Chapter 13 Diseases of the Ovary and Fallopian Tube
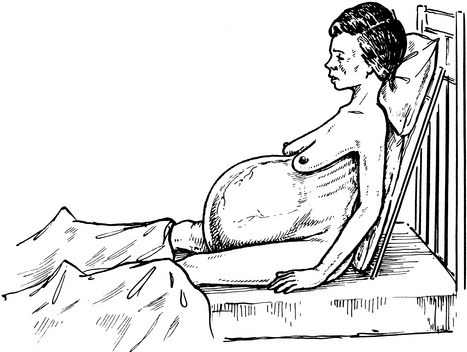
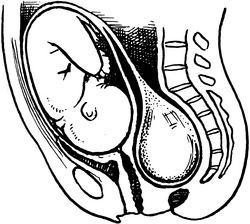
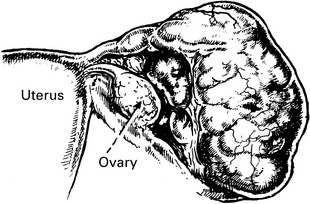
Clinical features of ovarian tumours
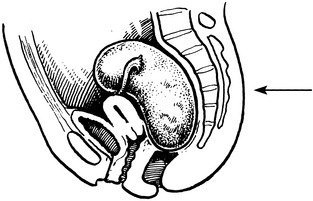
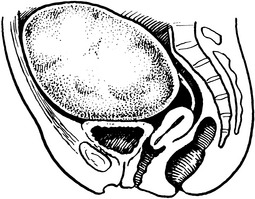
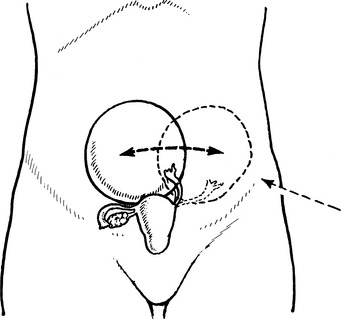
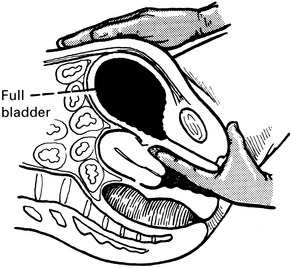
Differential diagnosis
Two very obvious mistakes must be avoided.
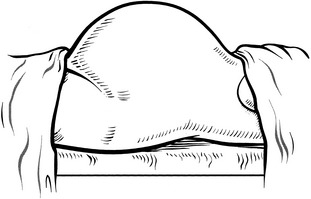
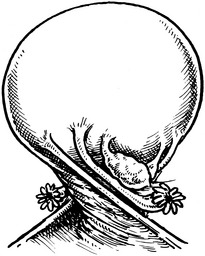
Ascites
(See ‘Shifting dullness’, page 77.)
Percussion note is dull over the top of the swelling and resonant in the flanks.
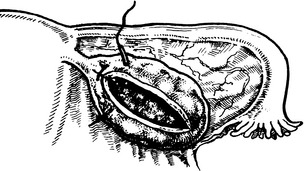
Ovarian cyst accidents
Differential diagnosis
‘Surgical conditions’ (i.e. those conditions commonly seen and dealt with by a general surgeon).
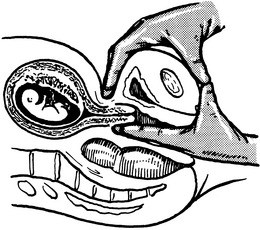
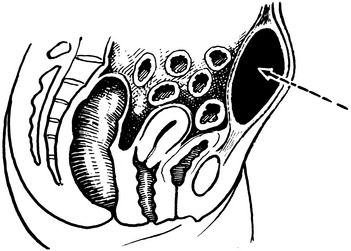
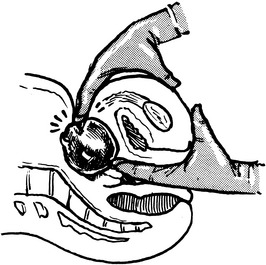
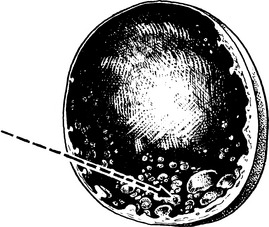
Rupture of ovarian cyst
Rupture may be either traumatic or spontaneous and may occur in the following conditions:
Benign and malignant ovarian tumours
Investigation
| Score | Menopausal status | Ultrasound |
|---|---|---|
| 1 | Premenopausal | 1 abnormality |
| 3 | Postmenopausal | 2 or > abnormality |
Risk factors for ovarian cancer
Ovarian cancer risk factors
| Increased | Decreased |
