Chapter 24. Disorders of the hip and knee
Osteoarthritis of the hip
Clinical features
Osteoarthritis of the hip is one of the commonest causes of disability in the western world. The condition is essentially mechanical wearing out of the hip joint rather than a disease and can be caused by many things. Trauma, obesity and previous infection can all be followed by osteoarthritis but there is probably a genetic element as well. The disease is much less often seen in Asiatic races.
The characteristic symptoms are:
1. Pain.
2. Loss of hip movement.
3. Abnormal gait.
Pain. The pain is worse on weight-bearing and movement of the hip but also occurs at rest and disturbs sleep. The pain is dull and aching in character at first but becomes sharper as the disease progresses.
The pain is usually felt in the groin but pain down the outer side of the thigh is also common. Some patients also have pain low in the thigh, around the knee, and become convinced that the trouble lies in the knee, not the hip. Referred pain of this type is a well-known diagnostic pitfall but still confounds the unwary.
Loss of movement. Movement is lost because osteophytes form around the joint and change the shape of the joint surfaces. As movement is lost, a flexion, adduction and external rotation deformity develops. The flexion deformity is compensated for by hyperextension of the lumbar spine, and this can cause backache. The adduction deformity causes apparent shortening of the leg and patients often complain that ‘my leg is getting shorter’.
The stiffness makes it difficult to tie shoe-laces, put on socks or cut toenails.
Abnormal gait. The limp is due partly to the restriction of movement in the joint, and partly to an antalgic gait (p. 25); i.e. walking so that the load on the hip joint is reduced. The limp is usually observed by other people rather than the patient but a few are more worried by the limp than anything else.
Clinical examination
Patients with osteoarthritis of the hip are ideal subjects for the clinical section of final medical examinations, and it is only the most foolhardy student who will attend the examination without being able to examine the hip easily and confidently.
Radiology
Osteoarthritic hips show characteristic radiological changes (Fig. 24.1).
 |
| Fig. 24.1
Osteoarthritis of the hip showing joint space narrowing, cyst formation, subchondral sclerosis, osteophytes, thickening of the femoral head and bone destruction. Shenton’s line (dotted) shows collapse of the femoral head.
|
Radiological changes in osteoarthritis of the hip
1. Narrowing of the joint space.
2. Cyst formation in the femoral head and the acetabulum.
3. Sclerosis of subchondral bone.
4. Osteophyte formation.
5. Subcortical thickening on the medial side of the femoral neck.
6. If there is bone destruction as well, Shenton’s line will be disturbed, indicating true shortening of the limb.
Pathology
Osteoarthritis of the hip begins with fibrillation of the articular surface and the formation of wear particles. The wear particles are swept to the side of the joint where they irritate the synovium and are responsible for some of the patient’s pain and the formation of osteophytes.
As the disease progresses, articular cartilage is lost, subchondral bone is exposed and the bone surfaces become eburnated (Fig. 24.2). Grooves form in the joint surfaces and the hip is gradually converted from a ball and socket into a roller bearing. Later, cysts form in the bone and the femoral head may collapse.
 |
| Fig. 24.2
Osteoarthritic femoral head.
|
Untreated, the hip becomes fixed in flexion, adduction and external rotation, a position which interferes seriously with mobility.
Treatment
The conservative treatment of osteoarthritis of the hip includes the following:
Conservative treatment of osteoarthritis of the hip
1. Anti-inflammatory drugs.
2. Weight reduction.
3. A stick, which is only helpful if it is held in the opposite hand and used correctly.
4. A raise to the shoe of the shorter limb to correct the apparent shortening and relieve the abnormal strain on the lumbar spine and opposite hip.
5. Aids to daily living to help the patient put on shoes and stockings and pick up dropped articles.
All these measures are important and must be considered, even if not adopted, before operation is recommended. There is some evidence that an arthroscopic washout and debridement is useful in the early stages. The results of this in established osteoarthritis of the elderly are poor.
Rheumatoid arthritis of the hip
As elsewhere, rheumatoid arthritis destroys bone, but the osteophytes and sclerosis of osteoarthritis are usually absent. Instead, the femoral head is gradually eroded or collapses suddenly, resulting in true shortening of the leg (Fig. 24.3).
 |
| Fig. 24.3
Rheumatoid arthritis of the hip. Note the thinning of the medial wall.
|
Treatment
If conservative measures fail, joint replacement is the only effective treatment. Rheumatoid patients do well because their activity is limited by disease elsewhere and also because they are generally lightweight.
Total hip replacement
Total hip replacement is the most popular operation for osteoarthritis of the hip and consists of replacing both surfaces of the joint with artificial materials (Fig. 24.4). The acetabulum is reamed out to take a cup and the femoral head replaced with a metal ball attached to a stem inserted in the femoral shaft. A resurfacing component that does not use a long stem has recently been introduced and is often used in younger patients to prevent bone loss (Fig. 24.5).
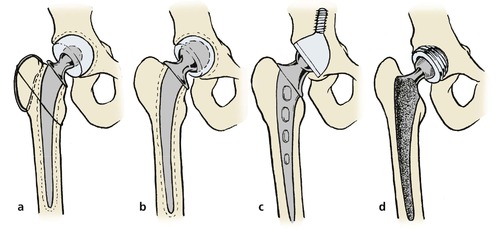 |
| Fig. 24.4
Types of total hip replacement: (a) Charnley hip replacement with greater trochanter reattachment; (b) Müller type replacement with larger femoral head; (c) ring-type replacement using a long, threaded acetabular component without cement; (d) uncemented prosthesis with sintered surfaces and screw-in acetabular prosthesis.
|
 |
| Fig. 24.5
Hip resurfacing components.
|
There are many types of hip replacement but most have a femoral component made of either stainless steel or a chrome cobalt molybdenum alloy and a cup made of high density polyethylene. Both components are usually fixed to the skeleton with cold curing acrylic cement (p. 49 and p. 299). Metal on metal articulation is possible and reduces the amount of wear debris within the hip capsule, as do ceramic bearings.
Some prostheses are inserted without cement, fixation relying on bone growing into irregularities on the surface of the component. The size and shape of the pores into which bone can grow is critical in securing fixation. A covering of hydroxyapatite may enhance this ingrowth; ceramic components are also used and new designs are continually being introduced.
Of the many different types of hip replacement, the Charnley low friction arthroplasty, the Exeter and the Stanmore are the best known (Fig. 24.6 and Fig. 24.7).
 |
| Fig. 24.6
A Charnley hip prosthesis.
|
 |
| Fig. 24.7
A Charnley total hip replacement.
|
The friction in most total hip prostheses is about 40 times greater than that of a normal healthy hip and this imposes a strain on the fixation of the components to bone. Furthermore, the rigid femoral stem causes stress risers in the femoral shaft.
Types of total hip prosthesis
• Cemented. In this, the most commonly used type, the components are fixed to bone with an acrylic cement. The acrylic cement can cause bone destruction if the components become loose, e.g. Charnley. Designed by Sir John Charnley, this prosthesis has been used since the late 1960s. It is made of stainless steel, has a small femoral head, a high density polyethylene cup and is secured with acrylic cement.
• Hybrid. In this, only one of the components is fixed by cement.
• Isoelastic. The femoral stem is designed to have the same flexibility as bone in order to minimize stress risers within the femoral shaft. These have not been shown to offer any great advantage.
• Ceramic. The bearing surfaces are made of aluminium oxide. Mechanical characteristics are good but the components can crack and ceramic particles may be irritant.
• Resurfacing. Use of a metal on metal articulation without a long femoral stem (Fig. 24.8).
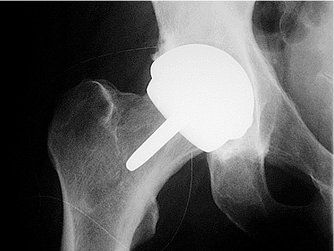 |
| Fig. 24.8
A metal on metal hip resurfacing component.
|
Results
The results of total hip replacement are spectacular, with good or excellent results in approximately 98% of patients. The operation is most successful in relieving pain but some restoration of movement and an improved gait can also be expected.
The results are so good that the operation has revolutionized hip surgery and brought treatment to many who would otherwise have been untreatable. This has in turn brought great pressure on the resources available for orthopaedic surgery.
Indications
The ideal patient for total hip replacement is a lightweight elderly patient who has severe pain and places few demands on the hip. The most unsuitable is a young, heavy, active man who wants to play football and return to heavy work. Between these two extremes the degree of pain and disability is weighed against the patient’s age and physical requirements but, in general, total hip replacement should not be offered to the following types of patient:
1. Those under the age of 60.
2. Those who are obese.
Technique
The operation can be done in several ways and through several approaches. These include:
1. The anterolateral approach, between tensor fasciae latae and the glutei.
2. The posterior approach through the posterior capsule.
3. The Charnley approach with detachment of the greater trochanter.
4. Detachment of the glutei and a portion of the vastus lateralis muscle.
With all these approaches the principle is the same. The acetabular surface is prepared by removing all debris and soft tissue and the femoral head is removed. The acetabulum is then replaced with a prosthetic component, which is fixed either mechanically or with bone cement. The femoral component is then inserted and similarly secured.
Prevention of infection
Infection in a prosthetic hip is a disaster and great care must be taken to prevent it occurring during operation by the following measures:
1. Meticulous asepsis during operation, or
2. Prophylactic antibiotics, or
3. A combination of the two.
Aseptic techniques. Meticulous asepsis in an operating enclosure with ultraclean air changed continuously and impervious operating gowns with individual exhaust systems for expired air (Fig. 24.9) can reduce the infection rate to 0.2%, but the operations may also be done in a standard operating theatre.
