Disaster Preparedness
Perspective
Disasters occur in all areas of the world and cause harm to people, property, infrastructures, economies, and the environment. Harm to people includes death, injury, disease, malnutrition, and psychological stress. Recent catastrophes include earthquakes in Pakistan (2005) and Haiti (2010) (Fig. 193-1); devastating tsunamis in the Indian Ocean (2004) and Japan (2011); massive hurricanes in the southern United States (2005); severe flooding in Australia (2011); tornadoes in Arkansas, Tennessee, and Kentucky (2008); and unusual weather conditions producing record snowfalls in the United States and Europe (2011). Increasing population density in floodplains and in earthquake- and hurricane-prone areas and the effects of global warming point to the probability of future catastrophic disasters with large numbers of casualties.
Given this probability and the increasing role of emergency medicine in disaster preparation, mitigation, response, and recovery, this chapter discusses disaster planning and operations with emphasis on the role of the emergency physician. The emergency physician has extensive responsibilities for community disaster preparedness and disaster medical services, including response to terrorism. In position and policy documents, the American College of Emergency Physicians outlines the scope of emergency medicine’s involvement in preparedness and response to disasters and terrorism, stating that “emergency physicians should assume a primary role in the medical aspects of disaster planning, management, and patient care” and that “emergency department personnel will become the first responders to a covert biological attack.”1,2
A committed emergency department alone is insufficient to provide hospitals with a successful disaster preparedness program. Institutional commitment by every hospital department and the administration is necessary to coordinate effectively with system-wide resources for disaster management. This is especially critical for creation of hospital surge capacity.3–5 A partial listing of general disaster medicine resources can be found in Table 193-1.
Table 193-1
List of Disaster Medicine Resources
| ORGANIZATION | WEBSITE |
| The Joint Commission | www.jointcommission.org/ |
| American College of Emergency Physicians | www.acep.org |
| Centers for Disease Control and Prevention, Emergency Preparedness and Response | www.bt.cdc.gov/training/ |
| FEMA National Preparedness Directorate, National Training and Education | http://training.fema.gov/ |
| National Response Framework | www.fema.gov/emergency/nrf/ |
| Agency for Healthcare Research and Quality | http://archive.ahrq.gov/prep/ |
| Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices | Cambridge University Press www.cambridge.org |
Surge Capacity
The concept of surge capacity has emerged as a way to manage an event that produces a sudden influx of casualties with medical and health needs that exceed current hospital resources.6 This can be due to either the volume or types of victims. The three basic components of the surge capacity system are commonly referred to as the three s‘s of staff (hospital personnel), stuff (supplies and pharmaceuticals), and structure (physical location and management infrastructure). A complete discussion of surge capacity is beyond the scope of this chapter but has been published elsewhere.7
Nature of Disasters
Classic Terminology
Some definitions have been based on the number of casualties. As previously described, the absolute number of patients is much less important than whether their medical and health needs exceed the resources to care for them at a given point in time. Another historical scheme divides disasters into three levels. Level I denotes a situation in which local resources are adequate to care for casualties. For example, the 2002 collision between a freight train and commuter train in Orange County, California, was managed effectively by local responders. Level II means that regional mutual aid is required to respond to the event. This was the case at the Hyatt Regency Hotel in Kansas City in 1981 when two skywalks collapsed, killing 114 people and injuring hundreds. Level III incidents require state and federal aid. The attack on the World Trade Center in 2001 (Fig. 193-2) and hurricane Katrina in 2005 were such events, causing such massive destruction that federal disaster medical assistance teams were deployed to New York and Louisiana, respectively, to provide medical personnel and supplies.
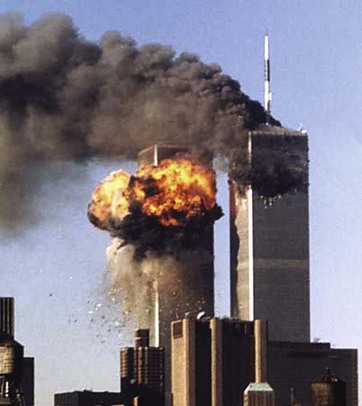
Figure 193-2 The World Trade Center attack of 2001 overwhelmed local resources and necessitated state and federal help.