|---|---|
| Low parity | High parity |
| Infertility | Combined contraceptive pill |
| Endometriosis | Breastfeeding |
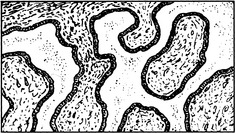
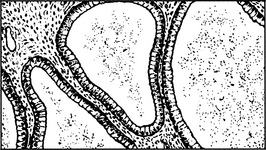
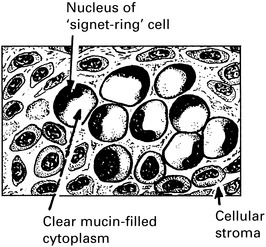
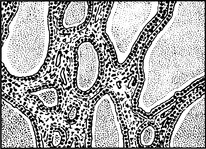
Epithelial ovarian tumours
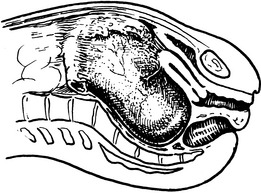
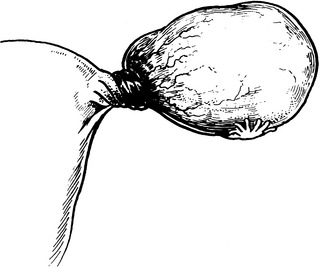
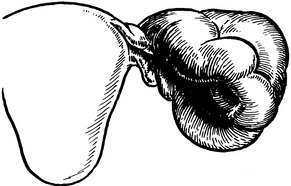
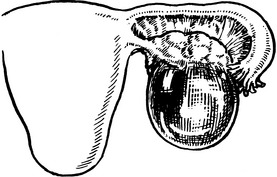
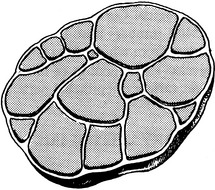
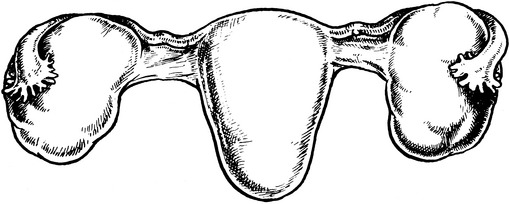
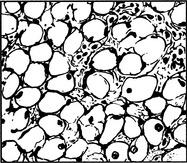
Serous cystadenoma
Germ cell ovarian tumours
| Undifferentiated | Dysgerminoma Gonadoblastoma |
| Differentiated | Embryonal Teratomas Extra-embryonal Yolk sac tumour Choriocarcinoma |
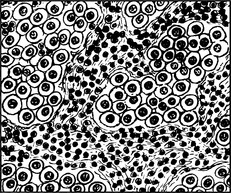
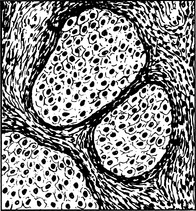
Germ cell ovarian tumours – undifferentiated
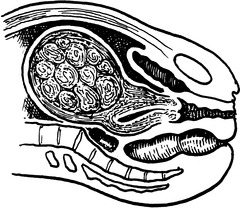
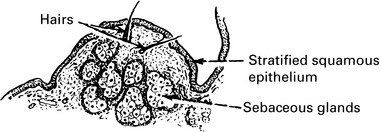
Teratomata
Hormone-producing tumours
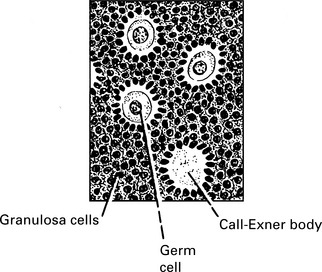
Oestrogen-producing tumours
Oestrogen excess can cause hyperplasia of:
In childhood there is accelerated skeletal growth and appearance of sex hair.
5% of these occur in children → precocious puberty.
60% occur in child-bearing years → irregular menstruation.
30% occur in postmenopausal women → postmenopausal bleeding.
