Eye Disorders
Most eye disorders tend to present as ‘red eye’. It is the single most common ophthalmic complaint encountered by general practitioners.
History
Pain
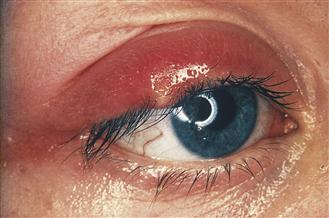
Most disorders of the eye present with pain. Sudden onset of unilateral eye pain and lacrimation may be due to a foreign body. Patients with infective conjunctivitis tend to complain of a soreness rather than true pain. Patients with blepharitis complain of a foreign body sensation or grittiness, whereas patients with allergic conjunctivitis (hayfever, acute allergy or atopy) tend to complain of itching rather than pain. Severe pain is experienced with corneal abrasions, ulcers, angle-closure glaucoma, herpes zoster ophthalmicus, uveitis and scleritis. Patients with either of the last two conditions experience exacerbation of pain on palpating the globe. A stye is a suppurative inflammation of an eyelash follicle. It is common and extremely painful. A meibomian cyst is an infection of a meibomian gland, which is in the posterior half of the eyelid margin. Following inflammation of a meibomian gland, it may either resolve spontaneously or leave a pea-size swelling known as a chalazion. Entropion is the rolling inwards of the lid margin. The eyelashes irritate the conjunctiva and cornea, causing a painful red eye. The opposite condition is known as ectropion and usually results in a watery eye. Subconjunctival haemorrhages are usually spontaneous and, although they may present with impressive chemosis (soft-tissue swelling), they are not usually painful.
Visual disturbance
Impairment of vision can occur with corneal ulceration, uveitis and acute angle-closure glaucoma. This is usually associated with photophobia. In addition, patients with glaucoma may perceive halos around lights due to corneal oedema.
Discharge
Documenting the presence, amount and colour of any discharge originating from the eye is important. A purulent discharge is associated with bacterial and chlamydial conjunctivitis, and a clear discharge with allergic and viral conjunctivitis.
Past medical history
A history of atopy or hayfever may be present in patients with allergic conjunctivitis. Previous herpes infection on the face may be the only clue with dendritic corneal ulceration. Conjunctivitis, urethritis and arthritis form the triad of Reiter’s syndrome caused by Chlamydia trachomatis infection. A history of contact lens use is important, as patients may develop sight-threatening infections acutely.
Scleritis is a deeper and more severe inflammatory process than episcleritis. It tends to be associated with connective tissue diseases, such as rheumatoid disease and SLE.
Uveitis is associated with inflammatory bowel disease, psoriasis, ankylosing spondylitis and sarcoidosis. Orbital congestion may be seen in patients with thyroid disorders. Xanthelasma are fatty plaques in the skin of the eyelids. Extensive or multiple xanthelasma may indicate abnormalities of cholesterol metabolism, diabetes or arterial disease.
Examination
Visual acuity should be assessed with correcting spectacles or pinhole, and documented with reference to a Snellen chart. Conditions that present with visual impairment are corneal ulceration, uveitis and glaucoma. Patients with these conditions should be referred to an ophthalmologist. The eyelids should be carefully inspected. Swelling of the upper eyelid with redness may indicate a stye. There may be a bead of pus apparent at the infected hair follicle. The upper eyelid is everted to inspect for a meibomian cyst and foreign bodies. Papillae (conjunctival elevations with a vessel in the centre) are seen with allergic conjunctivitis, and follicles (collections of lymphocytes) may be visible with viral or chlamydial infection. Ectropion and entropion are usually obvious: in the former the lower eyelid is everted and in the latter it is inverted, the eyelashes scratch the conjunctiva and cornea giving rise to a red, watery eye. A similar effect is produced by trichiasis, which is caused by irregular pointing lashes. Xanthelasma are fatty plaques in the skin of the eyelids. They look like masses of yellow opaque fat. They are not painful or tender.
Inspection is then undertaken to identify the presence of any foreign bodies on the surface of the eye. Areas of erythema should be carefully assessed. Diffuse erythema, maximal in the fornices, is a feature of conjunctivitis. Localised areas of segmental erythema may be due to episcleritis, but if it is maximal near the limbus it may be a focal keratitis. Scleritis produces a brawny red discoloration, while a deep crimson-red area is observed with subconjunctival haemorrhage. Marked erythema adjacent to the iris is known as a ciliary flush and occurs with anterior uveitis and glaucoma.
Attention is then focussed on to the cornea. Ulceration of the cornea may not be visible without fluorescein staining. Infection may extend to the anterior chamber, and a collection of pus (hypopyon) can present as a white fluid level. Loss of brightness of the cornea occurs with glaucoma due to corneal oedema.
The pupil is examined and the resting position noted. A constricted pupil may result from ciliary spasm with uveitis and it rests in a fixed, semi-dilated position with glaucoma.
Fluorescein staining should be performed and the eye is then viewed with a blue filtered light: corneal abrasions or ulcerations glow green.
General Investigations
■ Swab
Microscopy and C&S for infective organisms, e.g. stye, bacterial, viral and chlamydial conjunctivitis.
■ Rose bengal staining
To assess dead or damaged cells. It is useful in outlining a dendritic ulcer with herpes simplex infection.
■ Blood glucose
Infections are often associated with diabetes, as are xanthelasma.