One model eliminates the word disaster and replaces it with the acronym for potential injury-creating event, PICE.8–10 The PICE nomenclature is an attempt to resolve the issue regarding diverse meanings for disaster. This model is referenced in the Joint Commission standards and in publications from several countries. The PICE system is discussed here to help clarify important concepts in describing an event.
Potential Injury-Creating Event Nomenclature
The acronym PICE and its modifiers concisely describe the critical features of most types or degrees of disaster.8–10 The same occurrence can have different effects at different points in time; thus, as an event evolves over time, its description may change.
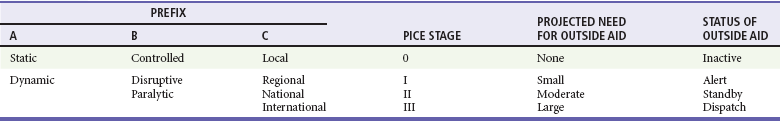
Modifiers are chosen from a standardized group of prefixes along with a stage to indicate the need for outside medical assistance (Table 193-2). The first prefix (column A) describes the potential for additional casualties. The second prefix (column B) describes whether local resources are overwhelmed and, if so, whether they must simply be augmented (disruptive) or whether they must first be totally reconstituted (paralytic). The third prefix (column C) shows the extent of geographic involvement.8–10 Column C refers strictly to the affected region and not to the location that sends assistance. Rather, the “stage” rating scale defines the likelihood that outside medical assistance will be needed either to augment or to completely reconstitute resources.8 Stage 0 means that there is little or no chance. Stage I means that there is a small chance and requires placing outside medical help on alert. Stage II means that there is a moderate chance and outside help should be placed on standby. Stage III means local resources are clearly overwhelmed and require the dispatch of outside resources and commitment of personnel. For example, a multivehicle collision with a dozen injuries and several deaths in a large city would be a stage 0, whereas in a small rural town it might be a stage III (Table 193-3).
Table 193-3
| World Trade Center attack, September 11, 2001 | Dynamic, paralytic, local, PICE stage III |
| Los Angeles civil disturbance | Dynamic, paralytic, regional, PICE stage I |
| Northridge earthquake | Dynamic, disruptive, regional, PICE stage II |
| Oklahoma City bombing | Dynamic, disruptive, local, PICE stage I |
A PICE can be either static or dynamic. Dynamic implies an evolving situation in which it is too soon after the incident to determine the numbers and types of casualties and the impact on the hospital. Alternatively, a static situation results if 10 people are injured in an incident and little potential for further harm exists.8–10
In some situations, enhancement of routine operations is not sufficient or possible. A PICE can completely overwhelm the capability to mount a normal response so that a substitute plan for recovery must be used. Situations that require significant reconstitution of critical resources are termed paralytic.8–10 Within the hospital, there are six critical elements necessary to provide a response (Box 193-1).11 If one or more of these resources are compromised, they must be reconstituted or a substitute must be implemented. Such paralytic events can be either destructive or nondestructive (Box 193-2).8
Hazard Vulnerability Analysis
After performing a hazard vulnerability analysis (www.emsa.ca.gov/disaster/files/kaiser_model.xls), emergency planners should consider the most probable events and prepare for them. There should also be planning for events that are rare but catastrophic.12 The major peacetime threat to life and limb in the United States is probably a large earthquake in a densely populated area or a terrorist attack. The disaster planner should proactively identify all such hazards and prepare contingency plans for each.
