DISORDERS OF THE GASTROINTESTINAL TRACT
DIARRHEA
General Therapy for Diarrhea
Diet. If nausea and vomiting do not prevent eating, adjust the diet:
Dehydration can be estimated as follows:
In a baby, dehydration is manifest as dry diaper (decreased urine output), sunken eyes, sunken “soft spot” (fontanel) on the top of the head, dry tongue and mouth, rapid pulse, poor skin color (blue or pale), lethargy (“floppy baby”), and fast breathing (greater than 30 breaths per minute in a small child, or 40 per minute in an infant). For purposes of estimation, a normal pulse rate (per minute) in a newborn averages 120; at 2 years, 110; at 4 to 6 years, 100; and at 8 to 10 years, 90.
Fluid replacement. If fluid losses are significant (more than five bowel movements per day), begin to replace liquids as soon as you can.
Antimotility (decreased bowel activity) drugs. If fever, severe cramping, and bloody diarrhea are absent, it is safe to use antimotility drugs, although they should be immediately discontinued if diarrhea lasts for more than 48 hours. If diarrhea lasts longer than 3 days, if the victim has a fever greater than 101°F (38.3°C), if he cannot keep liquids down because of vomiting, if there is blood in or on the stool, if the abdomen becomes swollen, or if there is no significant pain relief after 24 hours, seek a physician immediately.
The antimotility drug of choice is loperamide (Imodium A-D). The initial adult dose is 4 mg (two 2 mg capsules, or 4 tsp—20 mL—of the liquid), followed by 2 mg after each loose bowel movement, not to exceed 16 mg (eight capsules) per day or 2 days of administration. With uncomplicated (no fever or blood in stools), watery diarrhea, this drug can be given to children age 2 years and older. Give children a 0.2 mg/kg (2.2 lb) of body weight dose every 6 hours. The liquid preparation contains 1 mg/tsp (5 mL).
For adults, diphenoxylate (Lomotil) is an alternative, but has side effects of dry mouth and urinary retention. Pepto-Bismol is another, less effective choice (see page 212).
Kaopectate (kaolin plus pectin) is of limited value; it does not shorten the course of diarrheal illness, and acts only to add a little consistency to stools. Lactobacillus preparations (acidophilus beverages or yogurt) do not shorten the course of acute diarrheal illness, but they may be useful to repopulate the gastrointestinal tract with normal bacteria after a severe bout of diarrhea or administration of antibiotics used to treat diarrhea.
In foreign countries, drugs are on occasion recommended for diarrhea without a specific diagnosis. These drugs include chloramphenicol (Chloromycetin), Enterovioform, MexaForm, Intestopan, clioquinol, and iodoquinol. This may be dangerous, because these drugs can have certain adverse direct effects or side effects. Therefore, they should not be taken without a specific diagnosis for which they are felt to be indicated.
Antibiotics. These should be used if diarrhea is moderate to severe (more than eight bowel movements per day), particularly if it is bloody and associated with severe cramping, vomiting, and fever.
Traveler’s Diarrhea
Traveler’s diarrhea (“turista,” “Kathmandu quickstep,” “Montezuma’s revenge,” “Delhi belly,” “Aztec two-step,” “Hong Kong dog,” and many other synonyms) is frequent, loose bowel movements (three or more loose stools in a 24-hour period associated with one or more of nausea, vomiting, abdominal cramps, fever, urge to defecate, cramping and straining with defecation, or bloody or mucus-laden stools) caused by waterborne or food-borne pathogens, most commonly produced by forms of the bacterium Escherichia coli, which is introduced into the diet as a fecal contaminant in water or on food. Someone has described it as “stool that fits the shape of the container.” When caused by E. coli, symptoms usually occur 12 to 36 hours after ingesting the bacteria, and include the gradual or sudden onset of frequent (four to five per day) loose or watery bowel movements, rarely explosive, and far less violent than diarrhea associated with classic food poisoning (see below). Fever, bloating, fatigue, and abdominal pain are of minor to moderate severity. Nausea and vomiting are less frequently found than with viral gastroenteritis. Most traveler’s diarrhea is caused by bacteria, but a small percentage may be caused by viruses or parasites.