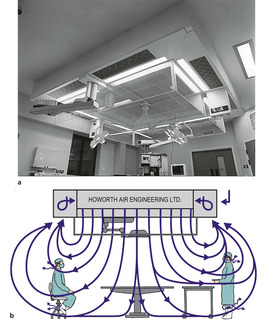 |
| Fig. 24.9
(a) Modern version of the world’s first clean air enclosure for surgery – the Charnley Howorth Exflow Ultra-Clean Air System. (b) The flow of air using an ultraclean system with exponential flow. By kind permission of Howorth Airtech.
|
Prophylactic antibiotics used in a standard operating theatre will produce a similar infection rate to the operating enclosure. A regimen of flucloxacillin 500 mg started with the premedication and continued for three doses is effective. If the patient is allergic to penicillin, vancomycin may be used.
Combining antibiotics with a clean air enclosure can reduce the infection rate still further.
Catheterization. Inserting catheters immediately after operation runs the risk of infection. If it cannot be avoided, catheterization should be done gently with complete sterility and covered with an appropriate antibacterial drug.
Cross-infection. Patients with clean joint replacements should not be nursed in the same ward as those with abscesses, colostomies or open infection.
Postoperative care
Some surgeons prefer to hold the hip in abduction by placing a wedge-shaped pillow between the patient’s thighs for 2 days. This is particularly helpful if a Charnley hip prosthesis with a small femoral head has been used.
The suction drains are usually removed after 2 days, when the patient may sit out of bed. They should not sit in a low chair because this flexes the hips beyond 90° and can, in some circumstances, cause the hip to dislocate. Most patients should mobilize the next day with a frame and be walking reasonably with elbow crutches, ready for discharge, after 4–5 days. By then the patients should be able to climb stairs and be able to cope with many activities of daily living.
Between 6 and 12 weeks after the operation most patients have little pain from their hip and an improved range of motion that allows them to resume normal activities. However, heavy work, especially lifting and jumping, should be avoided indefinitely in case it stresses the bone–cement interface.
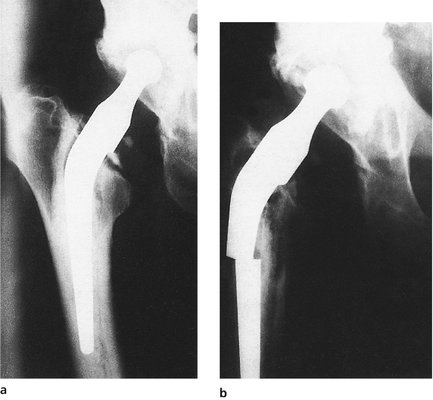
Failure
Not all hip replacements are successful and it is estimated that between 0.5% and 1% of all hip prostheses in position fail each year because of infection or loosening (Fig. 24.10).
 |
| Fig. 24.10
Early McKee–Farrar prosthesis with loosening and fracture of the pelvis.
|
Early infection around a total hip replacement almost invariably leads to failure and special care is needed to avoid infection at the time of operation.
Late infection can also occur later via the bloodstream from infections in the urinary tract or elsewhere.
The organisms responsible for infection around total hip replacements include many normally regarded as non-pathogenic, e.g. Staphylococcus epidermidis. The explanation is unknown but it may be that these bacteria flourish in the unusual tissue that surrounds prosthetic materials (glycocalyx), or that the minute amount of metallic salts leaving the prostheses inhibits macrophage activity.
Loosening. Acrylic cement is strong in compression but weak in shear and torque. It causes little soft tissue reaction as long as it is intact but in particulate form it initiates a foreign body reaction that destroys bone. These two factors put together mean that violent twisting stresses may split the cement and allow the two surfaces of acrylic to ‘fret’, creating wear particles which destroy bone, cause more loosening, more fractures in the cement, and failure of the bone–cement interface.
In many ways, a hip prosthesis can be compared with a fibreglass patch on an old car; the repair is perfect as long as the car remains in the garage but it will loosen if driven hard over a bumpy road. The analogy is apt because the cement used in hip surgery is similar to that used for car repairs.
From the clinical standpoint, loosening usually affects the femoral component in active and overweight patients and causes pain on weight-bearing and hip movement.
Pain in the thigh usually indicates loosening of the femoral component, pain in the groin loosening of the acetabular component. The patient does not feel the components moving within the bone until the loosening is very severe indeed.
Treatment of loosening. Replacement of the loose component with another may be successful, but the operation is more difficult and less reliable than a primary hip replacement. Excision arthroplasty may be needed (Fig. 24.11) as a salvage procedure.
 |
| Fig. 24.11
Porotic rheumatoid bone. The prosthetic components have been removed from the right hip and the bone has fractured around the cement on the left.
|
Other complications
Other complications include fracture of the components (Fig. 24.12), dislocation (Fig. 24.13) and excessive new bone formation (Fig. 24.14).
 |
| Fig. 24.12
Fracture of a femoral component. (a) Note the ‘windscreen wiper’ gap between the cement and prosthesis; (b) the component has fractured.
|
 |
| Fig. 24.13
Dislocation of a prosthesis. The cup was placed too steeply.
|
 |
| Fig. 24.14
New bone formation around a total hip prosthesis.
|
Investigation of a painful hip prosthesis
A painful hip prosthesis needs investigation by the following means:
• Radiographs.
• Blood tests.
• Isotope scans.
• Aspiration.
Radiographs. A transradiant line is seen around a loose or infected prosthesis, with scalloping of the deep surface of the cortex where it has been eroded by the foreign body reaction or infection.
Blood tests. Infection around hip prostheses is not dramatic and the white cell count is almost always normal. The ESR is usually raised to between 30 and 50 mm/h in both loosening and infection and does not differentiate between the two. The polymerase chain reaction to detect microscopic parts of the bacterial DNA may be the most sensitive.
Isotope scan. Technetium-99m scans show areas of activity in both loosening and infection and a gallium or indium scan may show areas of infection (Fig. 24.15).
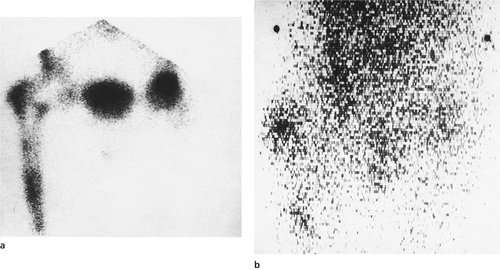 |
| Fig. 24.15
(a) Technetium-99m bone scan showing loosening or infection around the femoral components. (b) Gallium scan showing activity around the tip of the prosthesis and the greater trochanter, suggesting infection.
|
Aspiration. Aspiration of the fluid around the prosthesis is helpful if a bacterium is retrieved but a sterile aspirate does not exclude infection. This procedure should be done with full sterile precautions in the operating theatre.
Revision hip replacement
Replacing (revising) a hip replacement is more difficult than the original procedure. Technical problems include dissecting through tissue that has abnormal anatomy. Dense scar tissue may contain the femoral and sciatic nerves.
Removing the prosthesis and the bone cement is difficult. Bone cement is harder than bone and the femur may be split as the cement is removed from the depth of the shaft. There is likely to be such extensive bone loss in both the femur and acetabulum that the standard prostheses do not fit.
Care must be taken to be as certain as possible that the wound is not infected. Tissues can be examined by Gram staining during the procedure but a negative finding does not exclude infection. If it seems likely that infection is present, it is wise to remove all foreign material, irrigate thoroughly, pack the wound with antibiotic-impregnated beads and close it. Antibiotics should be given systemically for at least 8 weeks, by which time any residual infection should be under control. The new prosthesis can then be inserted at a second operation.
For all these reasons, revision surgery of the hip and other joints is a formidable procedure in terms of technique, surgical time and expense.
Other operations for osteoarthritis
Osteotomy
Before total hip replacement was available, femoral osteotomy was commonly done to realign the femur so that the load was taken by a different area of bone (Fig. 24.16). In this respect, the operation was similar in principle to moving an area of worn carpet away from the door. Osteotomy also affects the venous drainage of bone, and perhaps allows microfractures to heal.
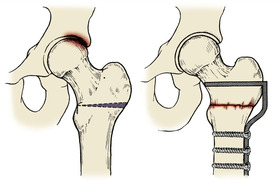 |
| Fig. 24.16
Osteotomy for osteoarthritis of the hip. A wedge is taken from the femur to alter load bearing across the hip.
|
Results of osteotomy are satisfactory in about 75% of patients 2 years after operation, but many have pain relief for much longer. The operation is indicated for younger patients who are unsuitable for total hip replacement. Acetabular rotational osteotomies work in the same way.
Excision arthroplasty
Excision arthroplasty was developed by Girdlestone as a primary procedure for osteoarthritis and is still known as Girdlestone’s operation. The hip joint is replaced with a fibrous ankylosis and is similar to Keller’s operation and other excision arthroplasties.
The operation converts a painful but stable joint into one that is unstable but less painful. The limb is shortened but function of the limb is improved. Today, the operation is done as a salvage procedure for failed total hip replacement and not as a primary procedure.
Arthrodesis
Arthrodesis of the hip leaves a solid hip that will last a lifetime and is indicated for gross destruction of the hip in a young patient, e.g. after a motorcycle accident (Fig. 24.17). The alternative operation in such a patient is a total hip replacement, which is doomed to failure in a young and active adult.
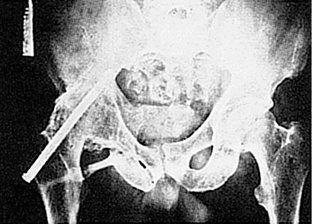 |
| Fig. 24.17
An extra-articular arthrodesis of the hip.
|
The operation has the advantage that an arthrodesis can be revised to a total hip replacement but hip replacement can only be revised to another hip replacement or excision arthroplasty.
Arthrodesis also has the disadvantage that the movement lost at the hip is made up for by excessive movement of the lumbar spine and the knee, which then become worn and present problems of their own.
Hemiarthroplasty
Prosthetic replacement of the femoral head alone was once used as a treatment for osteoarthritis of the hip but was unsuccessful because the degenerate acetabulum was eroded by the metal head of the prosthesis. The operation is successful when used as the treatment for fractures of the femoral neck because the acetabulum is healthy in these patients.
