102 Disorders of the Respiratory System
Etiology and Pathogenesis
Several well-defined events are necessary for the transition to extrauterine life, including establishment of spontaneous respirations, clearance of amniotic fluid from the airway, surfactant release and function, and a decrease in pulmonary vascular resistance to aid in pulmonary blood flow. Impediments to one or more of these events generally manifest as respiratory distress in the newborn. The differential diagnosis of respiratory distress in neonates is broad, and nonrespiratory etiologies are varied (Table 102-1).
Table 102-1 Differential Diagnosis of Neonatal Respiratory Distress
| System | Category | Diagnoses |
|---|---|---|
| Respiratory |
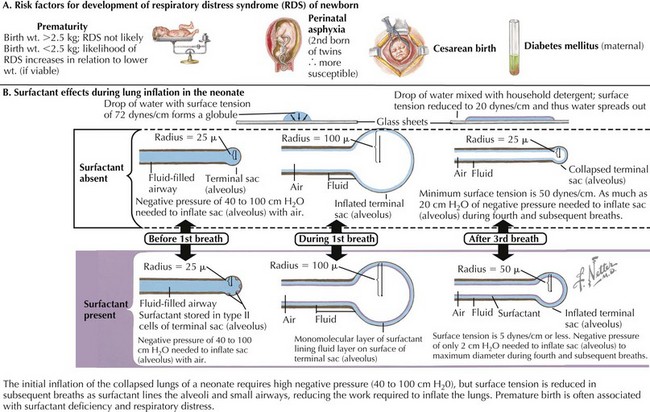
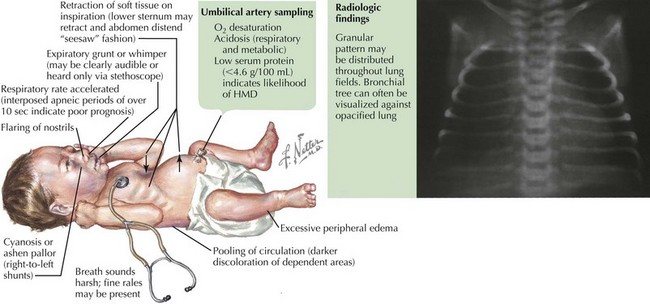
Respiratory Distress Syndrome
Respiratory distress syndrome (RDS), also known as hyaline membrane disease, is the end result of a relative surfactant deficiency that, when combined with the compliant chest wall of the neonate, promotes alveolar atelectasis and prevents newborns from developing a normal functional residual capacity (Figure 102-1). The most significant risk factor for RDS is prematurity because surfactant production begins between 24 and 28 weeks of gestation and does not become fully functional until at least 35 weeks. Other risk factors for the development of RDS include maternal diabetes; early-onset sepsis; and less commonly, congenital surfactant deficiency. Fifty percent of infants with birth weights between 500 and 1500 g develop some degree of respiratory distress; however, survival is greater than 90% with the use of exogenous surfactant and antenatal steroids.
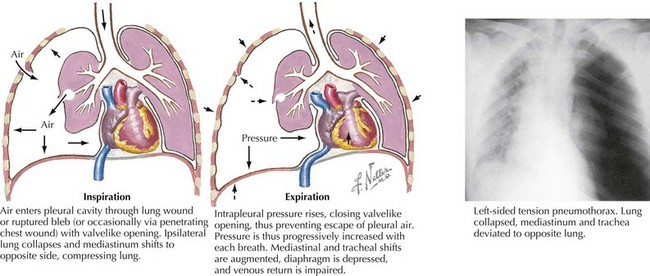
Pneumothorax
Air leak syndromes, as the name implies, result from rupture of the alveolar sac with subsequent flow of air into the interstitial spaces of the lung, and they occur in the setting of a rapid change in intrathoracic pressure. In term infants, pneumothorax is the most common result of an air leak and occurs in 1% of all deliveries (Figure 102-2). Risk factors include positive-pressure ventilation with high peak inspiratory pressures (>20–25 mm Hg) and surfactant administration. Pneumothorax may occur spontaneously at birth even without application of positive-pressure ventilation.
