is usually the first to go, but the extensor pollicis longus can also rupture where it runs around Lister’s tubercle at the lower end of the radius (Fig. 23.2 and Fig. 23.3). Later the ligaments stretch, bone collapses, the joint becomes unstable and a characteristic deformity develops, with the wrist radially deviated and supinated on the forearm and the fingers in ulnar deviation.
 |
| Fig. 23.2
Rheumatoid of the hands with synovial swellings and ulnar deviation.
|
 |
| Fig. 23.3
Rheumatoid of the hand: (a) postoperative with correction of m.c.p. joints, synovectomy of wrist; (b) with associated psoriasis in palm.
|
Treatment
Conservative treatment with anti-inflammatory drugs and rest is usually effective but if the synovitis cannot be controlled medically, surgery is needed for the following indications:
1. Synovectomy to remove painful and inflamed synovium if it cannot be controlled by conservative means.
3. If the lower end of the ulna is unstable it must be excised before it damages the tendons that cross the wrist.
4. Arthrodesis if the wrist joint is unstable. Note: Arthrodesis limits flexion and extension of the wrist only, leaving pronation and supination unaffected.
5. Replacement arthroplasty.
Although arthrodesis is contraindicated in multiple joint disease (p. 298), arthrodesis of the wrist in rheumatoid arthritis produces a good result. If both wrists are to be arthrodesed, care should be taken not to fix them both in extension. With both wrists dorsiflexed it is difficult to fasten buttons and personal hygiene is almost impossible. Hold both your own wrists in dorsiflexion and see how inconvenient it is.
Hand
Rheumatoid arthritis of the hand presents many problems and much disability. The disease usually presents with symmetrical painful swelling of the metacarpophalangeal joints caused by synovial proliferation, and is often first visible as in-filling of the valleys between the metacarpal heads (Fig. 23.4). The small joints are destroyed later and fixed deformities develop (Fig. 23.5).
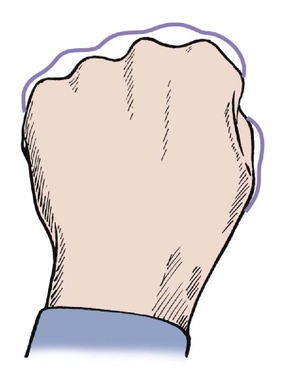 |
| Fig. 23.4
Filling of the ‘valleys’ between the metacarpal heads in rheumatoid arthritis.
|
 |
| Fig. 23.5
(a) Rheumatoid arthritis of the hand with destruction of the small joints. (b) Late rheumatoid arthritis of the hand with fixed hyperextension of the first interphalangeal joint and fixed adduction of the first m.c.p. joint.
|
Treatment
Management of the rheumatoid hand is almost a specialty in its own right.
Initial treatment is conservative, with resting splints, occupational therapy and drugs, and is best conducted by a rheumatologist. If rest, night splints and anti-inflammatory drugs do not control symptoms or induce remission, surgical synovectomy may be necessary to remove exuberant synovium from the metacarpophalangeal joints. This will relieve pain but there is no evidence that it minimizes joint destruction.
If conservative measures fail, operation must be considered. This entails a careful and thorough assessment of the patient’s disability and a critical estimate of the likely benefit from operation.
Operation is done neither because the disease is there nor because the operation is possible, but to produce a specific improvement in function.
There are several indications for operation:
1. To repair ruptured tendons by using a ‘spare’ tendon, such as the extensor indicis proprius, or by attaching the ruptured tendons to those that remain intact to produce a common extensor action.
2. To salvage destroyed metacarpophalangeal joints by replacement arthroplasty.
3. To correct other deformities, including the swan-neck deformity that results from tightness of the intrinsic muscles and damage to the volar plate and flexor digitorum sublimis. Dislocation of the extensor tendons may also need correction (Fig. 23.6).
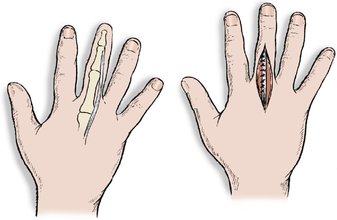 |
| Fig. 23.6
Tendon displacement in rheumatoid arthritis. The extensor tendon can slip off the back of the m.c.p. joint and may need to be replaced.
|
Osteoarthritis
Wrist
Osteoarthritis of the wrist is usually the late result of trauma, often a fractured scaphoid, and causes pain and stiffness of the wrist after use (Fig. 23.7).
 |
| Fig. 23.7
Osteoarthritis of the wrist with narrowing of the radiocarpal joint following perilunate dislocation.
|
Treatment
If the symptoms only occur when the patient is working, a firm wrist support may be sufficient. If this is not effective, arthrodesis is needed. A trial period in plaster before operation will allow the patient to assess the likely result and be convinced that pronation and supination really are possible with the wrist fused.