Interposition arthroplasty
Cup, or mould, arthroplasty was a standard operation for osteoarthritis of the hip before total hip replacement was introduced, but has now been superseded.
Surface replacement arthroplasty, in which both joint surfaces were replaced but the femoral shaft left intact, was comparable with a mould arthroplasty. The operation was introduced in the 1980s but the results were poor and it became obsolete. New designs of such prostheses are promising (see Fig. 24.5 and Fig. 24.8).
Other hip conditions
Protrusio acetabuli
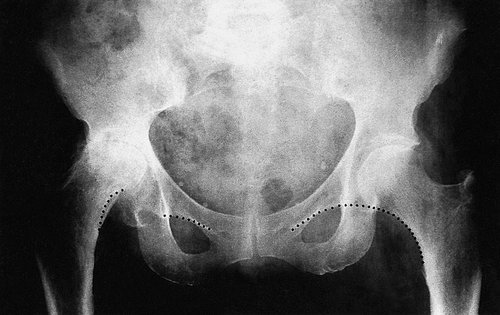
Protrusio acetabuli is a strange condition for which no cause is known (Fig. 24.18). The medial wall of the acetabulum becomes paper-thin and the head migrates medially. The result is a hip that is virtually ankylosed in the neutral position.
 |
| Fig. 24.18
Bilateral protrusio acetabuli.
|
Treatment. Untreated, the patient loses both rotation and abduction and in effect has bilateral hip arthrodesis. No treatment is effective except joint replacement.
Ankylosing spondylitis
Ankylosing spondylitis causes stiffness of the spine and large weight-bearing joints, including the hip. The HLAb27 gene is often found in association with this condition.
Treatment. It is tempting to restore joint movement by total hip replacement but the hips may stiffen again with a bony ankylosis around the components. Apart from general conservative management to improve the function of the joint, there is no effective treatment for ankylosing spondylitis of the hip.
Infections
Tuberculosis of the hip was a common cause of hip disease in the past and many older patients still have destroyed or ankylosed hips as a result. Total hip replacement produces a good result. The theoretical risk that the mycobacteria could be lying dormant at the hip and be reactivated at the time of operation does not appear to be justified in practice.
Trochanteric bursitis
The trochanteric bursa lies between the greater trochanter and the insertion of the abductors and, like other bursae, can become inflamed and swollen. Some patients have an acute calcific bursitis comparable with acute calcific supraspinatus tendinitis.
On clinical examination the pain is localized to the greater trochanter and the bursa is tender. Passive hip movements are full but active abduction and abduction against resistance are painful. Radiographs may show a puff of calcification arising from the apex of the greater trochanter.
Treatment. A steroid injection into the bursa usually produces immediate relief of symptoms.
Septic arthritis
Acute septic arthritis is a rare condition today and therefore often escapes diagnosis when it does occur.
Treatment. Left untreated for even 24 h, the articular cartilage of the hip is destroyed and late osteoarthritis becomes almost inevitable. Accordingly, any child with an acute illness and a painful hip should be considered to have septic arthritis until proved otherwise.
The treatment consists of intravenous antibiotics after blood culture specimens have been sent to the laboratory, and immediate exploration of the hip.
Septic arthritis in adults is rare, but gonococcal arthritis is sometimes seen. In debilitated patients, diabetics and those taking steroids, septic arthritis is not uncommon.
Irritable hip (transient synovitis)
This condition is of unknown aetiology. It may occur 2–3 weeks after a viral upper respiratory tract infection. It is important to exclude sepsis of the hip and, in approximately 4% of cases, Perthes’ disease. The condition usually settles spontaneously over 2–3 days.
Treatment. No treatment is required apart from reassurance and analgesics but the condition is important because its presentation is similar to that of acute septic arthritis. It is therefore prudent to admit children with irritable hips to hospital if there is any suspicion of systemic illness or pyrexia, so that systemic antibiotics can be administered without delay. Ultrasound scans of the hip and aspiration of the joint are used to differentiate the two conditions and can be used on an outpatient basis.
Snapping hip
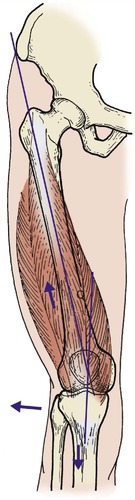
Odd thuds and bangs can arise from normal hips and cause much anxiety, although they are seldom of serious significance. The commonest type is due to the iliotibial tract snapping across the greater trochanter when the patient stands on the affected leg while flexing and extending the knee (Fig. 24.19).
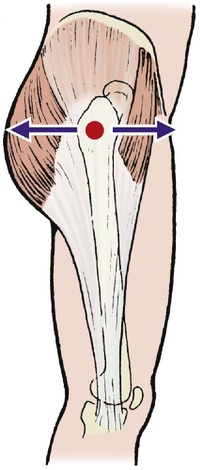 |
| Fig. 24.19
Snapping hip caused by the iliotibial band flicking across the greater trochanter.
|
Treatment. Apart from reassuring the patient that they are not dislocating the hip – a frequent anxiety – no treatment is required for these hips.
Osteoarthritis of the knee
Clinical features
Osteoarthritis of the knee can follow trauma, infection, meniscectomy, ligament injury or any other insult to the joint, but it also occurs without any obvious cause.
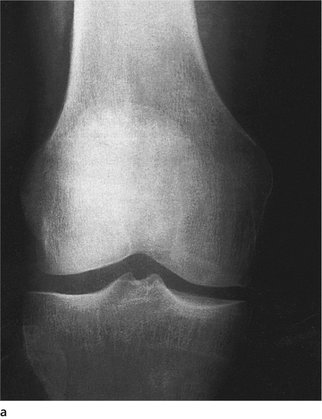
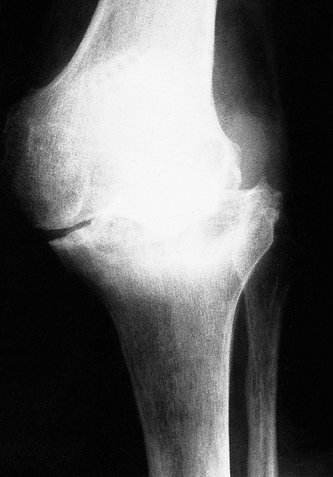
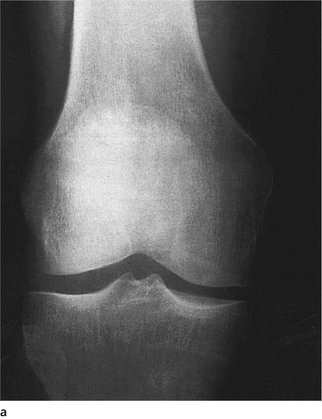
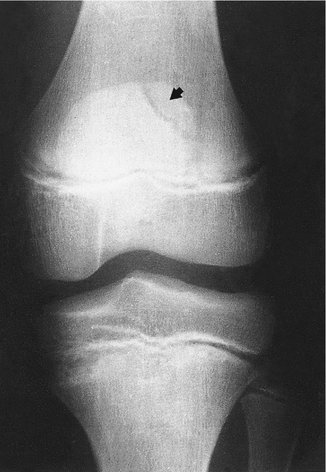
The medial compartment is more often affected than the lateral and a varus deformity develops as the medial compartment becomes worn (Fig. 24.20 and Fig. 24.21). As the varus increases, more load is taken by the medial compartment, the wear becomes greater, the deformity worse and the disease progresses rapidly (Fig. 24.22). On examination, a valgus strain will open up the medial side as the tibia returns to its normal position. This is due to wear of the medial compartment, not to the medial ligament being lax.
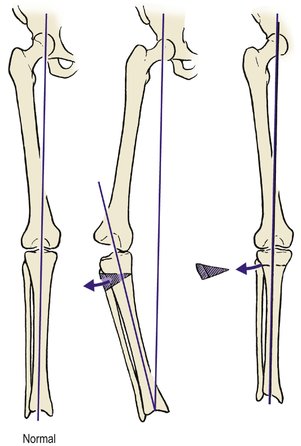 |
| Fig. 24.20
Corrective osteotomy for osteoarthritis of the knee. The aim of the procedure is to place the hip, knee and ankle in correct alignment.
|
 |
| Fig. 24.21
The upper surface of the tibia removed at total knee replacement. The medial plateau has exposed bone and grooves, and is surrounded by osteophytes. The lateral plateau is almost normal. Note that it is convex upwards, not concave.
|
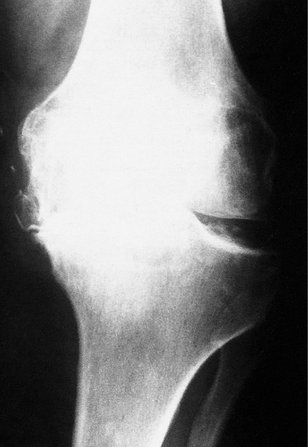 |
| Fig. 24.22
Medial compartment osteoarthritis. Note the narrowing of the medial compartment, widening of the lateral compartment and a varus deformity.
|
As the condition progresses, osteophytes form around the joint, cysts develop in the femur and tibia, and crepitus is felt when the knee is moved.
Treatment
Conservative treatment should always be tried before suggesting operation.
Many patients with early osteoarthritis experience a little aching after long walks and require only anti-inflammatory drugs. Some find that it is helpful to take the tablets before the anticipated exercise, e.g. before the weekend golf match or long shopping expeditions.
In more advanced disease the usual conservative measures of a stick, weight reduction, restriction of activity, analgesics and anti-inflammatory drugs are all helpful. Only when these measures fail should operation be considered.
Tibial osteotomy
Tibial osteotomy can correct the varus deformity of medial compartment osteoarthritis and break the vicious circle which leads to progressive wear and collapse by adjusting the line of weight-bearing so that the healthy compartment takes more weight (Fig. 24.23). The operation is most useful in patients with a worn medial compartment and a healthy lateral compartment.