People who would be advised to consider taking a drug to prevent infectious diarrhea include those with a significant underlying medical problem (such as acquired immunodeficiency syndrome [AIDS], inability to produce stomach acid, or inflammatory bowel disease) and those with an itinerary rigid enough that it would be catastrophic to the mission to be laid up with diarrhea.
Probiotics have not yet been demonstrated to reduce the risk of traveler’s diarrhea.
One important topic is how best to wash dishes to remove diarrhea-causing bacteria and viruses. One effective washing-up system is removal of most food residue with detergent (5 milliliters or 1 teaspoon) in the water in bowl 1, followed by a finishing wash (scrub until clean) with bleach (10 milliliters or 2 teaspoons of 4% chlorine bleach) in the water in bowl 2, followed by a final rinse in drinkable water in bowl 3. The final rinse is felt to remove the taste of the detergent and bleach (the latter considered to be a disinfectant). A few final recommendations are to use hot water in bowl 1, use a scouring pad or brush in bowl 2 with the bleach to avoid contamination of the scourer, allow all utensils to air dry after washing, and clean the washing-up bowls and allow them to dry between uses. Another suggestion is to use up to 100 milliliters or 20 teaspoons (3 teaspoons = 1 tablespoon) of bleach in bowl 2 if there is a current outbreak of diarrhea and vomiting. This increases the disinfection power of the second bowl.
Water disinfection is discussed on page 433. Stick to boiled water, food that is served steaming hot, dry foods (bread), bottled carbonated beverages, and reputable food establishments. Alcohol in mixed drinks does not disinfect water. Packaged butter and packaged processed cheese are usually safe to eat. Unpasteurized dairy products should be avoided. Avoid casseroles, quiches, lasagna, and other foods that are prepared in advance and then may be allowed to sit for a prolonged period before consumption. During that time period, they can be contaminated by bacteria from fingers, insect legs, and contaminated serving utensils. With regard to seafood, raw or undercooked products, particularly shellfish, are especially hazardous. Vibrio organisms—which cause, among other problems, cholera—frequently reside in crabs and oysters. Cook all shellfish for a minimum of 10 minutes of boiling, or 30 minutes of exposure to full steam.
E. coli O157:H7
Escherichia coli O157:H7 is a bacterium that has been transmitted by as few as 10 bacteria in raw or undercooked hamburger meat, fruit juices, and other food with fecal contamination. It can be spread person to person, and has also been transmitted by petting animals, contacting animal manure, and swimming in recreational pool water. After ingesting the bacteria, an infection may occur after an incubation period of 1 to 10 days, with 3 days being the average delay between exposure and illness. It causes a syndrome of fever or no fever, abdominal pain, vomiting, and nonbloody diarrhea, followed in a few days by bloody diarrhea, dehydration, weakness, anemia, and kidney failure. There is not yet an effective treatment with antibiotics. In fact, therapy with some antibiotics may contribute to more severe illness. Prevention means strict handwashing before eating and cooking ground beef until it is no longer pink (160°F). Do not mix raw and cooked foods, particularly meat. After you cook meat, do not serve it on the unwashed dish that carried the raw food. Since raw meat, especially beef, can be a problem, be certain to wash hands, cooking utensils, cutting boards, dishes, and counters after they have been in contact with raw meat. Milk and fruit juices prepared from crushing processes require pasteurization. Understand that in the absence of pasteurization, which is a heating process, no product can be guaranteed to not be contaminated with the bacteria normally killed in the pasteurization process. Many of us like to drink fresh fruit juice. When we do so, we take a risk, usually, quite minor, that it may be contaminated. In the presence of someone with any cause of diarrhea, excellent handwashing technique should be observed. If a person is ill with a diarrheal illness, he or she should not prepare food for others or share common bodies of swimming or bathing water. Try to not swallow lake or swimming pool water.
Giardia Lamblia
If more than 10 to 25 cysts are swallowed, the organisms establish residence in the duodenum and jejunum (first parts of the small bowel), and after an incubation period of 7 to 20 days emerge in another form (trophozoite) to cause stomach cramps, flatulence, a swollen lower abdomen, often explosive and foul-smelling watery (“floating”) diarrhea, “rotten” (sulfurous) belching, and nausea. Fever and vomiting are unusual except in the first few days of illness. Foul flatus and abdominal cramping are common. Because of the delay in onset after ingestion of the cysts, many a backpacker develops “backpacker’s diarrhea” or “beaver fever” after he returns to civilization, and he does not make the mental connection to his recent journey. If the diarrhea becomes chronic, the victim can lose appetite, lose weight, and become weak. Diagnosis is made by a physician who recognizes trophozoites or microscopic cysts in the stool of the victim, takes a sample of mucus from the duodenum, or is confident with a clinical diagnosis.