Hand
The trapeziometacarpal joint is affected by osteoarthritis and causes pain on gripping and twisting movements (Fig. 23.8). The joint is tender on palpation, abduction of the thumb is limited, and longitudinal pressure reproduces the symptoms.
 |
| Fig. 23.8
Advanced osteoarthritis of the first carpometacarpal joint.
|
Treatment
Conservative treatment includes a support to splint the thumb, anti-inflammatory drugs and restriction of activity. If these measures are unsuccessful, operation may be required.
Fingers
Generalized osteoarthritis of the interphalangeal joints produces unsightly osteophytic lumps at the margins of the interphalangeal joints (Fig. 23.9). These are called Heberden’s nodes if they involve the distal interphalangeal joints and Boucher’s nodes if they involve the proximal interphalangeal joints. They are different from the swelling of the interphalangeal joints seen in rheumatoid arthritis.
 |
| Fig. 23.9
Osteoarthritis of the hand.
|
Treatment
No operative treatment is helpful but physiotherapy may improve function.
Disorders of tendons
De Quervain’s tenosynovitis
The extensor pollicis brevis and the abductor pollicis longus pass beneath a tight fibrous bridge just proximal to the radial styloid process and repeated stressing of these tendons by wringing out dish cloths or other twisting movements can cause a localized tenosynovitis (Fig. 23.10). The tendon swells, movements become painful and the fibrous bridge becomes thickened and forms a firm swelling on the lateral side of the radius just proximal to the wrist, which can be alarming. The tendon sheaths sometimes become inflamed above and below the fibrous bridge and make a soft creaking sound with movement.
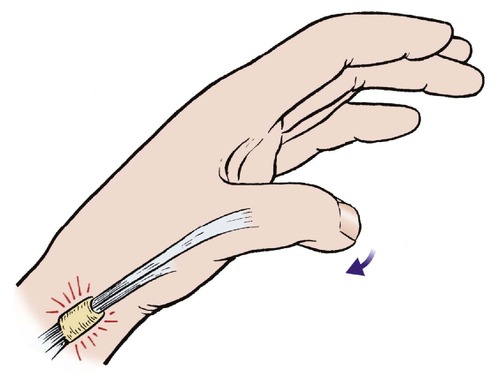 |
| Fig. 23.10
De Quervain’s disease. The extensor pollicis brevis and abductor pollicis longus tendons are irritated as they pass beneath a fibrous bridge proximal to the radial styloid.
|
The diagnosis can be confirmed by stressing the tendons. Ask the patient to grasp the thumb with the other fingers and then push the hand gently into flexion and ulnar deviation. This stretches the affected tendons and reproduces the pain.
Treatment
If elimination of the activity which caused the condition does not produce relief, steroid injection into the tendon sheaths can be helpful. If this is ineffective, the fibrous bridge must be divided surgically.
Extensor tenosynovitis
The extensor tendons, which do not have a tendon sheath, are less vulnerable to tenosynovitis than the flexors but the paratenon can become inflamed. Affected tendons produce the creaking, leathery sensation of muffled crepitus as they move.
Treatment
Rest and splintage are usually effective but steroid injection is sometimes necessary.
Trigger finger
The flexor profundus longus tendon is subjected to friction where it enters its tendon sheath and swelling can occur on the tendon at this point (Fig. 23.11). As the swelling enters the tendon sheath it irritates the opening of the sheath and this can narrow it still further. A vicious circle is therefore established, with the swelling aggravating the constriction and vice versa.
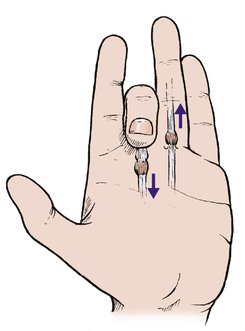 |
| Fig. 23.11
Trigger finger. Triggering is caused by a swelling on the flexor tendon catching as it moves in and out of the opening into the fibrous flexor sheath.
|
Clinical features
The swelling on the tendon prevents the tendon moving easily and causes a ‘pop’ as it enters the tendon sheath. The flexors are stronger than the extensors and the tendon becomes stuck in the flexed position. Extension is only possible passively, when it will straighten with a click.
This phenomenon is known as ‘triggering’ and is usually worse first thing in the morning after sleeping with the fingers flexed but improves during the day as soft tissue swelling subsides.