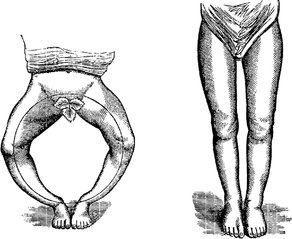 |
| Fig. 24.23
Corrective osteotomy.
From: MacEwen, William (1880) Osteotomy, J & A Churchill, London. By kind permission of the Wellcome Institute Library, London.
|
Disadvantages are that the operation is a major inconvenience to the patient and is not always effective. The osteotomy takes 6–8 weeks to unite and the underlying osteoarthritis remains. Nevertheless, about 75% of patients are content with the knee 2 years later and the operation conserves bone stock so that a knee replacement can be performed later if it becomes necessary. Later conversion to a total knee replacement is often difficult.
Low femoral osteotomy
For patients with a valgus deformity greater than 10° a low femoral osteotomy is preferable to a high tibial osteotomy.
When the lateral compartment is worn, there is usually more bone loss from the femoral condyle than the tibial plateau and correcting the deformity by tibial osteotomy leaves a knee joint that is no longer parallel with the ground. This can lead to further problems. The operation is done by removing a wedge of bone based medially from the lower part of the femur and securing the fragments with a blade plate (Fig. 24.24). Early mobilization and weight-bearing is possible but the plate should be removed approximately 1 year after operation.
 |
| Fig. 24.24
A low femoral osteotomy for a valgus deformity internally fixed with blade plate and screws.
|
Total knee replacement
Total knee replacement is a greater technical challenge than total hip replacement. Whereas the hip can move in any direction and rotate about its axis, the knee has a maximum of 150° flexion in one plane only.
This has a number of implications. The fixation is subjected to far more stress than the hip, making loosening more likely, and the prostheses are designed to minimize the forces on the interface between the patient and the prosthesis.
Placement of the prosthesis must be more accurate than in the hip and even 3° of malalignment can lead to failure. To add to these difficulties, the prostheses are larger and more superficial than a hip prosthesis.
Treatment of a failed total knee replacement is also less straightforward (Fig. 24.25). A failed hip replacement can be salvaged by converting it to an excision arthroplasty but excision of the knee produces a very poor result indeed and the joint must be arthrodesed.
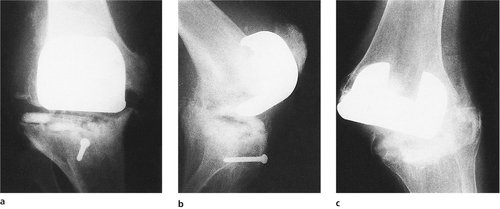 |
| Fig. 24.25
Failed total knee replacement. (a), (b) The bone has collapsed beneath the tibial plateau and the femoral component has come completely away from the femur. (c) The medial side of the joint has become disrupted and the prosthesis has dislocated. The operation was done beneath a stiff hip.
|
The potential for making the patient worse rather than better is therefore considerable.
Results. The criteria for a good result from knee replacement are less ambitious than for total hip replacement. A successful knee replacement offers the following:
1. A knee that will straighten.
2. Flexion to 100° so that the patient can rise from a chair.
3. A leg that will take the patient’s weight while standing.
4. A stable joint.
Five years after operation, the result is still as good as this in approximately 90% of patients.
Total knee prostheses can be considered in four groups and may either be secured with acrylic cement or left uncemented (Fig. 24.26):
1. Unconstrained prostheses.
2. Semiconstrained surface replacements.
3. Mobile bearing prostheses.
4. Fully constrained (hinges).
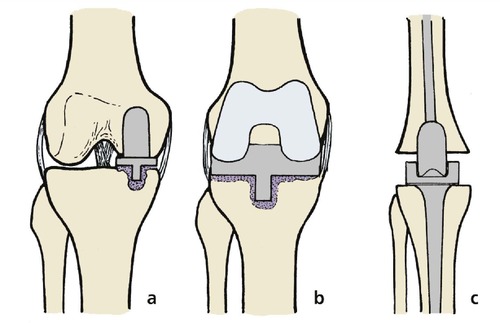 |
| Fig. 24.26
Types of total knee replacement: (a) unicompartmental arthroplasty; (b) unconstrained total knee replacement; (c) constrained hinge total knee replacement.
|
They can also be considered as unicompartmental or total replacement prostheses. Unicompartmental prostheses replace the medial or lateral compartment when the other is healthy. Total knee replacements replace both the medial and lateral compartments and usually the patellofemoral joint as well.
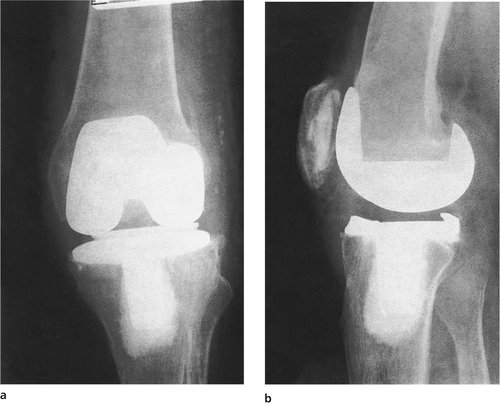
Unconstrained prostheses consist of metal and plastic components secured separately to the femoral and tibial surfaces of each compartment. The components simply resurface the joint and do not contribute any stability to the joint. They should only be used when the joint is stable and the ligaments intact. They are suitable for early disease or disease of one compartment only and may be revised to another surface replacement (Fig. 24.27).
 |
| Fig. 24.27
(a) Osteoarthritis of the knee with valgus deformity; (b) corrected by a unicompartmental arthroplasty; (c) anteroposterior and (d) lateral view of a different type of prosthesis inserted for a varus deformity.
|
Semiconstrained prostheses replace the whole of both joint surfaces and the patella and contribute to the stability of the joint by their shape. This means that the fixation to the skeleton is exposed to greater forces (Fig. 24.28). The amount of stability they offer varies from one design to another.
 |
| Fig. 24.28
(a), (b) An Insall–Burstein total knee replacement.
|
Semiconstrained prostheses are more suitable than unconstrained prostheses for more advanced disease.
Mobile bearing prostheses allow the plastic insert to move on the flat tibial tray, thereby hopefully reducing the wear.
Fully constrained prostheses (hinges). Hinged knees are constrained; i.e. the two parts are firmly linked mechanically. For a grossly unstable joint with poor bone stock, a hinge offers a sound and stable limb (Fig. 24.29). The disadvantages are that extensive bone resection is required, making revision difficult (Fig. 24.30). If the prosthesis is removed for loosening or infection, two hollow trumpets of bone remain, arthrodesis is almost impossible and amputation is sometimes the only solution.
 |
| Fig. 24.29
(a), (b) A Stanmore hinge total knee replacement.
|
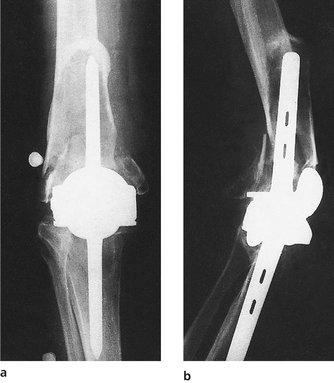 |
| Fig. 24.30
(a), (b) A failed Walldius total knee replacement. The femur has fractured and both femoral and tibial components have worked through the bone.
|
Revision knee replacement
Revision replacement of a prosthesis is more difficult at the knee than the hip for three reasons:
1. Soft tissue tension must be restored to eliminate varus and valgus instability.
2. Loosening and infection both cause bone loss. This means that the new prosthesis must be larger than the old.
3. The extensor mechanism must remain intact.
Revision often involves the use of a ‘custom-made’ prosthesis for the individual patient. These are sometimes supplied in modular form and assembled during operation.
If the knee is to be revised for infection, the original prosthesis and cement must be removed and infection eradicated. This may involve replacing the prosthesis with a mass of antibiotic-impregnated acrylic cement for between 6 and 12 weeks, during which time the knee will be unstable and the patient may be unable to walk. The new prosthesis can be inserted when the infection has been eliminated but antibiotics should be given for several weeks or months after operation. Even then, the infection may recur.
Amputation must sometimes be considered if the knee cannot be salvaged.
Arthrodesis
Arthrodesis of the knee, like other arthrodeses, is a reliable operation that lasts a lifetime. The operation allows the patient to walk comfortably but makes it impossible to sit comfortably and difficult to climb out of a car or bath. The operation is indicated in badly damaged knees in young adults.
Arthrodesis is achieved by compressing the two bone surfaces together, usually by external fixation devices, or a plate, or with an intramedullary nail (Fig. 24.31).
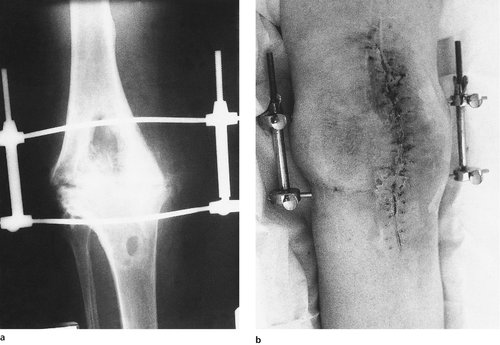 |
| Fig. 24.31
(a), (b) Arthrodesis of the knee using Charnley compression clamps. The operation was done for infection following total knee replacement.
|
Debridement and lavage
Arthroscopic joint debridement to remove loose tags of meniscus, osteophytes and articular cartilage debris while leaving the meniscal rim intact produces a satisfactory result in about 75% of patients with early osteoarthritis. Arthroscopy also allows a thorough inspection of the joint surfaces so that a firm prognosis can be offered but it does not make the osteoarthritis regress.
