CHAPTER 17 Disorders of the Proximal Biceps Tendon
ANATOMY
The LHB arises from the glenoid labrum and supraglenoid tubercle. It is an intra-articular but extrasynovial structure that is essentially static within the joint, sliding passively on the humeral head during elevation or rotation.1 The tendon is approximately 9 cm long and 5 to 6 mm in diameter, and the articular portion is flatter and a little larger than the groove portion.
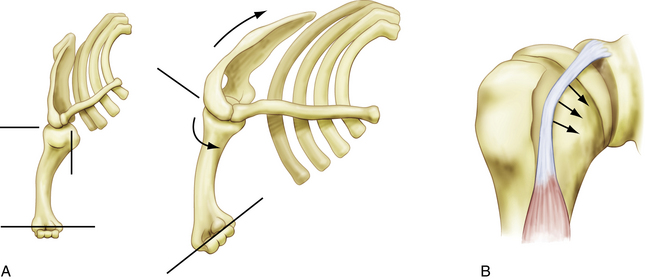
The location of the LHB just anterior to the supraspinatus tendon makes it susceptible to subacromial impingement. In addition, under load, the LHB often bears on the medial aspect of the groove, with the lesser tuberosity and soft tissues acting as a pulley (Fig. 17-1). This renders the tendon highly vulnerable to mechanical attrition and, if the soft tissue restraints of the biceps pulley become incompetent, subluxation.3
The contributions of the superior glenohumeral ligament and coracohumeral ligament to the biceps pulley mechanism are critical to the stability of the tendon. The transverse humeral ligament is not a significant stabilizer at the entry of the groove, and doubt has been expressed about its existence as a distinct entity, because it may be a continuation of the insertion of the subscapularis.4 Posteriorly, the leading edge of the supraspinatus is the primary restraint, although the anterior location of the groove and anterior vector of the pull of the tendon make this less important in most functional positions.
The function of the LHB at the shoulder is still a matter of debate. Some authors have considered it a purely vestigial structure with no true function at the glenohumeral joint, viewing it as the appendix of the shoulder. It functions as a weak abductor of the shoulder, but only when the arm is in external rotation, a position that is rarely used in activities of daily living.4,5 It has also been proposed as a depressor of the humeral head and, although some cadaver, biomechanical, and radiologic studies have supported this,6,7 electromyographic studies,8,9 clinical observation, and the long-term results of tenotomy in the presence of a rotator cuff tear10 appear to negate this role. The primary function of the biceps is at the elbow, where it acts as a flexor and supinator.
There has been recent interest in the role of the LHB in glenohumeral stability, especially following the description of superior labrum anteroposterior (SLAP) lesions,6,11–13 and mostly in the context of the throwing athlete.14,15 Anterior instability leads to increased activity in the muscle on electromyography, indicating the possible role of the biceps as a secondary glenohumeral stabilizer. However, the magnitude of this function is likely to be small.
PATHOANATOMY
Tenosynovitis, tendinosis, delamination, prerupture, and rupture probably represent the natural history of progressive degeneration of the biceps. The LHB is subject to tenosynovitis because of its anatomy, with a synovial sheath and constrained path in the bicipital groove.16–18 Arthroscopic evaluation shows fluid, adhesions, and increased vascularity around the tendon, but this must not be confused with the normal vascular pattern on the superficial surface of the tendon within the groove. Early tendinosis may be difficult to visualize arthroscopically, and may be best visualized using magnetic resonance imaging (MRI) or ultrasound imaging. Often, the tendon appears macroscopically normal, although there may be some increase in diameter. As the condition progresses, fibrillation, splits, and hypertrophy or attentuation occur, and may be described as delamination or prerupture.
Most degenerative changes in the LHB are associated with pathology of the rotator cuff, as highlighted by Neer.19 The relative importance of these structures in producing symptoms is still uncertain and will probably continue to be as long as our understanding of the mechanism of pain generation in disease of the rotator cuff remains incomplete.