Treatment
The symptoms usually follow unaccustomed repetitive activity and settle with rest and elimination of the cause. If this is ineffective a steroid injection into the tendon sheath is needed.
If the symptoms persist after three injections, the fibrous opening of the flexor tendon sheath must be incised to ease the passage of the tendon swelling. The operation is effective, but only required if all conservative measures have failed.
Trigger thumb
The same phenomenon can occur at the thumb, which can become locked in flexion. The lesion is also seen in infancy, usually before the age of 2.
Treatment
Most can be cured by injection of the tendon sheath with hydrocortisone but open release of the tendon sheath may be needed in children if the condition has not resolved by the age of 4.
Ganglia
A ganglion is a collection of thick fluid, similar to synovial fluid, surrounded by a thin layer of synovium in the soft tissues around joints and tendons. Although these cysts are called ganglia they have no connection with the nervous system.
Synovial fluid is produced by synovial cells, which normally secrete synovial fluid into the joint space. If the cells secrete fluid into the soft tissues rather than the joint cavity then a ganglion results (Fig. 23.12).
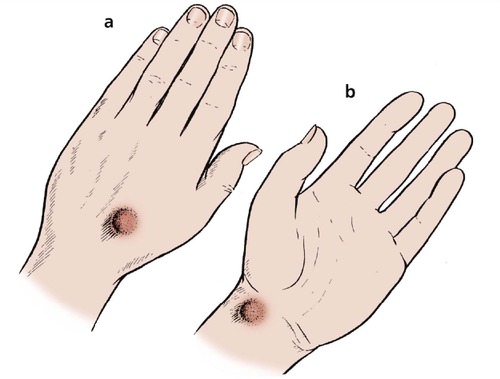 |
| Fig. 23.12
Ganglia at the wrist: (a) on the dorsum of the hand; (b) on the volar aspect of the wrist, beside the radial artery.
|
The lesions can form around any joint or tendon sheath but do not communicate with the joint space. Some extend inside the sheaths of peripheral nerves and cause peripheral nerve damage. Others extend deep to periosteum and involve bone.
Clinical features
Ganglia usually appear in early adult life and are particularly noticeable on the back of the wrist, associated with the scapholunate ligament. They also occur on the front of the wrist, where they emerge between the flexor tendons and the radial artery.
Ganglia vary in size, ache after the hand is used, and interfere with its function.
Treatment
Ganglia sometimes rupture or disappear spontaneously after an accidental blow or, according to medical folklore, being ‘hit with the family Bible’. If they do not disappear spontaneously and interfere with function, excision is required.
If the ganglion is causing neurological problems, early excision is indicated. If not, operation is best deferred for as long as possible because:
1. The scar is often more unsightly than the ganglion.
2. The soft tissue swelling at the site of operation can be almost as large as the original ganglion and takes up to 6 months to resolve.
3. A new ganglion may form in the place of the original because the area of abnormal synovium produces many small ganglia rather than a single large one.
4. Wide excision of the tissue at the base of the ganglion is needed to minimize the risk of recurrence and the operation causes more discomfort than patients expect.
Pearl ganglia
A variation of the common ganglion occurs in the midline of the flexor tendon sheaths where the fibres decussate opposite the metacarpophalangeal and interphalangeal joints (Fig. 23.13). These ganglia are small, round, tense and painful when gripping hard objects such as a steering wheel.
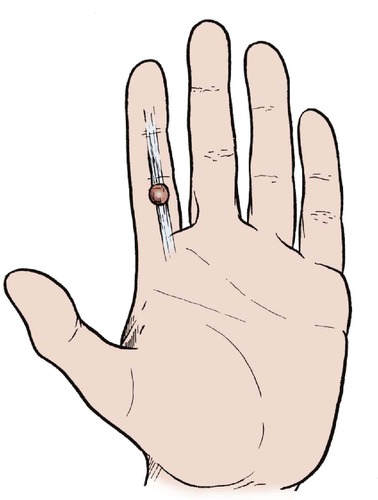 |
| Fig. 23.13
Pearl ganglion – a small tense ganglion may develop on the volar aspect of the flexor sheath at the level of the joint.
|
Treatment
Pearl ganglia often rupture and disappear after a simple puncture with a hypodermic needle, but they sometimes need excision. At operation they resemble a pearl and have a thin wall. Recurrence is unusual.
Ganglia at the distal interphalangeal joint
Mucous cysts are also seen at the distal interphalangeal joint, where they interfere with the nail bed and sometimes extend into the pulp of the finger. They are unsightly and interfere with the function of the finger.
Treatment
These ganglia seldom respond to conservative treatment and excision may be necessary. They frequently recur.
