Chapter 10 Diseases of the Cervix
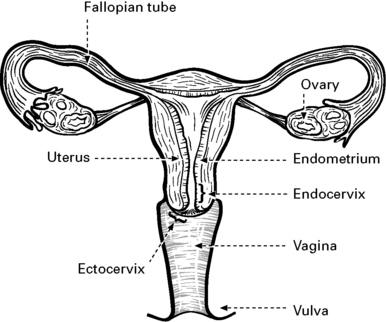
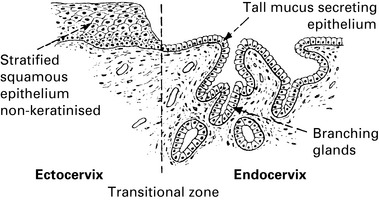
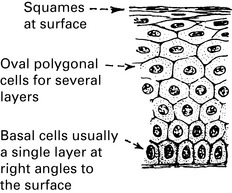
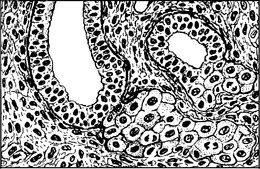
Normal cervical epithelium
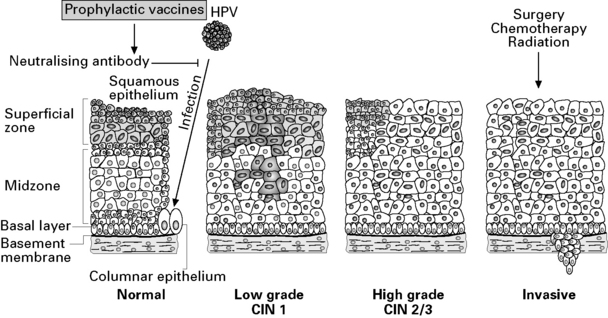
The role of human papilloma virus in cervical disease
Screening for cervical cancer
Screening process
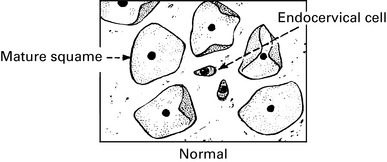
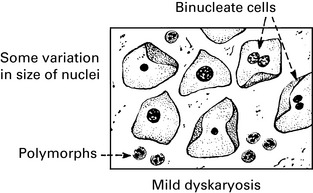
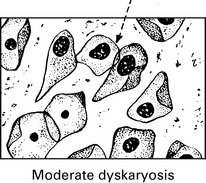
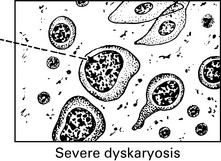
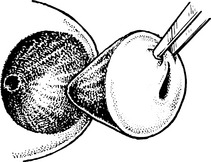
The Cervical Smear
In Scotland, the current cervical screening programme includes the following:
An abnormal smear is usually an indication for colposcopy (see p. 179).
Cervical Smears
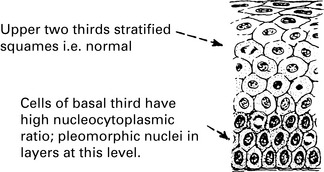
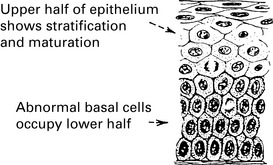
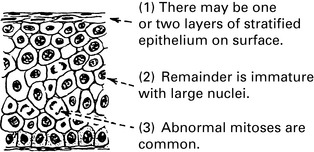
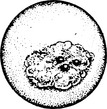
Premalignant and malignant cervical disease
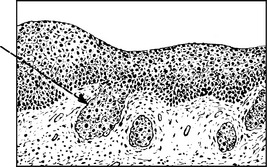
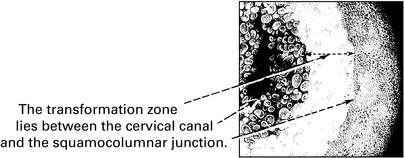
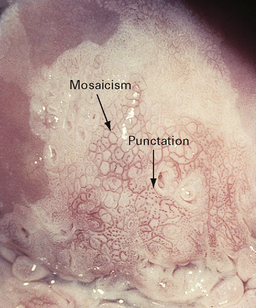
Colposcopy
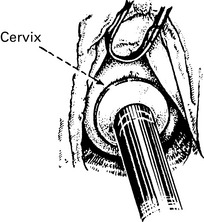
Colposcopy means binocular inspection of the cervix with magnification.