Triage
The term triage derives from the French verb trier, meaning “to sort.” The concept of triage was used as far back as Napoleon’s time to assign priorities to treatment of the injured when resources were limited. Priority is given to the most salvageable patients with the most urgent conditions. The emergency department uses triage in the hospital setting on a daily basis, but the focus of such triage is changed under disaster conditions.13,14 Standard emergency department triage is intended to identify the most seriously ill patients first and to ensure that they receive rapid care. The goal of disaster triage is slightly different, that is, “to do the most good for the most people.” In other words, there is a shift from focus on individual patients to focus on the entire affected population.15 It can be difficult for physicians to realize that to achieve the goal of maximizing benefit to an entire population of patients, they may need to let some patients die with only comfort care. Under true disaster conditions, cardiopulmonary resuscitation should not be performed.16
Routine Multiple-Casualty Triage
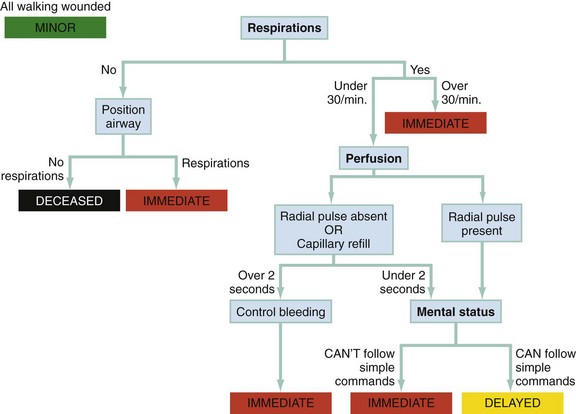
To assist in understanding of triage techniques, it is useful to consider a routine out-of-hospital event with multiple casualties (e.g., a multivehicle collision). In such situations, rescue personnel often use a Simple Triage and Rapid Treatment (START) technique that depends on a quick assessment of respiration, perfusion, and mental status.17 These three assessments can be remembered by the mnemonic RPM (respirations, perfusion, and mental status). Initially, all victims who are able to walk are asked to move away from the immediate incident area. These patients are classified as green, or “walking wounded,” and are reassessed after the more immediately critical patients are triaged.
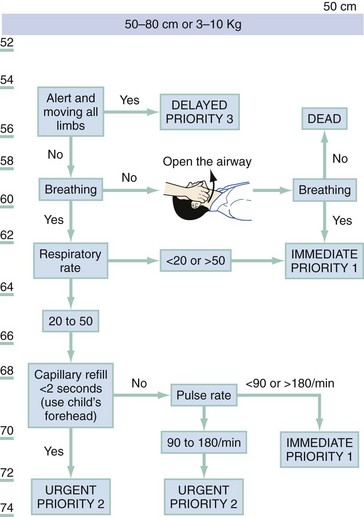
The Pediatric Triage Tape (PTT) and JumpSTART have been proposed for the triage of children. JumpSTART is a modification of the START triage protocol that includes an additional step of five rescue ventilations for children presenting apneic and modification of criteria for hypoventilation and tachypnea as well as for a decrease in mental status. The PTT uses criteria that change in proportion to increasing victim size. The parameters for a child 50 to 80 cm in length are illustrated in Figure 193-3. In a comparison of sensitivity and specificity between the PTT and JumpSTART in pediatric trauma patients, the PTT demonstrated superior outcomes.18 Both START and the PTT appear to be useful tools, but only START has been evaluated in an actual disaster situation.19–21
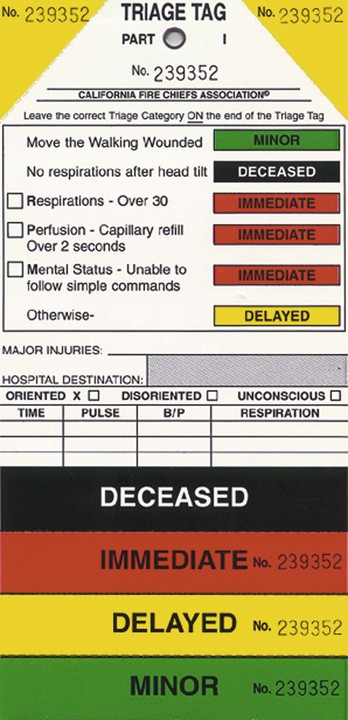
As illustrated in Figure 193-4, a rescuer can assess each patient in seconds, quickly checking respiratory rate, pulse, and ability to follow commands (mental status), and divide the patients into the remaining three categories: red (immediate), yellow (delayed), and black (deceased). The only patient care interventions provided during this process are the opening of an obstructed airway and direct pressure on obvious external hemorrhage. At this point, patients are generally transported to a hospital for definitive care. Most often, patients arrive with a color-coded triage tag and are reassessed and retriaged by the hospital staff (Fig. 193-5). An outcomes-based evaluation of the performance of START triage in an actual disaster (2002 Placentia Linda train crash) demonstrated acceptable levels of undertriage (100% sensitivity of the red category and 90% specificity of the green category).21 However, significant amounts of overtriage occurred. Use of START also appropriately prioritized the transport of victims, with patients triaged as red arriving at hospitals earlier than patients triaged as yellow or green.