Debridement is not an alternative to osteotomy or joint replacement.
Management of osteoarthritis of the knee
The following is a very rough guide to the management of osteoarthritis of the knee:
1. Recurrent effusions, little or no deformity and near normal radiographs with or without mechanical symptoms – conservative treatment with NSAIDs, weight reduction, physiotherapy.
2. As above, if conservative treatment has failed – arthroscopic debridement.
3. Increasing deformity and disability in patients under the age of 60 – osteotomy.
4. Increasing deformity with disease confined to only one compartment, over the age of 60 – unicompartmental joint replacement.
5. Deformity and disease involving two or more compartments, over the age of 60 – total joint replacement with unconstrained prosthesis.
6. Gross instability and collapse, over the age of 70 – total joint replacement with constrained prosthesis if necessary.
Rheumatoid arthritis of the knee
The treatment of acute rheumatoid arthritis is conservative but synovectomy may be needed if the synovial disease cannot be controlled medically (Fig. 24.32).
 |
| Fig. 24.32
Rheumatoid arthritis with destruction of the tibial plateau and a valgus deformity.
|
In patients over the age of 60, synovectomy can be done chemically or with a radioisotope such as yttrium. The indications for surgical synovectomy are becoming much less common as medical management improves, but it is still required for young patients with uncontrolled disease.
Synovectomy is now usually performed arthroscopically to minimize surgical trauma.
Treatment
As the disease progresses, bone is destroyed, deformities develop and salvage procedures become necessary. Osteotomy is not helpful and joint replacement is usually required.
Septic arthritis of the knee
Septic arthritis of the knee has several causes (p. 314):
1. Penetrating injuries.
2. Spread from osteomyelitis of the lower end of the femur or upper end of the tibia.
3. Systemic infection, e.g. septicaemia or gonococcal infections.
Treatment
Septic arthritis of the knee is managed in the same way as in other joints, with rest, adequate antibiotics and irrigation. Suction drainage is particularly suitable for septic arthritis at the knee, and thorough lavage combined with arthroscopy is effective.
Internal derangements of the knee
The term ‘internal derangement of the knee’ is a common provisional diagnosis for any patient with mechanical symptoms in the knee. The initials ‘IDK’ also stand for ‘I don’t know’ and the temptation to use these initials instead of making a complete diagnosis must be avoided.
There are many causes of internal derangements of the knee.
Common internal derangements of the knee
• Meniscus lesions
• Loose bodies
• Chondral separations
• Osteochondritis dissecans.
Meniscus lesions
Meniscus lesions are the commonest internal derangements. Although the menisci are damaged by trauma, they are included in this section because the trauma responsible is often so trivial that the patient cannot remember any injury at all. Because of this, patients with meniscal injuries are most often seen in orthopaedic clinics and not accident departments.
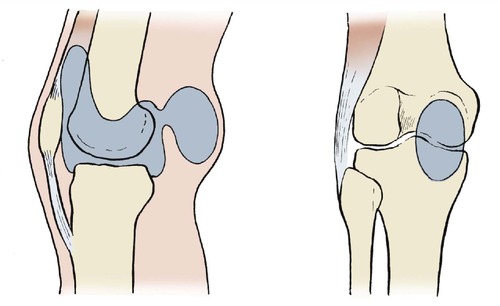
Function of the meniscus
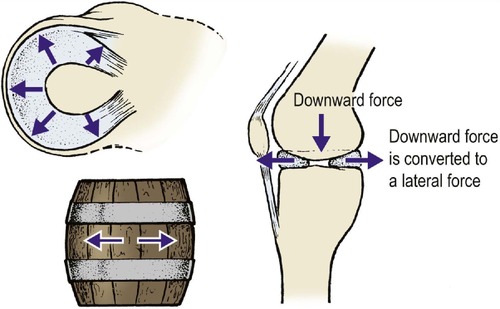
The menisci are important parts of the load-bearing mechanism of the knee and they absorb the downward thrust of the convex femoral condyles (Fig. 24.33). The menisci are so effective that, if they are removed, the force taken by the articular cartilage on peak loading increases by about five times. Meniscectomy therefore exposes the articular cartilage to much greater forces than normal, and evidence of degenerative osteoarthritis is seen in 75% of patients 10 years after total meniscectomy.
 |
| Fig. 24.33
Function of the menisci. The menisci act like hoops on a barrel.
|
If degenerative osteoarthritis is already present at the time of meniscectomy, the degeneration will progress much more rapidly, and it is therefore important to conserve as much meniscal tissue as possible in degenerative joints.
The menisci are constructed a little like ligaments but they are curved and their ground substance is stiffer. When a meniscus tears, a mobile gristly fragment is produced inside the knee which pops in and out of the joint and blocks movement.
The characteristic symptoms of a meniscal lesion are caused by movement of the meniscal fragment in the joint and include recurrent locking and unlocking of the knee; i.e. mechanical obstruction of movement followed by a return to normal. The original tear and the subsequent locking usually occur with little applied violence and are often the result of twisting on the bent knee, or even from turning over in bed.
Patients use ‘locking’ to describe episodes of severe pain, or even collapsing of the knee. It is curious that the word is not applied in this way to other joints. ‘Locking’ means mechanical ‘jamming’ of the joint, and nothing more.
Meniscal tears
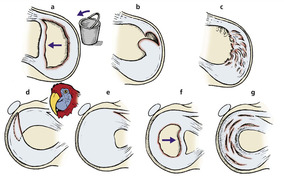
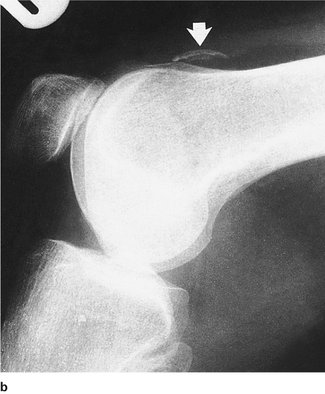
Several types of meniscal tear are seen (Fig. 24.34). A circumferential tear creates a long fragment attached at each end which can swing over into the intercondylar notch. The movement of the fragment is likened to a bucket handle and these fragments are known as bucket handle fragments (Fig. 24.35).
 |
| Fig. 24.34
Types of meniscal lesion: (a) bucket-handle tear; (b) flap tear; (c) degenerate tear of the medial meniscus; (d) oblique ‘parrot-beak’ tear of the lateral meniscus; (e) discoid lateral meniscus; (f) locked bucket-handle tear of the lateral meniscus; (g) cystic or myxoid degeneration of the lateral meniscus.
|
 |
| Fig. 24.35
A bucket-handle fragment of the medial meniscus.
|
Flaps and pedunculated fragments do not cause mechanical locking but they move in and out of the joint space and can sometimes be felt in the medial or lateral gutter of the knee.
On the lateral side, complex oblique tears based on the popliteus tunnel occur and are called ‘parrot beak’ tears because of their shape. These tears result from a sharp twisting injury when the lateral compartment is loaded. They do not occur in the medial compartment because it does not have a popliteus tunnel.
Discoid menisci
In approximately 5% of people the lateral meniscus is congenitally abnormal, lacking its normal crescentic shape. The meniscus in these patients may be truly circular, or discoid, but is more often shaped like a half-moon. The meniscus may also be thicker than normal.
Intact discoid menisci seldom cause symptoms, but in children they may be responsible for a block to extension or a loud clunk when the knee is straightened. Discoid menisci may become torn and cause mechanical symptoms like other meniscal tears, or undergo ‘cystic’ change which causes a dull aching pain in the knee.
‘Cystic’ menisci
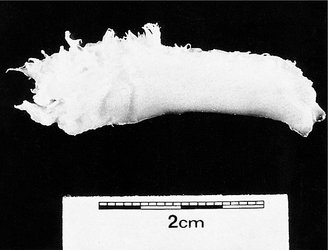
Meniscal tissue can undergo a myxoid degeneration, which converts the normal firm meniscal tissue to a soft and friable mass (Fig. 24.36). The lateral meniscus is affected far more often than the medial.
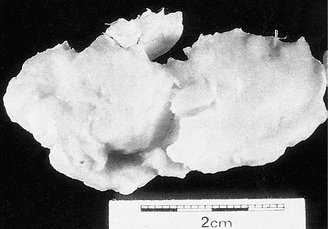 |
| Fig. 24.36
A lateral meniscus affected by cystic (myxoid) degeneration.
|
The classic symptoms of a cystic meniscus are a dull, aching pain in the lateral side of the knee ‘like toothache in the knee’, often worse at night. No conservative treatment is effective.
Meniscal cysts
Degeneration of the menisci must be distinguished from ganglia on the lateral joint line. Ganglia can develop anywhere and need only to be excised without opening the joint.
A true cyst in a degenerate meniscus may communicate with the knee by a horizontal fissure, sometimes called a ‘fish mouth’ tear.
Treatment
Because of the importance of the meniscus in load-bearing it is essential that the meniscus is left undisturbed until the diagnosis has been confirmed by arthroscopy or MRI. Clinical diagnosis alone is accurate in only 70% of patients.
Tears. When the diagnosis is confirmed, the loose fragment should be excised, leaving as much healthy meniscal tissue as possible. The operation is almost always undertaken arthroscopically because this allows a precise diagnosis and careful excision of the lesion with preservation of all intact tissue (Fig. 24.37). Patients can return to light work 1 week after arthroscopic meniscectomy, and heavy work within 2 weeks.
 |
| Fig. 24.37
Withdrawing a fragment of medial meniscus from the knee by arthroscopic surgery.
|
Open meniscectomy gives equally good long-term results but the initial rehabilitation is slower and patients may be unable to return to work for as long as 3 months. The only indication for open meniscectomy is the inability of the surgeon to perform arthroscopic meniscectomy.
Reattachment is suitable for peripheral tears that leave the meniscus intact but mobile. Such tears are most often seen in patients with anterior cruciate ligament ruptures.