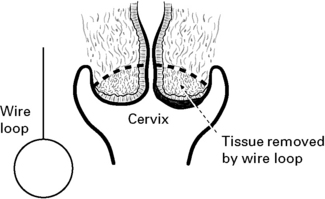
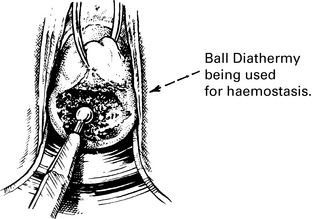
Treatment of cervical intraepithelial neoplasia
Carcinoma of the cervix
Clinical findings
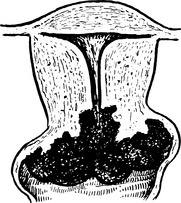
The cervix becomes very indurated; necrosis and ulceration commonly follow quickly.
Later, a large fungating mass is produced. Sloughing may leave an excavated crater.
Carcinoma of the cervix
Squamous cell carcinoma
The appearances are typical, but cell nests are absent and keratinisation is rarely seen.
The appearances in this form are typical of adenocarcinomas in other organs.
Diagnosis of cervical carcinoma
Some differential diagnoses include:
Cervicitis with ectopy, the commonest cervical lesion and, if florid, can be most misleading.
Tuberculosis is rare in the cervix. There is nearly always a history of genital tuberculosis.
Staging of cervical carcinoma
Each growth is allocated to a stage according to the extent of spread (FIGO).
Stage IA Microscopic Cervical Cancer.
Stromal invasion ≤3.0 mm in depth and ≤7.0 mm in horizontal spread.
Stromal invasion ≤5.0 mm in depth and ≤7.0 mm horizontal spread.
Stage IB The growth is confined to the cervix.
Clinically visible lesion ≤4.0 cm dimension.
Clinically visible lesion >4 cm in greatest dimension.
Stage II Tumour invades beyond the uterus but not to pelvic wall or to lower third of the vagina.
IIA Without parametrial invasion.
IIA1 Clinically visible lesion ≤4 cm greatest dimension.
IIA2 Clinically visible lesion >4 cm greatest dimension.
IIB Extension into the parametrium but not as far as the pelvic wall.
Stage III Extension to lower third of vagina or to pelvic wall.
IIIa Carcinoma involving the lower third of the vagina.
IIIb Carcinoma extending to the pelvic side wall and/or hydronephrosis due to tumour.
Stage IV Extension through vagina into bladder or outside the pelvis.
IVa Carcinoma involving adjacent organs.