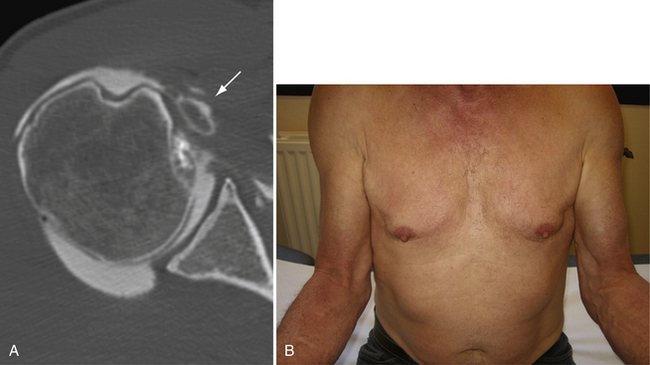
Spontaneous rupture of the LHB is usually secondary to progression of a chronic partial tear, and may happen during a movement of daily living or a minor injury. Rupture usually occurs in the presence of a cuff tear.19 The classic Popeye sign of a ruptured LHB is unmistakable, but not all rupture, or tenotomies produce this deformity.10,20 Dislocated tendons often become encased in fibrous tissue or adherent to the subscapularis before rupture, and hypertrophic tendons may become fixed within the bicipital groove, resulting in an autotenodesis. Dislocation itself may, by shortening the course of the tendon, produce a low-rising muscle belly, which we call a false Popeye sign (Fig. 17-2).
Mechanical incarceration of the tendon within the joint has been described as an hourglass biceps,21 which is often seen in association with advanced disease of the rotator cuff. The intra-articular portion becomes hypertrophic and is unable to slide into the bicipital groove, resulting in buckling of the tendon on elevation of the shoulder, with painful entrapment of the tendon between the humeral head and glenoid and a mechanical block to terminal elevation. The hypertrophic tendon may also dilate the entry to the groove and lead to subluxation.
Failure of the biceps sling leads to subluxation and eventually dislocation in the presence of a rotator cuff tear. Although the difference may be subtle, it is important to distinguish subluxation from dislocation. A subluxation is defined as a partial and/or transient loss of contact between the tendon and its groove. A dislocation is the complete and permanent loss of contact between the tendon and the groove. Dislocations of the LHB can be classified into intra-articular, intratendinous, and extra-articular subtypes, depending on its position relative to the subscapularis. In cases of subluxation and dislocation, the subscapularis is almost always torn and, most often, the supraspinatus is also torn.3 Instability of the LHB is almost always medial, but lateral instability has been described, mainly in a traumatic context in association with anterior dislocation and/or fracture of the greater tuberosity,22,23 but also in association with supraspinatus tears (see Fig. 17-2B).24
HISTORY AND PHYSICAL EXAMINATION
Spontaneous rupture of the tendon is often accompanied by retraction of the tendon and the classic Popeye deformity. With subluxation or dislocation of the tendon, the muscle belly can have the attenuated appearance of a false Popeye sign (see Fig. 17-1). A side to side comparison palpating the bicipital groove is often useful, and is felt most easily in 10 degrees of internal rotation.25 In dislocations of the LHB, the tenderness is more medial on the lesser tuberosity, and the tendon can sometimes be rolled under the fingers. We also find the Speed test (palm-up test) useful for diagnosing biceps pathology.
Patients with a dislocation of the LHB may present with a very typical clinical picture. Dislocation is often traumatic and almost always associated with a tear of the upper subscapularis. The patient presents with a loss of active elevation above 90 degrees, and it is common to find a limitation of active and passive external rotation with extra-articular and intratendinous dislocations because the dislocated biceps tendon tethers the inferior part of the subscapularis. The clinical sign of a hypertrophied and entrapped hourglass biceps is loss of the terminal 10 to 20 degrees of active and passive elevation without loss of rotation. This represents true mechanical locking of the shoulder, and should not be confused with a frozen shoulder.21
DIAGNOSTIC IMAGING
Radiographic examination should include a standard roentgenographic series (anteroposterior views in neutral, internal, and external rotation, axillary view, and supraspinatus outlet view), to rule in or out any associated abnormalities. We also find contrast studies (computed tomography [CT] arthrography, magnetic resonance [MR] arthrography) very useful to help diagnose pathology of the biceps tendon. With disruption of the medial sling, the LHB is frequently found to ride over the lesser tuberosity in a subluxated position, with a flattened appearance. With complete disruption of the sling, contrast material may escape from the biceps sheath and help outline the LHB in its dislocated position (see Fig. 17-2A).
INDICATIONS AND CONTERAINDICATIONS
Finally, a very thin, fragile LHB may be the technical limit of open or arthroscopic tenodesis. In this case, the procedure can easily be converted to a simple tenotomy. A simple tenotomy is also favored for low-demand older patients.