Recently, a multidisciplinary group was formed to propose a potential national triage system for the United States. The result, derived by consensus of opinions, was referred to as SALT (sort, assess, lifesaving interventions, and treatment or transport).22 It differs from START mainly in the assessment of respirations (relies on a qualitative evaluation of respiratory distress rather than a number), the requirement for performance of certain emergent interventions (chest decompression), and an unstructured estimate of survivability. The algorithm is more complicated than START, and no current data exist evaluating its sensitivity, specificity, or other performance characteristics in a disaster. As such, it is not currently possible to make recommendations for its use.
Catastrophic Casualty Management
To address this situation, researchers developed the Secondary Assessment of Victim Endpoint (SAVE) system of triage.23 The SAVE triage system is designed to identify patients who are most likely to benefit from care available under austere field conditions in a resource-poor environment. When it is combined with the START protocol, SAVE triage is useful for any scenario in which multiple patients experience a prolonged delay in accessing definitive care.
The SAVE triage methodology divides patients into three categories: (1) those who will die regardless of how much care they receive, (2) those who will survive whether or not they receive care, and (3) those who will benefit significantly from austere field interventions. Only those patients expected to improve receive care beyond basic and comfort measures. With use of SAVE, patients are separated into these three categories so resources can be focused appropriately. The decision to place patients in a particular group is based on field outcome expectations derived from existing survival and morbidity statistics.23 An example is a situation in which three victims require chest tubes (two victims require one tube each and one victim requires two tubes), but only two chest tubes are available. The SAVE principles guide providers to place their last two chest tubes into the two victims who need it rather than into the single victim requiring two tubes.
Since nuclear, biologic, and chemical terrorism has become a threat, new triage systems are under development.13,24 These systems attempt to incorporate the added threats from exposure and contamination into the triage process. One such method for biologic casualties triages many individuals to home observation rather than hospitalization to optimize resource use and to minimize the spread of the infectious agent.24 In addition, responders must be protected from secondary contamination or exposure; therefore, part of the triage algorithm should include a risk assessment and determination of whether and what type of personal protective equipment should be donned before patients are assessed. A quick determination is critical to prevent patient deaths from traumatic injuries while awaiting medical care from responders concerned about their own health and safety. This is particularly true in a “combined event” scenario, such as an event involving a radiologic dispersion device. Also associated with terrorism incidents are large numbers of psychogenic casualties, those who believe they were exposed but actually were not and those at risk for post-traumatic stress disorder. The emergency plan should include a mechanism to assess and to sort these individuals so as not to overwhelm the emergency department and also provide mental health care. While performing triage, the emergency physician should also consider the effects of extremes of age, underlying disease, and multiple injuries when assessing the potential prognosis for a given patient. Fortunately, the treatment of many nontraumatic emergencies can be accomplished with field interventions that do not consume extensive resources. Therefore, patients with such illnesses should usually be triaged to the treatment area.