Other Infectious Diarrheas
Diarrhea-causing pathogens cause a constellation of fever, chills, nausea, vomiting, diarrhea (with or without mucus and blood), weakness, and abdominal pain. Because the clinical picture can be similar with infection from all of these organisms, the differentiation frequently relies on examination of the stool under the microscope and/or culture of the stool to identify the specific pathogen. For the sake of the brief expedition, the treatment is the same: rehydration with copious amounts of balanced electrolyte solutions, and antimotility agents only when essential to prevent severe dehydration. If the victim suffers from high fever with shaking chills, has persistent bloody or mucus-laden bowel movements, or is debilitated by dehydration, he should seek the care of a physician. Meanwhile, the administration of ciprofloxacin (Cipro) 500 mg two times a day or azithromycin 500 mg once a day for 3 days will treat E. coli and Shigella, may eradicate Salmonella, and will not adversely affect other infections. As soon as the victim of persistent diarrhea returns to civilization, he should visit a physician for a thorough evaluation. If the ova or parasitic forms of amoebae are seen during microscopic examination of stool, other drugs, such as tinidazole, metronidazole, diloxanide furoate, paromomycin, or diiodohydroxyquin, may be prescribed. If the ova or parasitic forms of worms are seen, drugs such as mebendazole or pyrantel pamoate may be prescribed.
CONSTIPATION
To relieve the victim of mild constipation, try the following measures:
2. Adjust the diet (more for prevention than treatment).
3. Consider the use of a stool softener (mineral oil; docusate sodium: Colace, Regulax SS, Surfak); bulking agent (psyllium: Metamucil, Perdiem, Fiberall; methylcellulose: Citrucel; polycarbophil: Fibercon, Equalactin, Konsyl); osmotic laxative (magnesium hydroxide: Phillips’ Milk of Magnesia; magnesium citrate: Evac-Q-Mag; sodium phosphate: Fleet Enema, Fleet Phospho-Soda, Visicol), natural laxative (prune juice), poorly-absorbed sugar (lactulose: Cephulac, Chronulac, Duphalac); polyethylene glycol and electrolytes: Colyte, GoLYTELY, NuLYTELY; polyethylene glycol: Miralax, and/or stimulant laxative (cascara sagrada: Colamin, Sagrada-lax; senna: Senokot, Ex-Lax; castor oil: Purge, Neoloid, Emulsoil). Peri-Colace is a combination of the stool softener docusate sodium and casanthranol, a laxative. Other drugs are listed on page 500.
4. In general, it is best to avoid the use of repetitive enemas or potent laxatives, because they can cause large fluid losses. A useful enema is a Colace 5 mL (200 mg) “microenema.” A child may benefit from a plain glycerin suppository. In general, enemas can cause cramping and bloating. If they contain electrolytes, such as magnesium or phosphate, they can cause elevated levels of these in the bloodstream. Typical enemas include 6 to 12 ounces of milk and an equal portion of molasses; 2 tablespoons of Epsom salts per quart of lukewarm water; 45 mL of Phospho-Soda with 2 quarts of water; 9 mL packet of Castile soap in 2 quarts of tap water; 30 mL of mineral oil in 1 to 2 quarts of water; and 1 to 2 quarts of warm (body temperature) tap water.
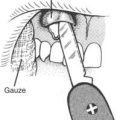
5. If a victim becomes impacted (has not had a bowel movement for 5 to 10 days due to constipation), using stool softeners will probably be ineffective, and piling on an ingested load of bulky fiber is just dumping more backfill behind the dam. Unfortunately, to break the roadblock, you may have to perform the physical removal of stool from the rectum, using a softening enema first and then a gloved finger for the extraction. This should be done gently, to prevent injury to the anus and walls of the rectum. Two fingers are used to dilate the anus, then the stool is broken up with a scissoring motion. After as much stool as possible is removed manually, an enema should be used.