TREATMENT OPTIONS
Conservative Treatment
A Cochrane26 review has looked at 26 trials of physiotherapy for shoulder conditions, and concluded that there was some evidence for mobilization and exercise in rotator cuff disorders, but no trials looked specifically at pathology of the LHB. It also concluded that there was no evidence to support the therapeutic use of ultrasound or laser for this group of conditions.26 Intra-articular injections can relieve bicipital symptoms, but they may be ineffective if adhesions or synovitis restrict the dispersal of the injection into the bicipital groove. In our opinion, injections into the bicipital groove should be placed under ultrasound guidance to improve accuracy, and are particularly valuable when a subacromial injection has been ineffective in the presence of an intact rotator cuff.
Arthroscopic Treatment
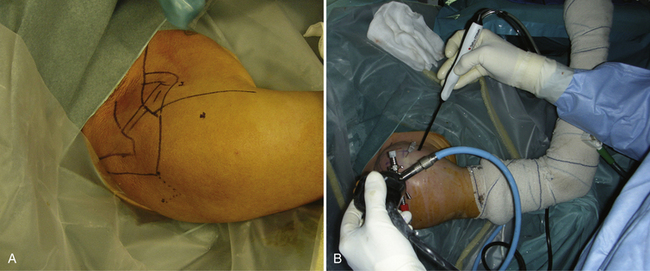
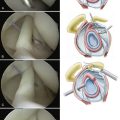
Bony landmarks are drawn on the shoulder to identify the acromion, coracoid process, and coracoacromial ligament. The procedure requires three arthroscopic portals—the classic posterior portal is created over the soft spot and two anterior portals (anteromedial and anterolateral) are created 1.5 cm on each side of the bicipital groove, 3 cm distal to the anterior corner of the acromion (Fig. 17-3A). A pump is helpful to obtain distention of the joint and the bursa but it is important to maintain low pump pressure (30 mm Hg or lower) during the procedure to prevent excessive soft tissue distension. The surgical technique is comprised of six steps, as follows.
Step 1: Glenohumeral Exploration and Tenotomy of the Long Head of the Biceps
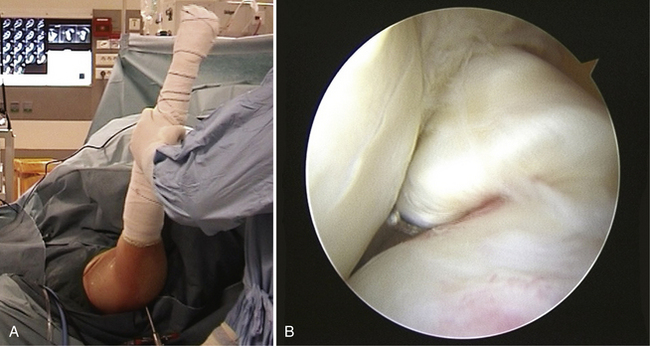
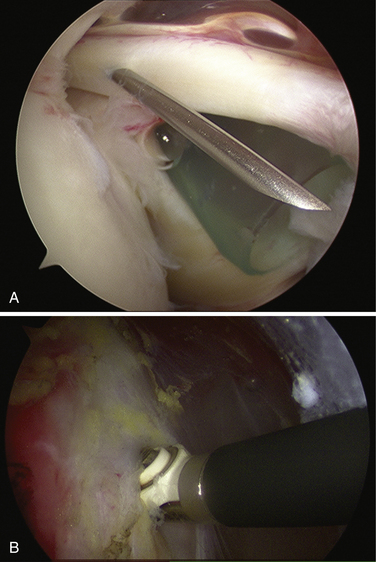
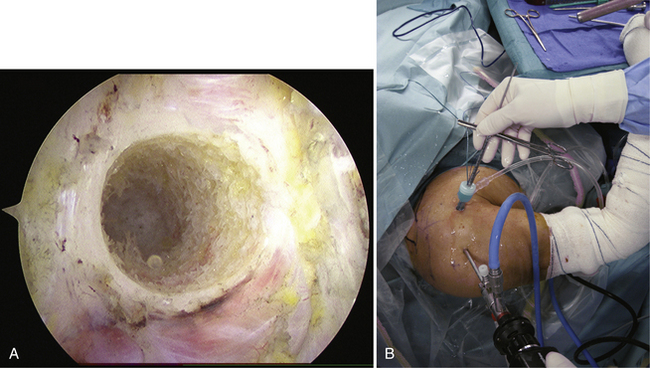
The 30-degree arthroscope is inserted through the posterior portal and a diagnostic arthroscopy of the glenohumeral joint is performed. An anteromedial portal is established using an inside-out technique, passing the trocar through the rotator interval lateral to the coracoid process, 1 cm distal to it, and just above the subscapularis tendon. An 8-mm cannula is then inserted. Biceps pathology is often in the intertubercular groove portion and it is important to draw this part of the LHB into the joint with a probe. Dynamic examination of the biceps is then performed, first with the hourglass test, in which the shoulder is elevated in the scapular plane in neutral rotation with the elbow extended (Fig. 17-4A). In a positive hourglass test, the hypertrophic tendon fails to slide in the bicipital groove and buckles in the articulation, limiting elevation (see Fig. 17-4B).21 The swinging test is then performed, in which the adducted shoulder is rotated internally and externally to look for instability of the LHB. Medial subluxation in external rotation indicates a partial- or full-thickness tear of the subscapularis tendon, whereas lateral subluxation in external rotation indicates a tear of the supraspinatus, which may be a PASTA (partial articular-sided supraspinatus tendon avulsion) lesion or a full-thickness tear.27