Care of Special Needs Populations
Within the general population, groups of unique individuals exist that are at greater risk for injury, death, and property loss resulting from a disaster. These vulnerable populations include children, the elderly, racial and ethnic minorities, the disabled, those residing in institutions such as skilled nursing facilities, and the mentally ill. Challenges in the management of these populations with special needs during a disaster include lack of mobility, tracking of victim movement during evacuations and issues of reunification with responsible family members, inability to understand English or to comprehend instructions issued by local authorities, and poor access to transportation resources. A detailed discussion on the disaster management of these populations is beyond the scope of this chapter but available elsewhere.25,26 Those responsible for disaster planning should ensure that policies and procedure are developed that address the unique needs of such groups.
Out-of-Hospital Response
Emergency Medical Services System Protocols
Physicians working at hospitals should be familiar with community disaster management operations, including the function of the emergency operations center.11 Mutual aid agreements with other hospitals or regions should be considered for situations in which current hospital capacity is exceeded or evacuation is necessary.
Incident Command System
Some form of an incident management system is now a standard component of emergency command and control throughout the United States. It provides a flexible management structure on which to organize a response.27 The federal version, known as the National Incident Management System, is incorporated into the National Response Framework and provides strategic guidance on the U.S. government’s involvement in disaster response. All states must use an incident management system, and it must be compliant with the National Incident Management System.28 By standardizing an organizational structure and using common terminology, an incident command system provides a management configuration that is adaptable to events involving a multiagency or multijurisdictional response. At the most basic level, there are five functional elements in the organizational structure: incident command, operations, planning, logistics, and finance. The principles of an incident command system can also be applied to the hospital setting through implementation of a Hospital Incident Command System. With this type of organizational infrastructure and the flexibility to expand and to collapse functions as needed, an orderly and efficient response to any incident can be accomplished. Because hospitals cannot anticipate every contingency, a system such as the Hospital Incident Command System assists with planned improvisation. The Joint Commission (formerly known as the Joint Commission on Accreditation of Healthcare Organizations) standards require use of an incident management system in health care facilities.
Incident Command
The incident commander has overall management responsibility for the incident. Physicians should understand that they are not in charge at the scene of an out-of-hospital incident.28 In general, nonhospital providers can manage the scene, and physicians should remain at the hospital to provide definitive care. When a physician is on scene, the best way to assist is to ask the incident commander where medical help is most needed.
The incident commander may choose to appoint a command staff to manage public information, safety, and interagency liaisons.27 When an event involves multiple jurisdictions, a unified command is established that coordinates a common and consistent action plan to make the best use of available resources.
Operations Section
The operations section has a chief who is responsible for the management of all incident tactical activities.27 This section can be expanded and subdivided into branches (e.g., law, fire, and medical) and divisions. Operations also manages the resources assigned to staging areas. Ambulances, personnel, and supplies should be staged outside the perimeter of the scene and directed in as needed rather than converging on the disaster site, potentially disrupting activities and blocking the exodus of patients. It is under the operations section that all medical triage and care is provided.
Planning Section
The planning section collects, evaluates, and disseminates information about incident operations and the status of resources. This section also develops incident action plans and conducts planning meetings.27
Planning and Hospital Response
Comprehensive Emergency Management
The comprehensive emergency management all-hazard approach to disaster preparedness has been a Joint Commission requirement since January 2001. Comprehensive emergency management consists of four phases: mitigation, preparedness, response, and recovery.29,30 Mitigation involves taking actions to reduce the impact of identified hazards. Training, drills, and cataloging of resources are examples of preparedness activities. Response includes assessment of the situation and coordination of resources. Finally, recovery consists of a return to normal operations and debriefing to critique the response and to provide long-term psychological support to the victims and rescuers.
As required by the Joint Commission, a hospital’s disaster or “emergency management” plan must address events that occur both inside (internal) and outside (external) the institution.30 Because some incidents affect both internal and external operations, a hospital emergency management program should contain plans that address all circumstances.