Discoid menisci. Conservative surgery is important in the management of discoid menisci, which are commonly seen in children, because total lateral meniscectomy in a child leads to early osteoarthritis. Symptomatic discoid menisci should be treated by excision of any torn fragments.
Loose bodies
Loose bodies (Fig. 24.38) which float around the knee and obstruct movement can arise from osteochondritis dissecans, synovial chondromatosis, osteochondral fractures or localized separation of the articular cartilage. They can also grow in the synovial fluid, which is an excellent tissue culture medium. Patients with loose bodies give a classic account of a loose fragment in the knee and will usually be able to describe its size and shape. Loose bodies are sometimes called joint mice – a good analogy because they can be recognized instantly but disappear and may then be impossible to find again.
 |
| Fig. 24.38
Multiple loose bodies removed from the knee.
|
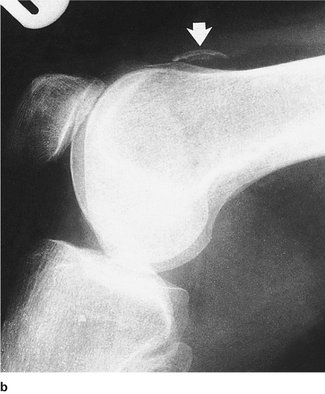
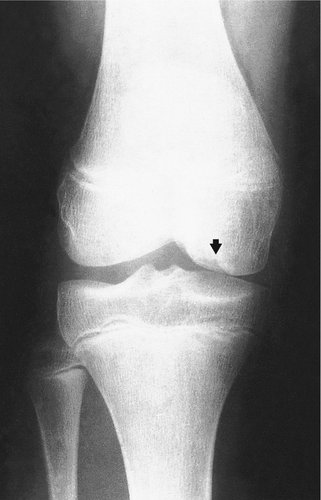
Radiographs are less helpful than might be imagined and at least two views in different planes are essential (Fig. 24.39). Twenty five percent of loose bodies are transradiant, and not all isolated areas of calcification in the knee are due to loose bodies. Some are firmly fixed to synovium and the fabella can be confused with a loose body by the unwary.
 |
|
(a) Osteochondritis dissecans of the knee. Can you see the crater or the fragment? (See Fig. 24.39 (b) for the answer.)
|
 |
|
(b) The loose body ( arrowed) is lying in the suprapatellar pouch.
|
| Fig. 24.39 |
Loose bodies should not be called ‘foreign bodies’. Foreign bodies, including bullets and bits of gravel, come from outside the body and are rare in joints.
Treatment
Removing the loose fragment is the only reliable way to relieve symptoms.
Osteochondral lesions
Many different pathological processes can affect the femoral condyles. The conditions themselves are separate, are treated differently and have different prognoses. They are not all different types of osteochondritis dissecans, however beguiling such an impressive Latin diagnosis may be.
There are five main types of osteochondral lesion:
1. Osteochondral fractures.
2. Chondral flaps and separations.
3. Osteochondritis dissecans.
4. Spontaneous osteonecrosis.
5. Osteochondritis dissecans of the lateral condyle.
Osteochondral fractures
In adolescents and young adults, twisting movements of the knee or a direct blow can detach a segment of bone and articular cartilage (Fig. 24.40). Patients can usually remember the moment of detachment and the incident is usually accompanied by a haemarthrosis.
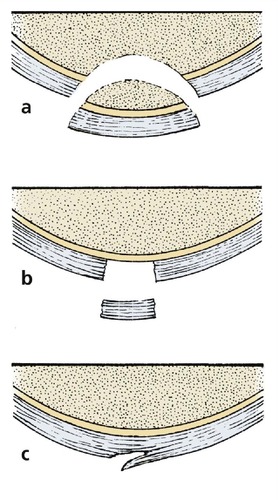 |
| Fig. 24.40
(a) Osteochondral fracture of the articular surface involving articular cartilage and bone; (b) full thickness chondral separation of articular cartilage without involving bone; (c) partial thickness flap of articular cartilage.
|
Treatment
Fragments can be reattached if they are large enough to take a screw. Many osteochondral fragments pass undiagnosed and wander freely around the joint as a loose body. The bed of the defect eventually heals with fibrocartilage and the fragment rounds off.
Chondral separations and flaps
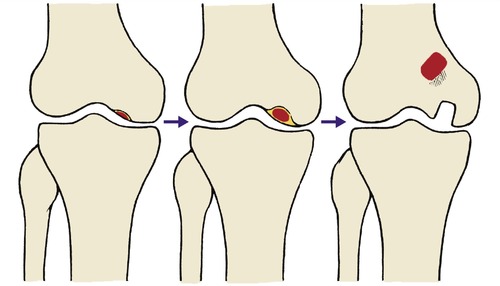
Osteochondral fractures are rare after the age of 30 but fragments of articular cartilage can separate from the underlying bone (Fig. 24.41). Radiographs do not show these fragments because articular cartilage is transradiant, but they can be found arthroscopically.
 |
| Fig. 24.41
Progression of osteochondritis dissecans from a small lesion on the medial femoral condyle to loose body formation.
|
Partial thickness separations, or chondral flaps, also occur and can mimic the symptoms of a meniscal tear. These occur in a slightly older age group.
Osteochondral fractures most commonly occur between 10 and 25 years, separations between 25 and 40, and flaps over the age of 40.
Treatment
Some chondral flaps are ground away by the action of the joint and the symptoms then disappear.
Chondral separations do not heal perfectly, however they are treated. Removal of the flap may help but this leaves a large area of bone exposed. An autologous chondrocyte transplantation may help cover this defect, as may a mosaicplasty. This involves moving a core of chondral surface and bone from one part of the knee to the defect.
Osteochondritis dissecans
Osteochondritis dissecans (not desiccans – the fragment does not dry up but dissects out) involves the medial femoral condyle and presents with pain between the ages of 8 and 12 years (Fig. 24.42). Boys are more often involved than girls, in a ratio of 6 : 1. The pain is worse when walking and on hyperextension.
 |
| Fig. 24.42
Osteochondritis dissecans before skeletal maturity.
|
On clinical examination there may be tenderness just medial to the patellar ligament and pain on hyperextension. The pain is sometimes more marked with the foot in internal rotation than external rotation.
Radiographs in the very early stages show only a small irregularity of the medial condyle. As growth proceeds, the irregularity develops into an area of bone separated from the rest of the condyle by a transradiant line. There may be several ‘fragments’ lying in the crater on the condyle. The articular surface overlying the lesion is intact at first, but after skeletal maturity the fragments may become loose and separate as a loose body within the knee.
Treatment
Conservative. Many fragments unite spontaneously without treatment and there is no evidence that the application of a cast increases the chances of natural union. Operation should not be considered unless the patient has been observed for at least 6 months, continues to have pain, and has no sign of radiological union.
Operative treatment. The lesion can be made to unite in approximately 90% of cases by drilling holes through the articular surface overlying the lesion into the medial femoral condyle. This can be done under arthroscopic control.
If the articular surface is broken and the fragment is loose it may be secured with a small screw or several pins. There are many techniques for performing this procedure.
Once the fragment has separated as a loose body a permanent defect remains on the articular surface. The fragment must be removed as a loose body and attempts to replace it are usually unsuccessful.
Spontaneous osteonecrosis
The cancellous bone in the weight-bearing area of the medial femoral condyle may undergo necrosis in patients over the age of 50. No cause is known. The cancellous bone is involved but the articular cartilage and cortex remain intact until they collapse into the defect. The condition is accompanied by pain and an increasing varus deformity.
Treatment
The lesion can be debrided arthroscopically and this produces a temporary benefit. Osteotomy may be helpful in transferring weight to the healthy lateral compartment but joint replacement is usually required in the long term.
Osteochondritis of the lateral femoral condyle
Large segments of the weight-bearing area of the lateral femoral condyle may separate from the rest of the condyle in early adult life. The condition differs from ‘classic’ osteochondritis dissecans, described above, in the age of the patients affected, the shape of the lesion, and the outcome. The cause is not known but the outcome is poor.
Treatment
The loose fragments require excision because the bone is too soft to be replaced.
Other knee disorders
Popliteal cysts
The synovial cavity of the knee often extends into the popliteal fossa through defects in the posterior capsule, of which the commonest lies just above the head of gastrocnemius (Fig. 24.43 and Fig. 24.44). The result is a swelling at the back of the knee, which is uncomfortable more than painful and limits flexion. The pain is worse after walking and may be confused with intermittent claudication.
 |
| Fig. 24.43
A popliteal bursa. The bursa communicates with the synovial cavity of the knee.
|
 |
| Fig. 24.44
An arthrogram showing a ruptured popliteal cyst with contrast medium leaking into the soft tissues of the calf.
|
Popliteal cysts are usually an indication of pathology in the rest of the knee rather than a disorder in their own right. Rheumatoid arthritis, gout and tuberculosis can all produce a large painful popliteal swelling but osteoarthrosis and trauma are more common. Beware of calling these cysts ‘Baker’s cysts’. In 1877, William Morrant Baker described massive swellings that extended down to the ankle. The original Baker’s cysts were probably tuberculous or rheumatoid in origin and are very rare nowadays.
Popliteal cysts also occur in children and present as a firm or hard swelling in the popliteal fossa. The swelling often arouses the fear of malignancy but this anxiety can easily be allayed by transilluminating the lesion to demonstrate that it consists of fluid only.
Natural history
Untreated, popliteal cysts do one of three things:
1. Disappear gradually.
2. Rupture suddenly, when they mimic a deep vein thrombosis. The calf becomes hot, tender and red and the patient may be admitted under the physicians and given anticoagulants. An arthrogram will confirm the diagnosis by showing the synovial leak into the calf.
3. Become so tense and painful that excision is required.
Treatment
Because most popliteal cysts disappear spontaneously, operation is seldom required. The joint should be investigated to exclude gout, rheumatoid arthritis or an internal derangement and any underlying cause treated. The patient should be warned that the cyst may rupture, so that they can avoid needless anticoagulation. If the cyst does rupture, rest and analgesics are all that is needed.