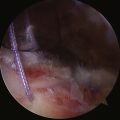
If a tenodesis is planned, the LHB is transfixed with a spinal needle intra-articularly at its entrance into the groove to avoid its retraction (Fig. 17-5A). The tendon is then detached from its glenoid insertion using a scalpel or punch, or electrocautery (see Fig. 17-5B). If a simple tenotomy is planned, it is not necessary to place a needle and the tendon is allowed to retract out of the joint. An hourglass biceps tendon may not slide out of the joint with extension of the elbow and shoulder. In such cases of autotenodesis, we simply resect the intraarticular portion of the LHB.
Step 2: Identification and Opening of the Bicipital Groove
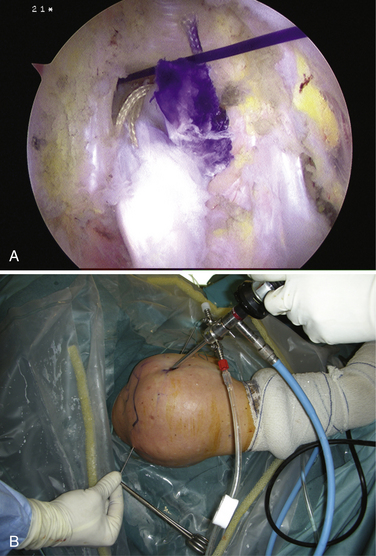
The anterolateral portal is now created. It is located 3 cm from the anterior border of the acromion and 3 cm from the anteromedial portal to allow triangulation (see Fig. 17-3A). The arthroscope is now placed in the anterolateral portal. The anteromedial cannula is removed from the joint and reoriented into the anterior subdeltoid space. At this point, the anteromedial portal is the working portal and the anterolateral portal is the viewing portal (see Fig. 17-3B). A blunt trocar is used via the anteromedial cannula to palpate the soft spot corresponding to the bicipital groove, which is found between the hard surfaces of the lesser and greater tuberosities. The trocar can be used to push the “cobwebs” of fibrous tissue off the transverse ligament gently, without disrupting the adjacent vessels, and to feel the roll of the LHB in the groove. Visualization of the white fibers of the transverse ligament and of the ascending lateral vessels also help locate the groove.
The bursa anterior to the bicipital groove is resected with a motorized shaver or the Mitek VAPR radiofrequency device (DePuy Mitek, Raynham, Mass). Anterior bursectomy is essential for visualization and is continued until the bicipital groove and overlying transverse ligament are clearly seen. It is also possible to use the spinal needle as a landmark, but we avoid doing so because there is a tendency to bleed when the dissection is carried superiorly into the vascular anterosuperior bursa. The transverse ligament is now opened in a longitudinal fashion, using a hook-tipped electrocautery or VAPR device (see Fig. 17-5B). Once the groove is open, the LHB is probed and a careful synovectomy is performed using the shaver. Now the biceps tendon is lifted out of the groove to free possible adhesions. Location of the groove is much easier when there is a large cuff tear, with the biceps being uncovered when it enters the superior part of the groove.
