Chapter 4 Disorders of keratinization
Ichthyosis vulgaris (Fig. 4-1A,B) usually develops around school age, and is characterized by generalized xerosis and scale, with characteristic sparing of the flexural skin. Additional findings include follicular accentuation (keratosis pilaris), hyperlinearity of palms and soles, and a personal or family history of atopy. Rare patients may have an associated palmar-plantar keratoderma. Skin biopsy demonstrates a decreased granular cell layer associated with moderate hyperkeratosis.
X-linked ichthyosis, in contrast, is usually present by one year of age, affects the posterior neck with “dirty”-appearing scales, and spares the palms and soles (Fig. 4-1C). The skin changes—gradually worsening with age—with the neck, face, and trunk ultimately developing thick, brown scales. The disease is caused by a defect in steroid sulfatase, an enzyme important in cholesterol synthesis and vital for normal development and function of the stratum corneum. Accumulation of cholesterol sulfate and a lack of tissue cholesterol ensue, leading to a disturbance in steroid hormone metabolism. Skin biopsy of X-linked ichthyosis is rarely diagnostic, and demonstrates a normal granular layer with hyperkeratosis.

Figure 4-2. Fatal case of harlequin fetus demonstrating large, fissured, keratotic platess.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)

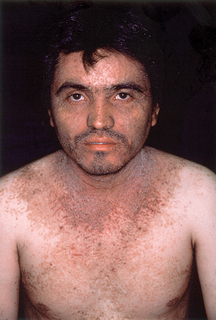
Figure 4-3. Acquired ichthyosis due to clofazimine.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
Homayoun A: Acquired ichthyosis and related conditions, Int J Dermatol 23:458–461, 1984.

Figure 4-5. Hailey-Hailey disease showing a patch of minute vesicles, erosions, and crusting in the antecubital fossa.
Key Points: Disorders of Keratinization
Burge SM: Management of Darier’s disease, Clin Exp Dermatol 24:53–56, 1999.