Infection
Infection in the hand is a serious matter. The function of the hand depends upon smooth soft tissues sliding over each other and anything that causes adhesions between the ‘moving parts’ has serious consequences. Infection of the hand can be classified as follows:
Infections of the hand
• Nail fold infections (paronychia).
• Pulp space infections or ‘whitlow’.
• Web space infections.
• Infections of the tendon sheaths.
• Infections of the deep spaces.
Nail fold infections
Infections of the nail fold, or paronychia, is a common problem (Fig. 23.14). The infection begins with a break in the skin of the nail fold and spreads from there to the subungual space, where it causes severe pain by raising tissue tension. The lesion is seen less often now than in the past, perhaps because people keep their hands cleaner.
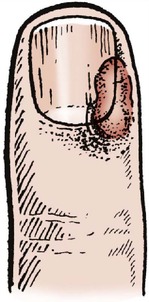 |
| Fig. 23.14
Site of pus in paronychia.
|
Treatment
The lesion should be cleaned, antibiotics administered and the hand elevated (Fig. 23.15). Unless there is a rapid improvement, the edge of the nail should be raised and the pus evacuated, or the proximal half of the nail removed.
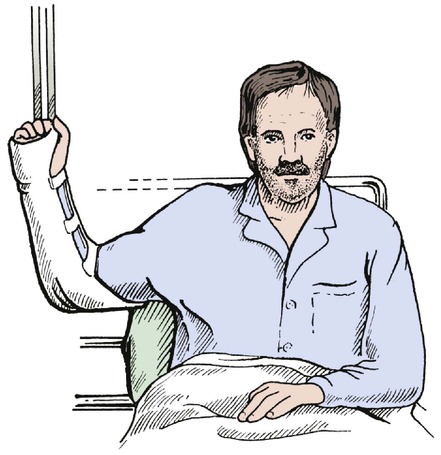 |
| Fig. 23.15
Elevation of the hand for infection.
|
This must be done under general or regional anaesthesia; local anaesthetics or ring blocks must never be used in the presence of infection because the injection helps spread the infection.
Pulp space infections
Pulp space infections, often referred to by the ancient name of ‘whitlow’, usually begin with a penetrating injury (Fig. 23.16).
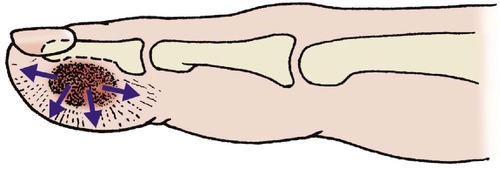 |
| Fig. 23.16
Pulp space infection (whitlow). The spread of pus is limited by fibrous septa and the increased tissue tension causes pain.
|
The pulp has many stout, fibrous septa, which make the pulp of the finger firm but also prevent soft tissue swelling. This in turn means that even a small collection of pus causes severe pain, particularly if the digit is accidentally knocked. The expression ‘sticking out like a sore thumb’ refers not only to the appearance of the thumb but also to the excruciating pain of a pulp space infection.
Treatment
Treatment is similar to that of paronychia. If rest, antibiotics and elevation do not bring rapid relief, the pus should be released through a transverse or oblique incision in the side of the pulp and not through a ‘fish mouth’ incision across the end of the pulp.
Herpetic whitlow
Herpes simplex can cause infection of the pulp space and is common in healthcare workers. Incision makes the condition worse. Beware of nurses and midwives with a whitlow.
Web space infections
The web space between adjacent fingers contains loose tissue, and quite large abscesses can form with little local pain or tissue tension (Fig. 23.17). Penetrating injury is the usual cause.
 |
| Fig. 23.17
Web space infection.
|
Treatment
If elevation and adequate antibiotics do not bring rapid relief, a short incision is needed to drain the pus.
Infection of the tendon sheaths
Tendon sheaths infected by spread from the pulp or by penetrating injuries provide an easy route for bacterial spread. The finger quickly becomes painful and is held in slight flexion because the volume of the sheath is greatest in this position. Any movement is excruciating. The extent of the infection is dictated by the anatomy of the tendon sheaths (Fig. 23.18).
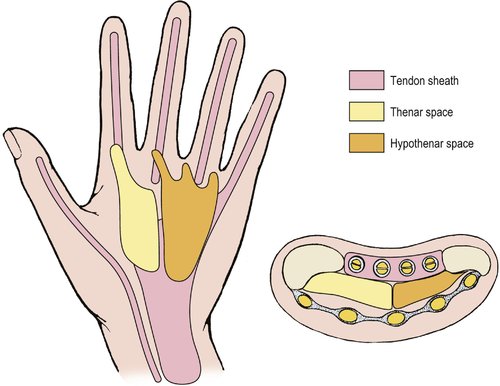 |
| Fig. 23.18
Tendon sheaths and deep spaces in the palm and fingers. Infection is confined to these spaces initially.
|
Treatment
The consequences of adhesions in the tendon sheath are worse than paronychia or pulp space infections and more energetic treatment is needed. The patient must be admitted, the arm elevated and antibiotics given in adequate doses. Intravenous antibiotics are advisable.