Excising a popliteal cyst is an extensive procedure, involving a dissection of the popliteal fossa; recurrence of the cyst is possible.
Ligamentous instability
Anterior cruciate instability
Clinical features
Patients with anterior cruciate instability give a very characteristic history, beginning with a violent injury in which the patient felt something break in the knee when tackled or twisting awkwardly (p. 259). Most patients remember the incident vividly, even many years later. The knee swelled after the injury and the swelling gradually subsided. Ever since then the knee collapses when the patient puts weight on it and twists and, although able to run fast in straight lines, he or she must slow down to turn corners.
Some patients only have symptoms when the knee is under great stress on the football field but some knees are so unstable that they collapse if the patient turns round when walking over a level floor, while walking over cobbles or uneven ground is quite impossible.
Roughly one patient in three needs reconstruction following anterior cruciate rupture. The remainder are evenly divided between those who have occasional minor problems and those who have no symptoms whatever.
Comparison with meniscal injuries. The history of anterior cruciate instability is very different from a meniscus lesion.
Differences between anterior cruciate rupture and meniscal lesions
1. Cruciate symptoms are caused by a high speed twisting or a deceleration injury with the knee almost straight, the meniscus lesion by low speed movements with the knee bent.
2. Patients stop playing after a cruciate injury.
3. Ligament injuries usually follow a memorable injury, meniscal injuries seldom do.
4. Menisci can lock the knee and block extension, but ligament injuries cause collapsing.
The diagnosis can be difficult if the patient has both a meniscal tear and an anterior cruciate injury, with locking as well as collapsing, but the two elements can be separated if the history is taken intelligently.
Mechanics
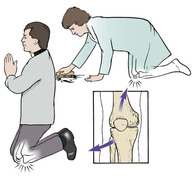
The instability is caused by the odd design of the lateral compartment of the knee, which consists of two convex surfaces that slip off each other when the compartment is loaded. Only the anterior cruciate holds the lateral condyle and the lateral plateau in the correct relationship (Fig. 24.45).
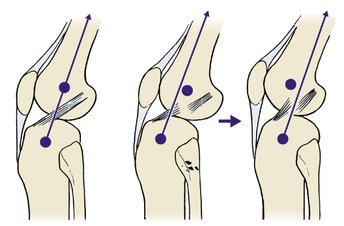 |
| Fig. 24.45
Mechanism of the ‘pivot shift’ phenomenon. If the anterior cruciate ligament is ruptured, the short arched lateral tibial plateau can slip in front of the femoral condyle. As the knee is flexed, the iliotibial tract moves behind the axis of rotation and the bones reduce with a thud.
|
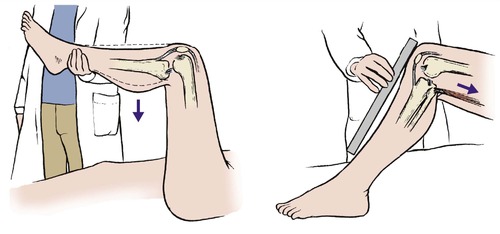
Clinical examination
Testing for anterior cruciate laxity is difficult. The hamstrings must be fully relaxed to elicit the anterior drawer sign, but even with the hamstrings tight, Lachman’s test (p. 29) is usually positive. The pivot shift test, in which the knee is flexed while loading the lateral compartment, will reproduce the patient’s symptoms, but the test is difficult and requires considerable experience.
Treatment
Conservative treatment cannot restore the integrity of the ligament but it can restore function.
Physiotherapy should be directed to building up the hamstrings so that they will help pull the tibia backwards on the femur and help make good the deficiency of the cruciate. Quadriceps exercises work in the opposite direction and may be counterproductive.
Many patients are content to adjust their life to their disability by giving up violent sports, and this should always be discussed with the patient.
Surgical treatment. If the symptoms interfere with everyday activities and conservative measures have failed, reconstruction of the anterior cruciate may be needed. This is a complex operation requiring much rehabilitation and at least 6 months away from sport. Two types of operation are available:
1. Replacement of the anterior cruciate, either with natural tissue or an allograft.
2. An extracapsular repair using the iliotibial tract.
The treatment of choice is an intra-articular reconstruction using the middle third of the patellar tendon or a four-strand hamstring graft. The use of an extra-articular reconstruction using the iliotibial tract may play a part in stabilizing the lateral structures.
The results remain satisfactory in about 80% of patients 5 years after operation.
Prosthetic ligaments have been described and discarded since about 1918. None has remained on the market for more than a few years because the long-term results are poor.
Chronic posterior cruciate instability
Posterior cruciate ruptures cause fewer problems than anterior cruciate injuries, but when they do, they are often intractable.
The usual symptoms of posterior cruciate deficiency are a feeling of unsteadiness when descending slopes or putting weight on the bent knee.
The posterior cruciate is ruptured in two ways:
1. A blow to the front of the knee in flexion.
2. Hyperextension.
If the patient gives a history of such an injury, or has a scar at the upper end of the tibia consistent with a blow, posterior cruciate rupture should be suspected.
Clinical examination
The injury can be distinguished from anterior cruciate rupture because the posterior sag sign is positive (Fig. 24.46). This can look a little like an anterior drawer sign but is easily distinguished by observing the knee from the side.
 |
| Fig. 24.46
Posterior cruciate rupture. The tibia sags backwards when the foot is lifted. A ruler run from the patella to the front of the shin shows the tibia sagging backwards.
|
Treatment
Quadriceps function can compensate for posterior cruciate instability. Operation is difficult, unreliable and indicated only if the symptoms are disabling. Many well-known athletes have returned to their former level of achievement after conservative treatment alone.
Medial ligament instability
For practical purposes, rupture of the medial collateral ligament alone does not cause symptoms unless it is accompanied by an anterior cruciate rupture. Management of the acute injury is described on page 261.
Patients with medial ligament injuries experience unsteadiness when the leg is caught awkwardly by a sideways blow to the foot.
Treatment
Reconstruction is difficult. The symptoms in most patients are due to the associated anterior cruciate ligament injury and are relieved by anterior cruciate reconstruction.
Anterior knee pain
Patellofemoral joint
Pain at the front of the knee usually comes from the patellofemoral joint, which is quite separate from the tibiofemoral joint. This joint is stressed when the knee is flexed under load, as when squatting or descending stairs, but there are many other causes (Fig. 24.47).
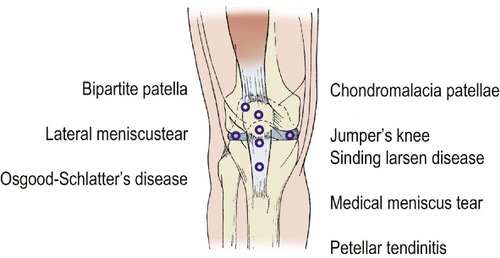 |
| Fig. 24.47
Causes of pain around the front of the knee.
|
The mechanics of the joint means that it takes up to seven times the weight of the body when loaded in flexion and it is therefore exposed to enormous stresses. The pain is felt around the knee cap and patients usually indicate the site of the pain by rubbing the palm of the hand over the knee cap. The pain can be serious enough to curtail sports or even make it difficult to climb stairs.
The articular surface may be abnormal but pain can also arise from structures around the joint.
Adolescent anterior knee pain
Anterior knee pain is a particular problem in adolescence. Girls between 13 and 15 years old are most often affected and the pain may be so severe that they are unable to take part in sports or even move between classrooms at school.
On clinical examination there are usually very few physical signs but the patella may be tender to the touch. A few have reflex sympathetic dystrophy (p. 309) in the early stages before the colour changes are present.
In many patients, no cause can be found but a plausible explanation is that during the adolescent growth spurt the load on the joint increases suddenly because of the rapid rise in body weight and muscle power. This, combined with the lengthening of the lower limb bones, which increases the leverage applied to the knee, increases the load across the patellofemoral joint very markedly.
The great majority of adolescents with anterior knee pain recover spontaneously without treatment. Provided there is no mechanical element to their symptoms, such as clicking, collapsing or an effusion, a gradual recovery can be expected over a period of 1 or 2 years.
Treatment
If there are no mechanical symptoms or signs and the radiograph is normal, the patient can safely be observed at regular intervals, perhaps every 6 months, until the symptoms settle.
Physiotherapy is unlikely to be helpful and may aggravate the pain. Operation, including arthroscopy, should be avoided at all costs. It is not possible to see pain down an arthroscope and the trauma of any procedure may precipitate reflex sympathetic dystrophy.
If it is necessary to exclude an internal derangement, MRI is preferable to arthroscopy. The mainstay of treatment is sympathy and regular reassurance until the pain resolves.
Chondromalacia patellae
Beware of the term ‘chondromalacia patellae’: it means only softening of the articular cartilage of the patella but is commonly used as a synonym for anterior knee pain in an adolescent.
Because the stresses on the patellofemoral joint are so great, some areas of articular cartilage are overloaded and become soft and swollen. This condition is known as chondromalacia patellae and is probably reversible in early cases. In some patients, the softened surface develops fissures and begins to break up, producing a condition which is, in effect, early osteoarthritis.
Chondromalacia patellae is only one cause of anterior knee pain – there are many others.
Treatment
The patient should be treated like other adolescents with anterior knee pain (see above) unless they develop definite crepitus or clicking under the patella. They will then require arthroscopic surgery to smooth irregularities on the patellar surface. The prognosis for patellae with articular surface irregularities is poor and many develop patellofemoral osteoarthritis later.
Lateral pressure syndrome
In a few patients the patella does not sit as firmly in the femoral trochlea as it should. Instead, it tilts so that the lateral facet runs along the lateral edge of the femoral trochlea.