HEMORRHOIDS
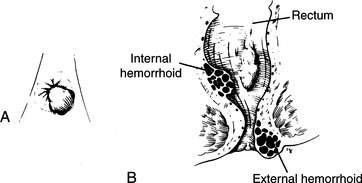
Hemorrhoids are enlarged veins that are found outside (external hemorrhoids) or inside (internal hemorrhoids) the anal opening (Figure 118). They cause problems that range from minor itching and skin irritation to excruciating pain, inflammation, and bleeding. The bleeding is noticed as bright red blood either on the outside of the stool (not mixed in with the excrement), in the toilet water, or on the toilet paper. Bleeding is usually sporadic, associated with difficult bowel movements (constipation) with straining, and passage of hard stools. To avoid problems, keep your stools soft. If hemorrhoids flare, the treatment is sitz (sitting) baths in warm water for 30 minutes three times a day, and the application of medication in the form of cream, ointment, or suppositories (Preparation H [essentially a petrolatum lubricant]; Anusol or Tronolane [with pramoxine 1% for pain and itching] or Anusol HC-1 [without pramoxine, but with hydrocortisone 1% for inflammation]; Nupercainal [1% dibucaine]; pramoxine hydrochloride 1% with hydrocortisone acetate 1% [proctoCream-HC]; ELA-Max 5 [lidocaine 5%] anorectal cream; Analpram-HC cream or ointment [hydrocortisone and pramoxine]). Unless bleeding is severe, it can be managed with sterile pads and gentle pressure. If the victim develops a fever associated with severe rectal pain or cannot pass a bowel movement, a physician should be sought.
HEARTBURN
Heartburn is a manifestation of esophageal reflux (in medical parlance, sometimes called gastroesophageal reflux disease [GERD]), in which stomach contents containing acid and food travel backward from the stomach into the esophagus. This causes irritation and pain, which is typically sharp or burning and located under the breastbone and/or in the upper abdomen. It may be associated with belching, a sour taste in the mouth, and/or near-vomiting. When severe, the pain may be confused with angina (see page 49). Omeprazole (Prilosec) is a drug that suppresses gastric acid secretion. It can be prescribed for a 1- to 2-week period by a physician for GERD or for up to a 4- to 8-week period for severe erosive inflammation of the esophagus (adult dose 20 to 40 mg by mouth in the morning and 20 mg in the evening). Other drugs in this category (“proton pump inhibitors”) are pantoprazole (Protonix) and rabeprazole (AcipHex). Mild heartburn is often managed with antacids, particularly Gaviscon, which forms a “foam” that floats on the stomach contents and protects the esophagus from refluxed acid. Metoclopramide hydrochloride (Reglan) helps control muscle tone at the sphincter (junction) between the stomach and the esophagus, and thus helps prevent reflux. Nizatidine 75 mg (Axid AR [“acid reducer”]) is an H2-blocker drug (see page 501) that inhibits gastric acid secretion. It is swallowed 30 to 60 minutes before eating, and can be used up to twice in 24 hours. Cimetidine (Tagamet) 200 mg can be used in a similar manner. Famotidine (Pepcid AC) 10 or 20 mg twice a day (preferably ingested 15 to 60 minutes before eating) for up to 6 weeks is another therapy.
NAUSEA AND VOMITING
Nausea and vomiting may arise from causes as simple as anxiety, or may represent a serious problem such as appendicitis, ingestion of a poisonous plant, or response to a head injury. When vomiting is secondary to a serious underlying disorder, the basic problem must be remedied. Any victim with nausea and vomiting who suffers from altered mental status, uncontrollable high fever, extreme abdominal pain, or chest pain that might represent heart disease—or who is either very young or very old—should be evacuated promptly. Anyone who vomits blood should be taken to a hospital immediately. Vomiting in children is particularly worrisome if it accompanies head trauma (see page 61), abdominal trauma (see page 119), or lethargy or confusion (which might represent an infection or poisoning); severe vomiting (which might represent a bowel obstruction [see page 127] or appendicitis [see page 126]) is also of concern.