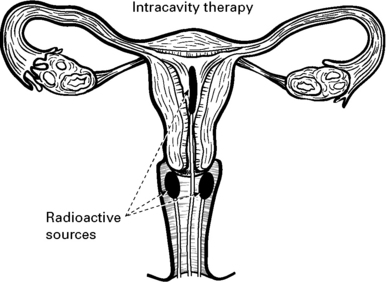
Radiotherapy and chemotherapy in cervical carcinoma
Complications
| Short term | Long term |
|---|---|
| Diarrhoea | Persistent bowel and bladder symptoms |
| Urinary frequency | Radiation menopause |
| Nausea | Vaginal stenosis/scarring/dryness |
| Vulval inflammation | Late secondary tumours |
Surgery for cervical carcinoma
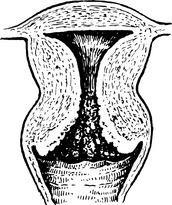
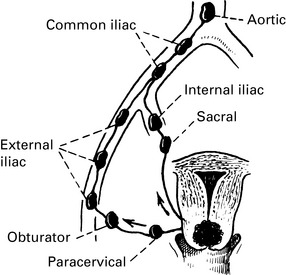
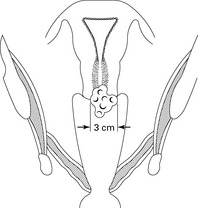
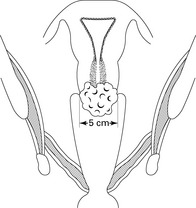
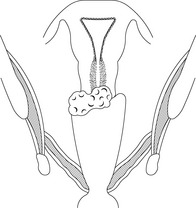
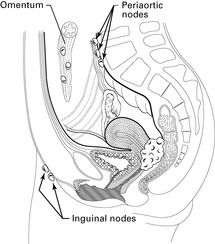
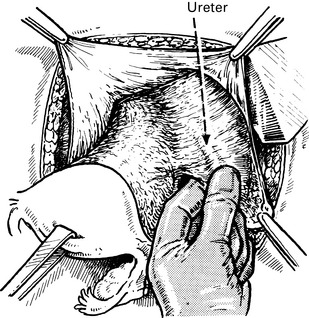
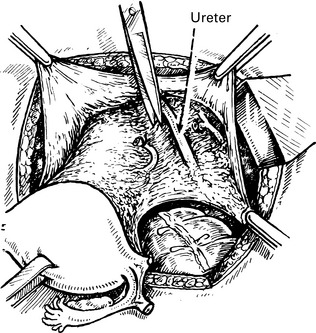
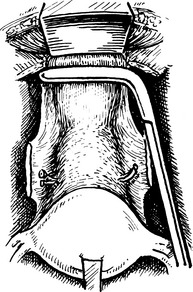
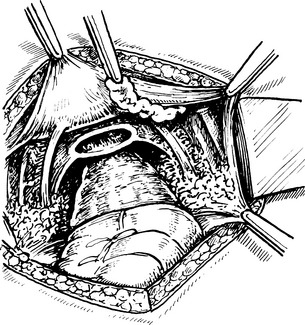
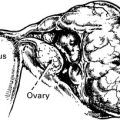
Radical hysterectomy and node dissection
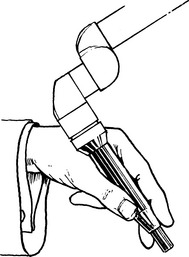
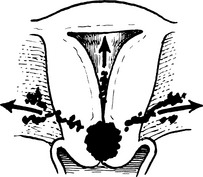
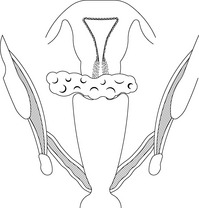
The vagina is severed below the Wertheim clamp in this example but similar clamps may also be used.
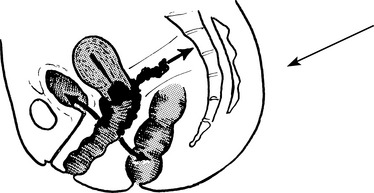
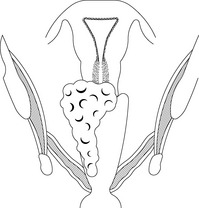
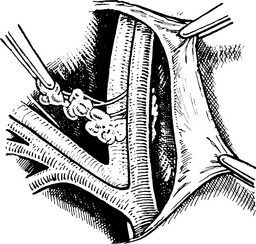
Dissecting out the fatty tissue and glands from the obturator fossa.
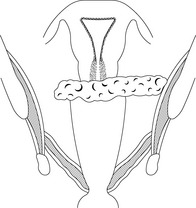
Dissecting out the external iliac glands. (Other accessible groups of nodes are also removed.)