Step 3: Biceps Exteriorization and Preparation
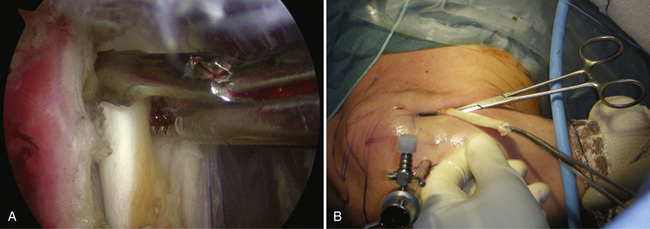
The spinal needle is removed and the elbow is slowly extended. As the proximal cut end of the LHB comes into view, it is grasped (Fig. 17-6A) and exteriorized through the anteromedial portal. Two atraumatic vascular clamps are used to grasp it progressively more distally to exteriorize as much tendon as possible. About 4 to 5 cm of tendon should be exteriorized, which is facilitated by flexion of the elbow. A single clamp is then used to keep the tendon outside for preparation (see Fig. 17-6B). Any remaining synovium is removed and, if necessary, the tendon is trimmed in the line of its fibers so that the diameter of the doubled tendon will be 8 mm.
The tendon is now doubled over a no. 2 Ethibond suture (Ethicon, Somerville, NJ) and a no. 1 polydiaxonone (PDS) suture (Ethicon). The end of the tendon is whip-stitched using a running baseball stitch with no. 1 absorbable polyglactin 910 (Vicryl) suture (Ethicon). The tendon should be doubled and sewn to its anterior face for a length of about 2 cm, where a mark is made with ink (Fig. 17-7A). The PDS suture is then tied at the end of the loop, with one end as long as possible and the other cut short. The PDS suture will later be used to guide the interference screw and screwdriver into the humeral socket. The no. 2 Ethibond suture is left passing through the doubled tendon loop unsecured; it will later be used to pull the tendon into the socket and subsequently removed after the tendon is fixed.
The diameter of the double tendon is measured using the same type of graft sizer used in anterior cruciate ligament (ACL) reconstruction. The size of the double tendon determines the drill diameter needed to drill the humeral socket and should be 7 or 8 mm. The prepared tendon is then kept outside the wound and held by an assistant or clamped to the drapes. The rest of the procedure is performed with the arthroscope in the anterolateral (viewing) portal and the instruments inserted through the anteromedial (working) portal (see Fig. 17-7B).
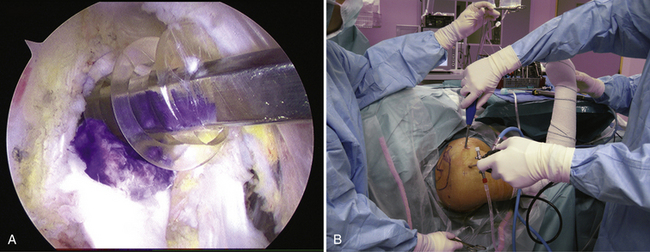
Step 4: Drilling the Humeral Socket
The location of the humeral socket is initially penetrated with a sharp-tipped awl to prevent skiving of the guide pin when drilling. A guidewire is then placed in the pilot hole and oriented strictly perpendicular to the humerus and parallel to the lateral border of the acromion (Fig. 17-8). The guidewire is drilled until it engages the posterior cortex of the humerus. The humeral guide pin is overdrilled with a cannulated reamer the same size as the doubled tendon (7 or 8 mm), to a depth of 25 mm, and the reamer and guide pin are removed. The shaver, VAPR, and an arthroscopic burr are used via the anteromedial portal to chamfer smooth the edges of the socket entrance and remove bone debris and tissues that may block or abrade the tendon (Fig. 17-9A). Most attention is paid to the inferior part of the humeral socket, where the tendon will enter.