Unless there is a response within 6 h, the tendon sheath should be opened at each end and then irrigated.
Infection of the deep spaces
There are two spaces in the hand, the thenar and hypothenar spaces, bounded by fascial sheaths that act as bulkheads to prevent the spread of infection (see Fig. 23.18). Infection can follow spread from infection in adjacent structures, penetrating injury, or spread from the web space by way of the lumbricals.
The pain and clinical signs are less dramatic than in the infections described previously because the infection is deeper and there is more room for the infection to spread. The hand is diffusely swollen, finger movement is restricted, and deep pressure over the infected space is painful.
Treatment
The patient should be admitted, the arm elevated and antibiotics given intravenously. Unless there is a rapid response, the appropriate space should be decompressed by an experienced hand surgeon who is familiar with the detailed anatomy of these spaces.
Dupuytren’s disease (or ‘contracture’)
In 1831, Baron Dupuytren, a surgeon in Paris, described a contracture of the hand which begins at the base of the ring or little finger and eventually pulls them into extreme flexion, making it difficult to put on gloves or shake hands (Fig. 23.19). The position of the fingers suggested the contracture was caused by holding the reins of a horse but the condition has survived the horse-drawn carriage and its cause is still unknown.
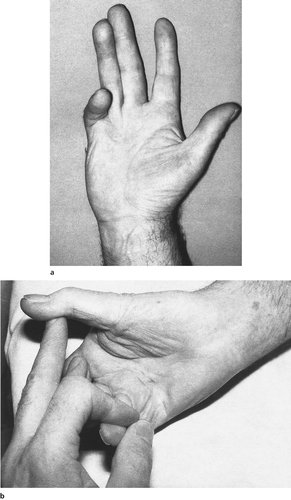 |
| Fig. 23.19
(a) Dupuytren’s contracture affecting the little finger; (b) the thumb is also involved.
|
Pathology
The basic pathology is contracture of the palmar fascia, similar to other fibrous diatheses such as Peyronie’s disease and retroperitoneal fibrosis. The contracture can also involve the skin.
Clinical features
The condition is very often symmetrical, is commoner in men, may run in families, and is associated with diabetes, epilepsy and alcoholism. The soles of the feet may develop fibrous nodules similar to plantar fibromatosis, and pads of firm fibrous tissue (Garrod’s pads) are sometimes seen on the dorsum of the knuckles.
Treatment
There is no effective conservative treatment but the symptoms are not always incapacitating and slight deformities are best left untreated, especially in elderly patients.
Surgical correction is possible by excising the contracted tissue, which is hard and almost cartilaginous in consistency. The success of operation depends on the extent of the contracture and the joints involved. Because of their anatomy (p. 33), the metacarpophalangeal joints can be easily straightened, even if they have been flexed for many years, while the interphalangeal joints quickly stiffen in flexion.
Even if full movement is restored, the contracture can recur or extend as the disease progresses. There is no need to advise operation as long as the patient has no disability and the interphalangeal joints are not involved. There are two indications for operation:
1. More than 30° contracture of the interphalangeal joints.
2. Disability from involvement of the metacarpophalangeal joints.
If the deformity is severe and cannot be corrected, it may be necessary to amputate the affected digit, usually the little finger, through the neck of the metacarpal.
Kienböck’s disease
Osteochondritis of the lunate is described on page 328; it may cause pain in the wrist on gripping and at the extremes of the range of movement. A firm splint is usually helpful and operation is seldom needed.
Neurological disorders
Sensory and motor disturbances in the hand are common and differential diagnosis is often difficult. The symptoms may involve the arm as well, but the conditions are described here because they usually present with symptoms in the hand. The following conditions account for the great majority of cases (Fig. 23.20).
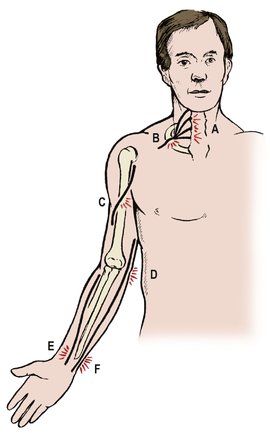 |
| Fig. 23.20
Sites of neurological lesions in the arm: ( A) cervical spondylosis; ( B) thoracic outlet; ( C) radial nerve damage; ( D) ulnar nerve compression ( E) median nerve compression; ( F) ulnar nerve damage.
|
Common causes of neurological abnormalities in the upper limb
• Ulnar compression at the elbow.