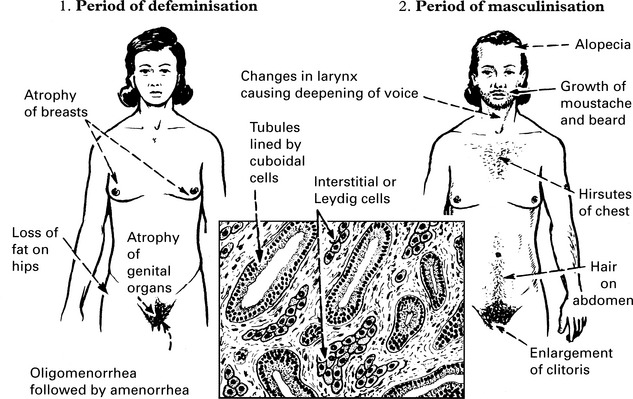
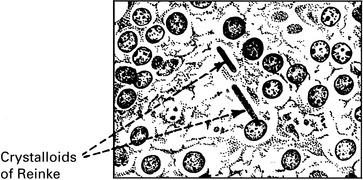
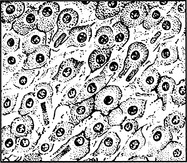
Other Hormone-Producing Tumours
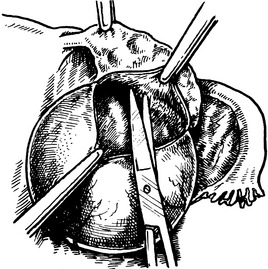
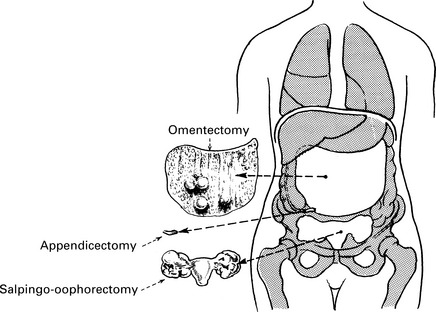
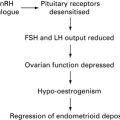
Treatment of ovarian cancer
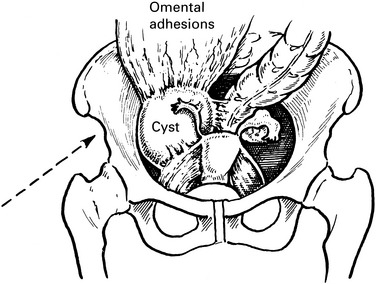
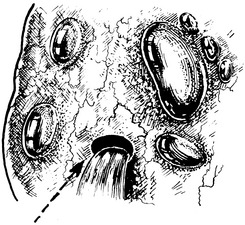
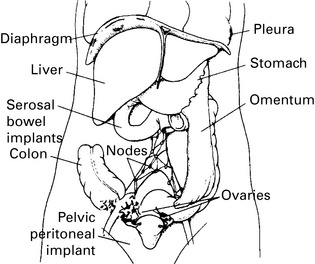
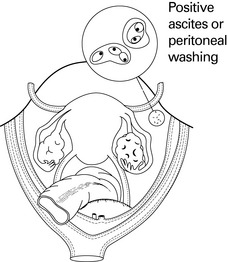
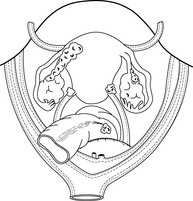
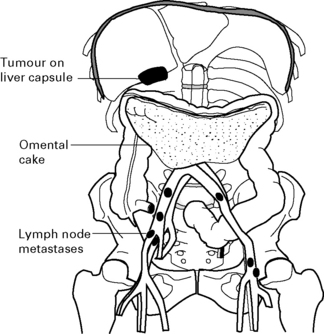
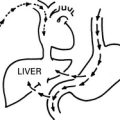
Spread of ovarian cancer
Spread directly into neighbouring structures – uterus, bladder or bowel.
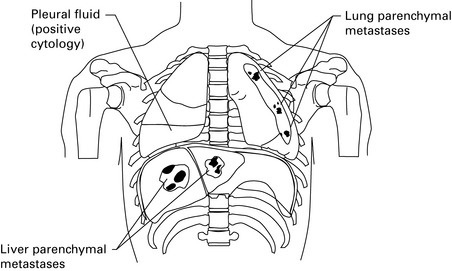
Blood spread is usually late and is to the liver and the lungs.
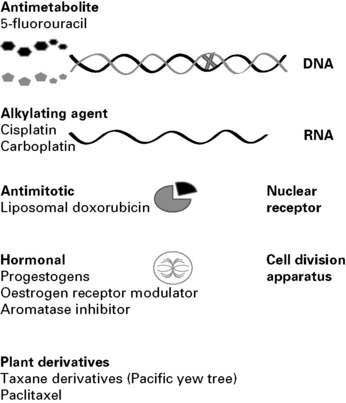
Chemotherapy is recommended for all stages of ovarian tumour greater than Stage 1B grade 2.