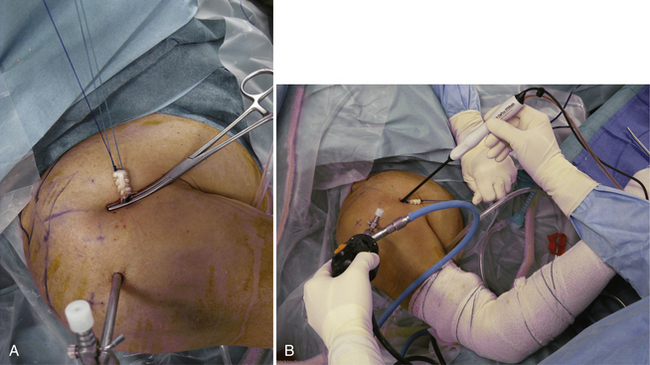
Step 5: Passing the Transhumeral Pin
A Beath pin pull-through technique is used for tendon placement. This pin has an eyelet on its trailing end and serves as a suture passer. The Beath pin is placed through the anteromedial cannula into the humeral socket. To centralize the pin, we place the reamer in the socket in a reversed orientation, removing it once the pin has been advanced (see Fig. 17-9B). The direction of the transhumeral Beath pin is important; it should be strictly perpendicular to the humerus and parallel to the lateral border of the acromion. The pin is drilled until it exits the skin, which will be approximately 2 cm inferior and 2 cm medial to the posterolateral border of the acromion, avoiding the axillary nerve (Fig. 17-10A).28,29 Both ends of the Ethibond suture are threaded through the eyelet of the Beath pin, and the pin and sutures are pulled through the humerus. The PDS suture is not passed posteriorly, because it will later be used to guide the screw into the socket. The tendon is checked for twists and, if necessary, reoriented with a probe or grasper. The Ethibond suture is used to pull the doubled loop of biceps tendon into the humeral socket. The ink mark at the base of the doubled portion of the tendon should pass just inside the socket (see Fig. 17-10B).
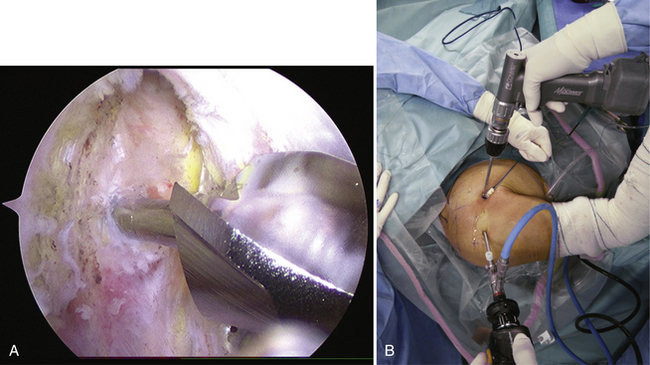
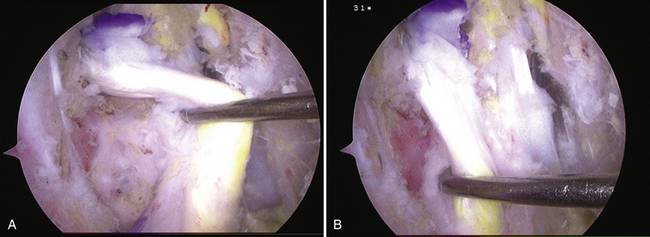
Step 6: Interference Screw Fixation
The tendon is fixed in the socket using a 9- × 20-mm bioabsorbable interference screw. As a general rule, we use an interference screw that is 0.5 mm larger than the socket diameter. The screws are bioabsorbable poly-L-lactic acid (PLA 98) and are smooth so as not to damage the tendon (Tenoscrew, Phusis; Tornier, Stafford, Tex). After the cannula is removed, the screw is passed over the PDS suture into the anterior subdeltoid space and placed on the superior aspect of the tendon (Fig. 17-11A). The elbow remains flexed at 90 degrees initially to avoid overtensioning the LHB (see Fig. 17-11B). Once the tip of the screw is engaged in the socket, the elbow is extended to tension the tendon and prevent twisting while the screw is advanced. After complete insertion of the screw, tension and fixation are checked by probing the tendon in flexion and extension (Fig. 17-12). Tensioning of the biceps is usually optimal because the intra-articular part of the tendon is placed in the humeral socket instead of being in the joint.
PEARLS& PITFALLS
PEARLS
SUMMARY
Pathology of the long head of the biceps brachii is increasingly recognized as an important cause of shoulder pain and dysfunction. Although the most appropriate management of the diseased tendon has been the subject of controversy, removal of the intra-articular portion, by tenotomy or tenodesis, is increasingly accepted. It is now recognized that the functional role of the LHB tendon at the shoulder is limited, so surgeons should be aware that retaining a pathologic tendon has a more negative functional consequence than loss of the tendon itself.