Hospital Disaster Response Plan
A disaster event can disrupt daily, routine hospital functions. This can represent an infrastructure failure (e.g., loss of electric power and water) or a threat to the safety of patients and hospital personnel (e.g., labor dispute or approaching hurricane). Because the response varies from postponement of elective surgery to facility evacuation, every hospital department must participate in the planning process. At a minimum, the disaster plan should clearly delineate the circumstances in which the plan is activated; identify the command structure with defined lines of authority and responsibility; describe a response strategy for each anticipated incident; estimate an incident’s impact on safety and hospital function, providing for evacuation if necessary; and list essential information, such as critical telephone numbers (e.g., elevators, key personnel, and pay telephones), community agencies (emergency medical services, police, and public health), and sources of vital supplies (water, oxygen, and drugs).29
In the unlikely event that evacuation of the emergency department is necessary, evacuation routes and relocation destinations that have been planned in advance maximize safety and efficiency. When resources are plentiful, emergency department patients in critical condition are assigned the highest priority for evacuation and transport. Less ill patients receive a lower priority.31 When resources are limited (e.g., in the event of a large-magnitude earthquake), the reverse strategy applies. The least critically ill patients receive the highest priority for evacuation.
Another scenario would be an event occurring in the community that results in a sudden influx of patients requiring emergency care at hospitals. This type of incident has no direct impact on hospital capacity or function. However, the need to rapidly increase surge capacity may require implementation of different patient management strategies (i.e., temporary creation of alternate care sites on hospital grounds). Participation in the planning and execution of the hospital disaster response is an important administrative responsibility.16 Available data guiding development of disaster strategies are incomplete, but an effective disaster response can be created by reviewing the essential components of disaster plans and the previous experience of hospitals.16,29,31,32 A member of the emergency department must have a leadership role in the planning and implementation of the disaster plans.
Basic Components of a Hospital Comprehensive Disaster Response Planning Process
Interdepartmental Planning Group
The interdepartmental planning group has the responsibility for hazard identification and disaster preparedness activities. The process of conducting a hazard vulnerability analysis is complex, but templates such as the one created by the Kaiser Foundation Health Plan may be informative.33 Frequently referred to as the disaster or emergency preparedness committee, it is composed of representatives from all departments vital to the hospital’s response, including administration, medical staff, nursing, safety, security, emergency department, and engineering. Additional input may occasionally be necessary from outside agencies (e.g., fire department, hospital suppliers of goods and services, and emergency medical services agency).
The committee should be structured to ensure that the plan is properly constructed, tested, and executed. Hospital resources must be provided to support the planning process and testing of the plan, and there must be a detailed educational program for all affected hospital staff.30,34
Resource Management
A full inventory of the hospital’s resources is necessary. In addition to equipment, space, and personnel within the institution, potential support from outside the hospital must be sought. It is also necessary to develop contingency plans to compensate for lost resources (e.g., failure of hospital computers during a power outage or cyber attack). Augmentation of such resources is critical to the successful increase of the hospital’s surge capacity.4,5,35
Strong relationships with community agencies (e.g., fire department and regional emergency medical services system) are important to ensure a coordinated disaster response. Hospitals located near companies using large amounts of hazardous materials are required by Title III of the Superfund Amendments and Reauthorization Act to participate in local emergency planning committees, sometimes termed LEPCs.36
Media
The media can be an important source of information but can also significantly disrupt the hospital’s disaster response. Therefore, arrangements should be made in advance for a designated individual to coordinate all media interactions and for these briefings to occur in a designated location. Media coordinators should inform reporters of the time they will receive their next update so they do not intrude on response operations while trying to obtain information. A strong media liaison can facilitate dissemination of important information to the public, such as that no blood shortage exists so that individuals refrain from coming to the hospital to donate blood. In fact, crisis and emergency health risk communication is now an important part of managing the disaster response and can have a significant impact on the public’s perception of events.37 Individuals designated the media coordinator should be familiar with the basic principles of emergency health risk communication. Security should be involved in managing the media response to the hospital and in preventing media from interfering with triage and treatment of patients.