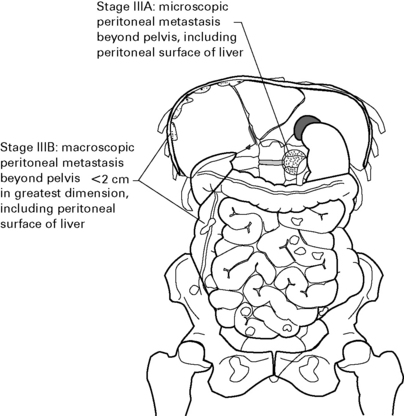
Staging of ovarian cancer
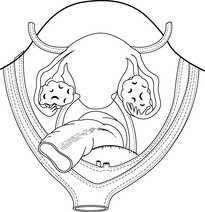
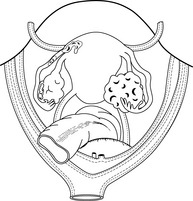
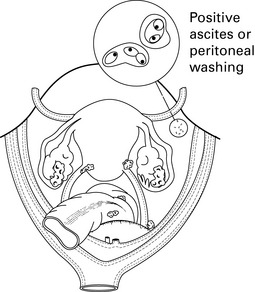
STAGE I Growth limited to ovaries.
IA. Limited to one ovary. No ascites.
IB. Limited to both ovaries. No ascites.
IIB. Spread to other pelvic tissues.
IIIC Abdominal implants >2 cm diameter or positive retroperitoneal or inguinal nodes.
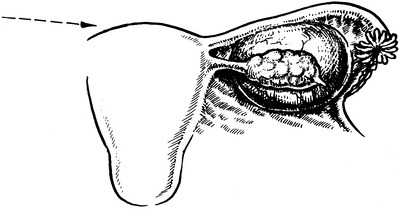
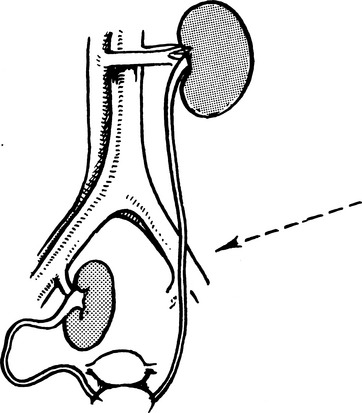
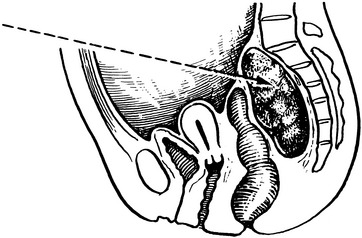
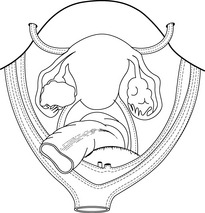
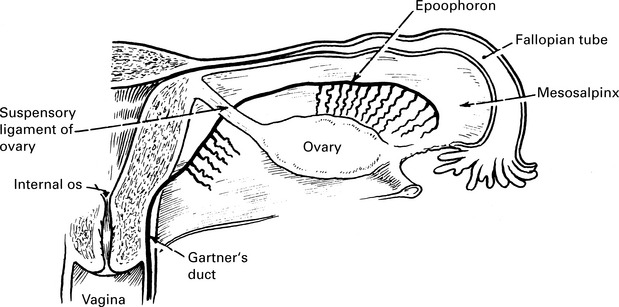
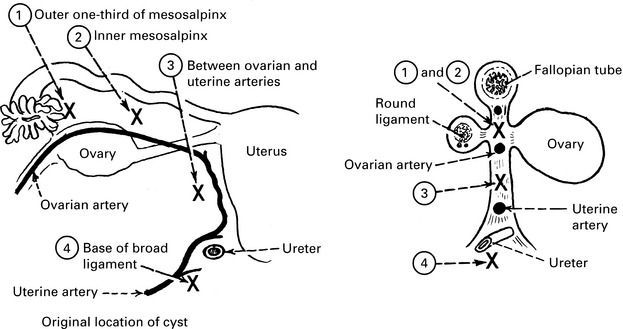
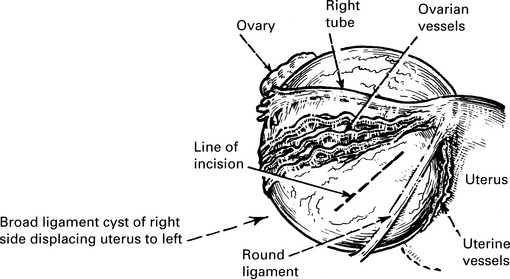
Broad ligament cysts
Carcinoma of fallopian tubes
Clinical staging
| Stage I | confined to one or both tubes |
| Stage II | pelvic extension |
| Stage III | spread to other structures (omentum, bowel, etc.), positive retroperitoneal or inguinal nodes or superficial liver metastases |
| Stage IV | distant metastases (including bladder), pleural effusion with positive cytology or parenchymal liver metastases |