• Ulnar nerve compression at the wrist.
• Median nerve compression at the wrist (carpal tunnel syndrome).
• Radial nerve lesions.
• Cervical spondylosis.
• Thoracic outlet syndrome.
• Combined lesions.
Ulnar nerve compression
Causes
The ulnar nerve may be compressed where it runs behind the medial epicondyle of the humerus at the elbow (Fig. 23.21). The symptoms are worse with the nerve under tension when the elbow is flexed; prolonged flexion of the elbow when reading or asleep precipitates symptoms.
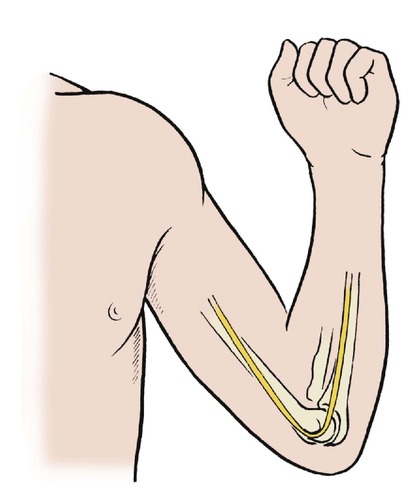 |
| Fig. 23.21
The ulnar nerve runs behind the medial epicondyle and may be irritated after prolonged full flexion.
|
The condition may arise because of an abnormal valgus angle at the elbow following a supracondylar fracture of the humerus in childhood (p. 200). As the child grows, the valgus deformity increases, the ulnar nerve is stretched and the symptoms develop. This condition is still known by the quaint title of ‘tardy ulnar palsy’.
Any other abnormality on the medial side of the elbow, whether the result of trauma or osteoarthritis, may also cause ulnar nerve compression. The symptoms also arise without obvious cause.
Clinical features
The characteristic symptoms are tingling, pain and numbness in the ulnar nerve distribution, which includes the little finger, the ulnar half of the ring finger and the medial side of the hand. The patient may also notice weakness, clumsiness and wasting of the interossei in severe cases.
On examination there is diminished sensibility in the ulnar distribution and sometimes wasting of the intrinsic muscles of the hand. In severe cases the ulnar two or three digits are held in the classic main-en-griffe (claw hand) position associated with loss of intrinsic power.
The ulnar nerve is palpable at the elbow and is sometimes sensitive to light finger pressure. If pressing the nerve does not reproduce the symptoms, the diagnosis can be confirmed by nerve conduction studies, which show a delay at the elbow.
Treatment
Apart from avoiding pressure on the elbow and keeping it straight, there is no conservative treatment for ulnar nerve compression.
If the symptoms become worse, the ulnar nerve can be transposed from its vulnerable position on the convexity of the elbow to a safer place in front of the medial epicondyle. By freeing the nerve from the fibrous tunnel through which it runs behind the medial epicondyle and allowing it to take a ‘short cut’ across the elbow, the nerve is decompressed and tension is released.
Reducing pressure on the nerve prevents further deterioration but the neurological symptoms do not always recover completely and patients should be warned that the operation is to prevent the symptoms getting worse rather than to relieve them completely.
Ulnar nerve compression at the wrist
The deep parts of the ulnar nerve may be compressed at the wrist as it enters the hand through the canal of Guyon beside the pisiform. The condition is so excessively uncommon that for practical purposes all ulnar nerve problems arise at the elbow.
Treatment
If the symptoms are severe, which is unusual, and the lesion is proven by electrical studies, surgical decompression is required.
Median nerve compression (carpal tunnel syndrome)
Cause
The median nerve enters the hand through the carpal tunnel, a bony trough covered with a stout fibrous roof (the flexor retinaculum) which it shares with nine tendons, each covered with two layers of synovium (Fig. 23.22). There is no room in this tight tunnel for the tissues to expand and any swelling of the tendons or the synovium around them is bound to compress the median nerve.