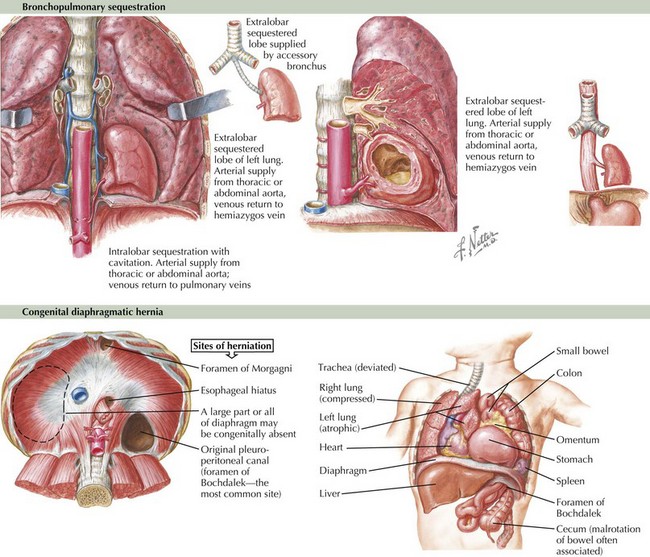
Anatomic Abnormalities
Congenital anomalies of the pulmonary system may or may not be prenatally diagnosed and include the following disorders: choanal atresia, a congenital blockage of the posterior nares; trachea-esophageal fistula; congenital diaphragmatic hernia (CDH), a patent pleuroperitoneal canal that allows the intestines to occupy the pleural space and results in pulmonary hypoplasia (Figure 102-3); congenital cystic adenomatous malformation (CCAM); bronchopulmonary sequestration, in which a segment of lung parenchyma is not supplied by the pulmonary blood supply and does not communicate with the bronchial tree (see Figure 102-3); bronchogenic cysts; congenital lobar emphysema, which results in air trapping in one lung segment; vascular rings and slings; and Pierre Robin sequence and other maxillofacial malformations. A full exploration of these disorders is beyond the scope of this chapter, but it is important to keep them in mind when faced with an infant with respiratory distress without risk factors for the more common disorders described above.
Evaluation and Management
Initial Evaluation
Chest radiography is the best test to differentiate between RDS and TTN, the most common causes of respiratory distress in newborns. Whereas fluid in the interlobar fissure, with perihilar streaking, indicates TTN, a uniform reticulogranular pattern (“ground-glass appearance”) and peripheral air bronchograms suggest RDS (Figure 102-4). Chest radiography is also useful to evaluate for pneumonia, congenital heart disease, pneumothorax, and CDH. Radiographic findings of pneumothorax are air in the pleural cavity resulting in hyperlucency with absence of pulmonary markings in the affected area. A more subtle chest radiography finding suggestive of pneumothorax is a downward displacement of the diaphragm, which can be verified with a cross-table lateral chest radiograph as an anterior mediastinal collection of air.
Dargaville PA, Copnell P, Australian and New Zealand Neonatal Network. The epidemiology of meconium aspiration syndrome: incidence, risk factors, therapies, and outcome. Pediatrics. 2006;117(5):1712-1721.
Engle WA, American Academy of Pediatrics Committee on Fetus and Newborn. Surfactant-replacement therapy for respiratory distress in the preterm and term neonate. Pediatrics. 2008;121(2):419-432.
Niermeyer S, Kattwinkel J, Van Reempts P, et al. International Guidelines for Neonatal Resuscitation: an excerpt from the Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: International Consensus on Science. Contributors and Reviewers for the Neonatal Resuscitation Guidelines. Pediatrics. 2000;106(3):e29.
Roberts D, Dalziel S: Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 3:CD004454, 2006.
Stevens TP, Harrington EW, Blennow M, Soll RF: Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev (4):CD003063, 2007.
Takaya A, Igarashi M, Nakajima M, et al. Risk factors for transient tachypnea of the newborn in infants delivered vaginally at 37 weeks or later. J Nippon Med Sch. 2008;75(5):269-273.
Wiswell TE, Gannon CM, Jacob J, et al. Delivery room management of the apparently vigorous meconium-stained neonate: results of the multicenter, international collaborative trial. Pediatrics. 2000;105(1 Pt 1):1-7.