On examination the pain is localized to the lateral edge of the patella. Untreated, such patellae will probably develop patellofemoral osteoarthritis of the type shown in Figure 24.48.
 |
| Fig. 24.48
Osteoarthritis of the patellofemoral joint, involving the lateral facet of the patella.
|
Treatment
There is no reliable conservative treatment. If the symptoms persist for more than 6 months, lateral release to divide the lateral structures of the extensor retinaculum may be needed. This procedure allows the patella to resume its correct position and relieves pain in about 75% of patients, but it requires vigorous physiotherapy afterwards and recovery is often slow.
Note: Lateral release does not help undiagnosed anterior knee pain or chondromalacia patellae.
Synovial shelf syndrome (plica)
A fold of synovium, the medial synovial shelf, lies against the medial femoral condyle in flexion and can be irritated by trauma or prolonged pressure against the condyle. If the shelf is the cause of pain, the patient will point to it with an index finger.
Treatment
If the symptoms do not settle with time, they can be relieved by excising the synovial shelf arthroscopically.
Jumper’s knee
Jumper’s knee is similar to tennis elbow (p. 371) and occurs at the insertion of the patellar ligament onto the lower pole of the patella (Fig. 24.49). The patient cannot jump vigorously and athletic performance is affected.
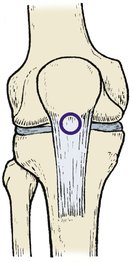 |
| Fig. 24.49
Jumper’s knee. The lower pole of the patella is tender at the centre of the patellar tendon attachment.
|
Treatment
Treatment is similar to tennis elbow. If three injections of hydrocortisone acetate at the site of pain (but not into the tendon) are unsuccessful, the area must be explored and the tissues drilled or scarified. Return to sport is unusual within 6 months of this procedure.
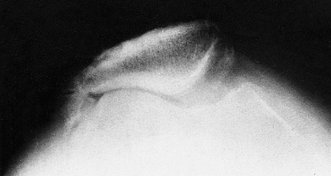
Bipartite patella
Some patellae have a separate fragment at the superolateral corner but it is not agreed whether this is congenital or acquired (Fig. 24.50). The condition is often bilateral.
 |
| Fig. 24.50
Bipartite patella.
|
Treatment
Operation is seldom needed but, if the separated fragment is painful or tender, excision of the separated fragment or a lateral release of the extensor mechanism will usually relieve pain.
Patellofemoral osteoarthritis
If the patellar surface develops osteoarthritis, the patient will be unable to bend the knee under load without pain. The rough areas cause crepitus, which is felt as an unpleasant grating ‘like broken biscuits in the knee’ when the patellofemoral joint is loaded, and in some patients the crepitus is audible. The lateral facet is affected more than the medial (see Fig. 24.48) and the condition is common in patients over the age of 40.
Treatment
No conservative treatment is really effective, apart from weight reduction, analgesics, and anti-inflammatory drugs. If the pain is severe, patellectomy will be needed to replace the rough surface of the patella with smooth tendon. After removing the patella, the tendon is carefully repaired and physiotherapy begun to restore joint movement and quadriceps strength.
The tibiofemoral joint is not involved in patellofemoral osteoarthritis and the two joints can be considered separately. It must be remembered, however, that if the tibiofemoral joint is badly affected by osteoarthritis a patellectomy will make a total knee replacement very difficult.
Anterior knee pain in the obese patient
Because the patellofemoral joint takes about seven times body weight during flexion, obese patients are particularly vulnerable to patellofemoral pain. Many of these patients have pushed the articular surface of the patella past its design limits and have done irreparable damage to their joint.
Treatment
No treatment is effective and it is folly to advise operation in such a patient unless their weight can be brought within normal limits.
Housemaid’s knee (prepatellar bursitis)
The prepatellar bursa is a normal structure which allows the skin to slide easily over the patella as the knee is flexed (Fig. 24.51). If the bursa becomes infected, injured or inflamed, fluid will accumulate inside the bursa and a swelling will appear in front of the patella in a characteristic position, which distinguishes it from an effusion of the knee. Sometimes a small fibrinous body forms in the bursa and causes severe pain on kneeling.
 |
| Fig. 24.51
Housemaid’s knee and clergyman’s knee. Housemaid’s knee affects the prepatellar bursa; clergyman’s knee affects the infrapatellar bursa.
|
In days past, before mechanization, housemaids spent much of their working days kneeling and leaning slightly forwards while scrubbing floors and doing other household tasks. Today, ‘housemaid’s knee’ is an occupational hazard of carpet layers, tilers and roofers, all of whom should use protective pads when kneeling.
Treatment
The swelling usually subsides with rest but in some patients an injection of hydrocortisone acetate into the bursa is needed. If this is ineffective and the swelling recurs, excision is required. Patients with gout are particularly susceptible to prepatellar bursitis, as well as olecranon bursitis (p. 372) and the bursitis is likely to remain or recur unless the gout is treated.
Clergyman’s knee (infrapatellar bursitis)
The infrapatellar bursa, which lies in front of the tibial tubercle, can also be inflamed. The condition is called clergyman’s knee because priests kneel in a more upright position than housemaids and take the load on the tibial tubercle instead of the patella.
Treatment
Treatment is the same as for prepatellar bursitis.
Patellar instability
The patellofemoral joint has little mechanical congruity and the patellar ligament is not in the same straight line as the quadriceps. The angle between the patellar ligament and the quadriceps is about 20° in the normal population and this angle is known as the Q angle (Fig. 24.52).
 |
| Fig. 24.52
The ‘Q’ angle: (a) the extensor mechanism does not run in a straight line from origin to insertion; (b) a lateral force is applied to the patella when the quadriceps contracts.
|
If any of these features is abnormal, e.g. an abnormally small or high patella (patella alta), generalized ligamentous laxity or dysplasia of the lateral condyle of the femur, patellar instability is likely.
Recurrent dislocation of the patella
Recurrent dislocation of the patella is a problem during adolescence, especially in girls because they have looser ligaments and smaller bones than boys. The dislocation is usually caused by a twisting movement of the knee in slight flexion and each generation appears to develop its own dance designed to displace the patella (see Fig. 14.30).
The patient usually knows if the patella has slipped out of place but if it reduces quickly the condition can be mistaken for an internal derangement. Other patients will say that their knee dislocates and this can be misleading.
Treatment
If the patella has dislocated three times and the patient has stopped growing, surgical stabilization is indicated. (Management of acute dislocations is described on page 256).
Stability can be achieved in several ways:
1. Releasing the lateral structures.
2. Realigning the quadriceps mechanism by transferring the tibial tubercle medially, thus reducing the Q angle.
3. Moving the tibial tubercle distally to bring the patella lower down in the femoral trochlea.
4. Tightening medial structures.
The choice of operation depends on the anatomical problem to be treated. Knees with normal anatomy and ligaments usually require only a lateral release but medial tibial tubercle transposition is needed if there is abnormal ligamentous laxity. Those with a small high patella require distal and medial transposition of the tibial tubercle combined with lateral release and perhaps medial plication.
Habitual and congenital dislocation of the patella
Habitual and congenital dislocation of the patella are different from recurrent dislocation (Fig. 24.53). In habitual dislocation the patella dislocates with every flexion of the knee, often because of abnormal tightness of the lateral structures. This may be the result of fibrosis following trauma, or injections into the vastus lateralis in the neonatal period.
 |
| Fig. 24.53
A permanent dislocation of the patella. Note the abnormal shape of the patella and the intercondylar groove.
|
Congenital dislocation of the patella is extremely rare and usually requires extensive surgery for its correction. The principles involved are the same as those for recurrent dislocation of the patella.
Osgood–Schlatter’s disease and Sinding Larsen’s disease
These conditions also cause pain at the front of the knee and are described on pages 328 and 331.
Case reports
These cases represent the decision making process in hip replacement surgery.
Patient A
A 48-year-old male patient presented to the orthopaedic surgeon with increasing rest and night pain in the right hip. He had previously been a keen athlete. He did not recall a specific history of trauma, but there was a strong family history of joint related problems with both his father and elder brother having had hip replacements.
Over the past 2 years he had had increasing pain and discomfort of such severity that he was unable to carry out his normal day-to-day activities. He had modified his lifestyle by stopping sport, losing weight and taking appropriate analgesics and using a walking stick when needed. Despite this, the pain was unacceptable and the orthopaedic surgeon discussed with him the operative treatment of the significant osteoarthritic degeneration in the hip.
He subsequently underwent a resurfacing total hip replacement after having been made aware of the risks and results of this procedure.
Patient B
A 78-year-old retired gentleman presented to the orthopaedic surgeon with increasing pain and discomfort in the right hip. As with Case A, conservative management had not helped sufficiently and it was felt that he needed a hip replacement.
He subsequently underwent a cemented Exeter total hip replacement.
Case C
A 22-year-old lady presented to the orthopaedic surgeon with a similar complaint of increasing pain and discomfort in the right hip. There was no clear history of a developmental dysplasia of the hip, but she had always recounted a ‘clicky’ hip and subsequent increasing pain.
Plain radiographs confirmed an acetabular dysplasia and an abnormal femoral neck shaft angle. It appeared that the hip was gradually progressing to an osteoarthritic hip and it was felt initially that she should have a hip arthroscopy to assess the chondral surfaces and labrum.
She subsequently went on to have a rotational acetabular osteotomy to cover the femoral head in the hope that this would prolong the life of the hip.
Summary
These three cases indicate different methods of management. In a very young patient it is important to try and preserve hip function for as long as possible.
In the middle-aged patient, when the symptoms are truly unacceptable and the patient has definitely failed conservative management then a hip replacement can be contemplated, but there are significant risks with this procedure. A resurfacing procedure may be beneficial as there is less resection of bone and this may, therefore, help in the long-term when this joint fails and a revision is contemplated.
In the elderly patient, again when conservative treatment has failed, a simple cemented total arthroplasty is indicated. The results of this are excellent in over 95% of cases.