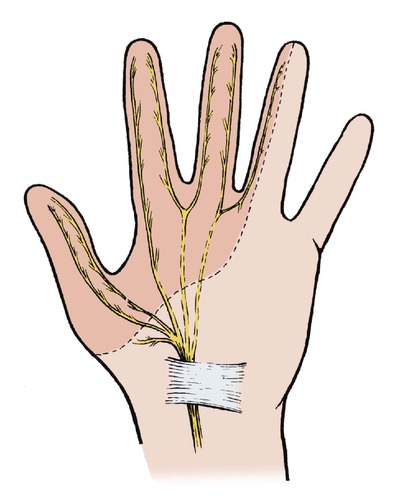 |
| Fig. 23.22
Carpal tunnel syndrome. The median nerve is compressed where it runs beneath the carpal ligament. There may be altered sensibility of the thumb, index, middle and half of the ring finger and wasting of the thenar muscles.
|
The commonest overall cause of carpal tunnel syndrome is fluid retention, of which the commonest cause is pregnancy. Overuse of the tendons from repeated forceful movements of the wrist, either at work or recreation, is probably the commonest cause of carpal tunnel syndrome referred to orthopaedic clinics. Any condition that causes synovial thickening, including rheumatoid arthritis and Colles’ fracture, can also be responsible.
Clinical features
Median nerve compression causes paraesthesia in the median nerve distribution, which in most patients is the front of the thumb, index finger, middle finger and the radial half of the ring finger. The palm is not involved because the palmar branch of the median nerve arises above the wrist.
The symptoms are worse at night and the patient will wake and fling the hand up and down to try and relieve the symptoms. In time, the paraesthesia is replaced by pain proximally as far up as the elbow, and eventually by numbness in the median distribution.
Most patients notice that the little finger is not affected and those who report that all the fingers are involved should be treated with suspicion.
Differential diagnosis
The differential diagnosis includes peripheral neuropathy, mononeuritis, cervical spondylosis and tumours of the thoracic inlet involving the brachial plexus (p. 186). These are often forgotten because carpal tunnel syndrome is such a common condition. If there is any doubt, the diagnosis can be confirmed by nerve conduction studies.
Conservative treatment
Conservative treatment consists of rest, diuretics and hydrocortisone injection.
Rest and diuretics. The carpal tunnel syndrome of pregnancy disappears after delivery and most other patients recover when the original cause has been eliminated. If symptoms persist, conservative treatment with diuretics and a resting splint at night is usually effective.
Hydrocortisone injection. Injection of hydrocortisone acetate into the carpal tunnel may be effective but if the patient is still troubled after three injections, carpal tunnel decompression is needed.
Operative treatment
Carpal tunnel decompression is a straightforward and reliable operation and recurrence is unusual. The tunnel is decompressed by dividing the flexor retinaculum throughout its length from top to bottom through a longitudinal incision.
Radial nerve lesions
In the upper arm
The radial nerve is vulnerable as it winds around the humerus and can be damaged by pressure against the medial side of the humerus in the axilla. Axillary crutches used wrongly can cause radial palsy, as can pressure against a hard object. The nerve can be compressed while dozing in an armchair or sitting with the arm resting along the back of an adjacent chair (Fig. 23.23).
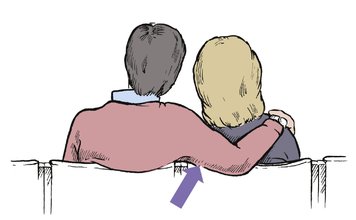 |
| Fig. 23.23
The radial nerve may be compressed by pressure on the back of a chair.
|
The characteristic symptom is weakness of the extensors, with a ‘drop wrist’ on clinical examination. There may be a small area of diminished sensibility on the back of the hand at the base of the thumb in the area supplied by the radial nerve. Paraesthesiae may be felt in the same area when the pressure is relieved.
The radial nerve may also be injured in fractures of the humerus, when the history will suggest the diagnosis.
Posterior interosseous nerve
The posterior interosseous nerve is vulnerable where it winds around the neck of the radius, as the common peroneal nerve is at the neck of the fibula. The interosseous nerve does not run between the radius and ulna, despite its name. It is comparable with the common peroneal nerve and is only called interosseous because it runs on the interosseous membrane.
The commonest cause of injury is trauma and the position of the nerve must never be forgotten when operating on the lateral side of the elbow. If the nerve is damaged at this point there will be weakness of all the wrist and finger extensors but there is seldom any sensory impairment.
Lateral cutaneous nerve of the forearm
The lateral cutaneous nerve of the forearm is also very vulnerable and its continuation into the hand has the doubtful distinction of being one of the few cutaneous nerves that can be palpated. If the extensor pollicis longus is contracted, the nerve can be felt by drawing a thumb nail along the tendon until a tingling sensation is felt in the hand.
Treatment
Operation is only required for mechanical entrapment or irritation of the nerve by adhesions or bone spurs around a fracture.