If nausea and vomiting due to gastroenteritis become excessive, they can be managed with an antiemetic. One effective drug is ondansetron (Zofran). The adult dose is one 4 mg dissolving tablet every 8 hours; the pediatric dose is 0.15 mg/kg of body weight of the oral dissolving tablet every 6 to 8 hours. Alternative drugs are prochlorperazine (Compazine), which can be administered orally or as a suppository, promethazine (Phenergan), which comes in suppository form, or trimethobenzamide (Tigan), which can be taken orally or by suppository. If the victim is so ill that he cannot keep anything in his stomach, it makes no sense to administer an oral medication, so an injection or suppository must be used. A person who requires medication to control vomiting should see a physician. After multiple episodes of vomiting, the victim may suffer from dehydration (see page 207), particularly if there is associated diarrhea as part of a gastroenteritis. Fluid replacement is essential. The diet should be advanced slowly as the victim’s hunger returns.
Nausea and vomiting due to motion sickness are discussed on page 440. Cyclical vomiting is a disorder in which the victim experiences fatigue and nausea, and perhaps sweating and pale skin color for approximately 90 minutes before onset of explosive vomiting, which may last for up to 24 hours in children and 3 days in adults. The victims may vomit up to 6 times per hour. This disorder, which may sometimes be accompanied by abdominal pain, can be triggered by stress, an upper respiratory tract infection, menses, sleep deprivation, certain foods, asthma attacks, motion sickness, or environmental allergies. Treatment is supportive and based on symptoms. If an attack is severe, the victim may require intravenous hydration.
ULCER DISEASE
The major symptom of ulcer disease is burning, sharp, or aching pain in the upper abdomen that is usually relieved by the ingestion of food or antacids, although the latter alone may be therapeutic. Classically, the pain occurs when the stomach is empty, particularly during times of emotional stress. Because the greatest amounts of acid are secreted following meals and between the hours of midnight and 3:00 a.m., these are times when pain is most frequent.
Therapy
1. Antacids. These are the traditional mainstay of therapy and should be taken in a dose of 2 to 3 tbsp (30 to 45 mL) 1 and 3 hours after meals, at bedtime, and as necessary to control pain. Liquids are generally more effective than tablets. Solid food and milk are not recommended as antacids. While they may decrease pain briefly, they actually stimulate the secretion of acid.
2. Drugs to inhibit the secretion of acid. Medications used to decrease acid secretion (antagonists to histamine H2 receptors [H2RAs] and proton [acid] pump inhibitors [PPIs]) decrease bowel activity and cramping.
3. Drugs to protect the lining of the gastrointestinal tract. Sucralfate (Carafate) is a drug that binds with the ulcer and protects the bowel lining from further erosion. Because it requires the presence of acid in the ulcer crater to be activated, it should not be given at the same time as antacids.
4. Avoidance of alcohol, tea, coffee, tobacco, and known gastric irritants.
5. Do not use household baking soda to neutralize acid in the stomach. Baking soda (bicarbonate) reacts with the acid to liberate heat and gas.
HEPATITIS
Hepatitis is inflammation of the liver that is caused by viral infection or parasitic infestation, drugs, toxic chemicals, alcohol abuse, or autoimmune disease. Type A infectious (short-incubation) hepatitis is the more commonly encountered viral form. The virus is excreted in urine and feces and contaminates drinking water and food products (such as raw shellfish). Type B infectious (long-incubation) hepatitis is caused by a virus found in many body fluids (blood, saliva, semen) and is spread by direct person-to-person contact. Type C infectious hepatitis (formerly non-A, non-B hepatitis) is caused by at least one virus and is most commonly associated with blood transfusions. Multiple other forms of viral hepatitis have been discovered by medical researchers.
Protection against hepatitis is best accomplished by prevention of virus transmission through good hygiene. Hepatitis A vaccine is available (see page 454). In countries of high hepatitis incidence (poor sanitation, infested water or food), pooled immune serum globulin (ISG, or gamma globulin) injections are advised (see page 454); these protect unimmunized people against hepatitis A, and diminish symptoms in infected people. In a recent study that compared hepatitis A vaccine against ISG for postexposure prophylaxis against hepatitis A in persons who had not been previously immunized, it appeared that they were roughly equivalent, with the ISG being slightly more effective at preventing hepatitis A. Hepatitis B vaccine (see page 454) is intended for health care workers or those who will visit or reside in regions of high endemicity. It is of little benefit against hepatitis A.