1. Hitchcock HH, Bechtol CO. Painful shoulder; observations on the role of the tendon of the long head of the biceps brachii in its causation. J Bone Joint Surg Am. 1948;30:263-273.
2. Balg F, Boulianne M, Boileau P Bicipital groove orientation: considerations for the retroversion of a prosthesis in fractures of the proximal humerus. J Shoulder Elbow Surg, 15; 2006:195-198.
3. Walch G, Nove-Josserand L, Boileau P, Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998;7:100-108.
4. Gleason PD, Beall DP, Sanders TG, et al The transverse humeral ligament: a separate anatomical structure or a continuation of the osseous attachment of the rotator cuff. Am J Sports Med, 34; 2006:72-77.
5. Furlani J. Electromyographic study of the m. biceps brachii in movements at the glenohumeral joint. Acta Anat (Basel). 1976;96:270-284.
6. Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121-130.
7. Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am. 1995;77:366-372.
8. Yamaguchi K, Riew KD, Galatz LM, et al Biceps activity during shoulder motion: an electromyographic analysis. Clin Orthop Relat Res, 336; 1997:122-129.
9. Levy AS, Kelly BT, Lintner SA, et al Function of the long head of the biceps at the shoulder: electromyographic analysis. J Shoulder Elbow Surg, 10; 2001:250-255.
10. Walch G, Edwards TB, Boulahia A, et al Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg, 14; 2005:238-246.
11. Andrews JR, Carson WGJr., McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337-341.
12. Pagnani MJ, Deng XH, Warren RF, et al Role of the long head of the biceps brachii in glenohumeral stability: a biomechanical study in cadavera. J Shoulder Elbow Surg, 5; 1996:255-262.
13. Kim SH, Ha KI, Kim HS, Kim SW. Electromyographic activity of the biceps brachii muscle in shoulders with anterior instability. Arthroscopy. 2001;17:864-868.
14. Itoi E, Kuechle DK, Newman SR, et al. Stabilising function of the biceps in stable and unstable shoulders. J Bone Joint Surg Br. 1993;75:546-550.
15. Youm T, El Attrache NS, Tibone JE, et al. The effect of the long head of the biceps on glenohumeral kinematics. J Shoulder Elbow Surg. 2009;18:122-129.
16. Post M, Benca P. Primary tendinitis of the long head of the biceps. Clin Orthop Relat Res. 1989;246:117-125.
17. Pfahler M, Branner S, Refior HJ. The role of the bicipital groove in tendopathy of the long biceps tendon. J Shoulder Elbow Surg. 1999;8:419-424.
18. Neviaser TJ. Arthroscopy of the shoulder. Orthop Clin North Am. 1987;18:361-372.
19. Neer CS2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am, 54; 1972:41-50.
20. Boileau P, Baque F, Valerio L, et al. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747-757.
21. Boileau P, Ahrens PM, Hatzidakis AM Entrapment of the long head of the biceps tendon: the hourglass biceps—a cause of pain and locking of the shoulder. J Shoulder Elbow Surg, 13; 2004:249-257.
22. Freeland AE, Higgins RW. Anterior shoulder dislocation with posterior displacement of the long head of the biceps tendon. Arthrographic findings. A case report. Orthopedics. 1985;8:468-469.
23. Bauer T, Vuillemin A, Hardy P, Rousselin B Posterior dislocation of the long head of the biceps tendon: a case report. J Shoulder Elbow Surg, 14; 2005:557-558.
24. Walch G. Pathology of the long head of the biceps. Cahiers d’enseignement de la SOFCOT. 1993;45:57-69.
25. Matsen FA3rd, Kirby RM. Office evaluation and management of shoulder pain. Orthop Clin North Am. 1982;13:453-475.
26. Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;2:CD004258.
27. Jacquot N, Boileau P. Can the long biceps be healthy in rotator cuff tears? Epidemiology and dynamic behavior. Rev Chir Orthop. 2007;5:S30-S31.
28. Burkhead WZSR, Box G. Surgical anatomy of the axillary nerve. J Shoulder Elbow Surg. 1992;1:31-36.
29. Wolf EM. Anterior portals in shoulder arthroscopy. Arthroscopy. 1989;5:201-208.