Cervical spondylosis
The cervical nerve roots can be compressed or irritated as they leave the cervical spine through the nerve root canals. Typically, the patient will have sensory symptoms confined to a single dermatome, usually the C5 or C6 dermatome (Fig. 23.24). The distribution of the sensory symptoms should point to the diagnosis but it may be hard to find any objective neurological impairment and EMG studies are often needed to exclude damage to the median, ulnar and radial nerves. The motor symptoms are usually overshadowed by the sensory symptoms. Weakness may be absent because most muscles in the forearm are innervated by several roots.
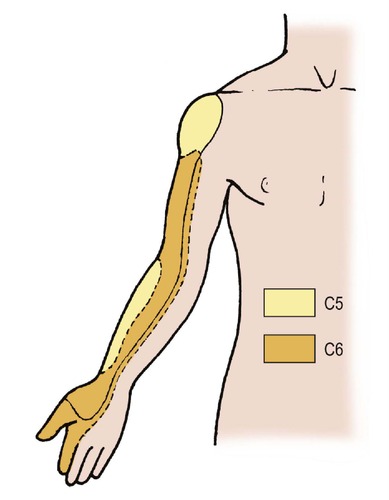 |
| Fig. 23.24
Dermatomes of C5 and C6.
|
Treatment
See page 446.
Thoracic outlet
Pressure on the lowest cervical roots as they cross the first rib or a fibrous cervical rib at the thoracic outlet can cause pain down the inner side of the forearm and hand in the T1 distribution.
Treatment
Removal of a cervical rib sometimes relieves the symptoms but the operation is best undertaken by a thoracic surgeon accustomed to operating in this region. An intrathoracic tumour can cause the same symptoms and signs.
Tumours of the thoracic inlet
Apical lung tumours can involve both the brachial plexus and cervical sympathetic chain. Although rare, it is important to consider this diagnosis and exclude it radiologically.
Combined lesions
More than one of these conditions can exist in combination and diagnosis is then more difficult. If a patient with carpal tunnel syndrome also has cervical spondylosis involving the C5 root, there will be altered sensibility on the radial side of the forearm as well as the hand and electrical studies may be helpful but not conclusive.
Treatment
In such patients it is wise to treat only one condition at a time and to stress to the patient that it will require more than one form of treatment to relieve all the symptoms. The cervical spondylosis may be relieved by physiotherapy, for example, while carpal tunnel decompression is needed to relieve carpal tunnel symptoms.
Case reports
Contractures and obvious clawing of the hand can be caused by a number of different conditions.
Patient A
A 53-year-old diabetic gentleman with a history of alcohol abuse presented in the Orthopaedic Clinic with clawing of the little and ring finger of the left hand. This had been a gradual process over the past 10 or 15 years and he had noticed a thickening of the skin in the palm of his hand.
On presentation he was unable to fully extend the fingers and it was obvious that there were nodules in the skin and tethering of the skin in the palm of the hand. The metacarpophalangeal and interphalangeal joint motion was severely restricted, but there was no loss of skin sensitivity and he had normal vascularity of the hand.
A diagnosis of Dupuytren’s contracture was made and he was referred for surgery to correct the deformity as this was impacting on his day-to-day activities.
Patient B
A 30-year-old worker had been involved in an industrial accident, sustaining a significant injury to the left elbow. He had a comminuted fracture of the distal humerus, which had been plated and this had subsequently healed. He had, however, noticed postoperatively that there was a loss of feeling on the little and ring finger of that hand and he had a clawing of these two fingers.
Examination confirmed normal median nerve sensibility, but an absence of the ulnar nerve function.
Patient C
A 46-year-old gentleman presented to the Orthopaedic Department with a catching sensation when flexing the middle finger. He was able to flex the finger, but this would catch within the palm and on extending the finger there was an audible and popping sensation in the palm. He had always been able to fully extend the finger, but over the last few weeks this had become more difficult and painful.
On examination he had a palpable nodule over the metacarpophalangeal joint and this was causing a trigger finger abnormality. When flexing the finger the nodule on the flexor tendon passed under the A1 pulley, getting trapped proximally and stopping the finger from extending fully. On forceful extension this nodule passed back through under the A1 pulley allowing the finger to extend. This was not associated with any neurovascular problems in the rest of the hand.
Summary
Clawing of the fingers of the hand can be for a number of reasons. It is important to look for general health problems including smoking, alcohol abuse or diabetes as these can be associated with Dupuytren’s contracture.
On examination of the hand it is important to identify whether there is a neural element, both motor and sensory, in the presentation. Remember that trigger fingers may be purely mechanical with neither an inflammatory process in the skin nor as a result of neurovascular problems.