Communication
Communication systems are probably the most important but also most vulnerable component of a disaster plan.16,31 Redundant systems are essential. Those responsible for mobilizing the emergency response require access to at least one other communication system besides the telephone (which is frequently one of the first systems compromised during a disaster). Two-way radios are often used, as are pay telephones, independent fax lines, and cellular phones. Another option is the use of satellite phones and wireless hand-held devices to transmit e-mail messages. Recent advances in communication technology exemplified by Facebook and Twitter show promise. Survivors of the 2011 Japan earthquake used these techniques to provide early information to the outside world on conditions within the disaster zone.38 Runners are also useful for intrahospital communication if all else fails.
Personnel
The disaster plan must include a roster of all critical positions and personnel and establish a reliable method for their mobilization. Several individuals should be assigned to each position in case some personnel cannot be reached. A protocol for managing volunteers is also crucial. A large group of uncontrolled volunteers descending on a hospital (“convergent volunteerism”) can be as disruptive as the disaster.39
Credentialing of volunteer health professionals in a timely manner so hospitals can use their services during a disaster remains a challenge. A federally supported program known as the Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP) is attempting to address this problem. It will provide a system for credentialing of volunteer health care providers in advance of a disaster so they will have emergency privileges should the need for their services arise.40 There remain significant challenges with such a system, including whether sufficient numbers of providers will participate, how fast they can deploy, how well qualified they will be, and whether they will have competing obligations during a disaster. An alternative system that permits hospitals to recognize each other’s credentialing process through a shared database shows promise. Not only will this alternative system facilitate participation by most health care providers, but it also permits hospitals to grant emergency privileges within minutes after a disaster.40
Training Exercises
Disaster exercises are one of the more effective ways of familiarizing hospital staff with their responsibilities. All hospital departments should participate, and community agencies should be involved. The Joint Commission requires two drills a year; these should mimic incidents that are likely to occur. Methods to assess the effectiveness of these exercises as measures of overall hospital disaster preparedness are improving.41
Review of Hospital and Community Disaster Response Experience
Catastrophic Disasters
In a large-scale disaster, paramedics may be unavailable to assist in patient transfers or hospital evacuations. Disaster medical assistance teams and urban search and rescue teams will deploy, but their time to arrival on scene may be variable. Each individual hospital may have to remain self-sufficient for 48 to 72 hours or longer.42 Generator problems are frequent; they either fail altogether (as they did during the Loma Prieta earthquake) or supply insufficient power to meet emergency needs (as during the Northridge earthquake). Evacuation plans must not require elevators for this reason. Telephone service will cease as lines are disrupted or deliberately restricted by the phone company. Cellular phones may function within a local area, but failure is likely if more distant sites within the city are dialed. Hospital radios designated for disaster use should have the hardware secured to prevent earthquake damage.
After earthquakes or explosions, immediate access to structural engineers is important. In the Northridge earthquake, eight hospitals in the Los Angeles area sustained enough damage to force evacuation of at least one patient. Four institutions completely evacuated their facilities in the first 24 hours, including two hospitals that met the most current structural earthquake standards. Further structural damage was subsequently identified, and two additional hospitals were forced to evacuate completely in the next 2 weeks. Ultimately, four of these hospitals were permanently closed and demolished.31
Hospitals are also vulnerable to hurricanes. In a study of hurricane Rita’s (2005) impact on regional hospitals in Texas and Louisiana, seven hospitals were forced to evacuate patients.32 Significant problems included prolonged loss of power, potable water, and staff. It was also difficult to obtain vehicles for transportation of patients to other facilities. Nonmedical vehicles were sometimes used to evacuate stable patients.
Need for Local Response
Currently, it is not possible for outside assistance to arrive in force during the crucial first 48 hours after the event. Therefore, an alternative source of immediate, sophisticated medical care is necessary. It appears this is best provided by local responders who can begin caring for patients soon after the event.43 The Medical Disaster Response Project is the most advanced model of a local medical response to such a disaster. Developed by emergency physicians in southern California, the Medical Disaster Response Project has two components: (1) training of health care providers in the management of disaster victims under austere conditions and (2) placement of sophisticated medical supplies at designated sites within the community.42 Under this plan, victims could receive rapid, advanced medical care from surviving volunteer health care providers even if hospitals were destroyed. The current Strategic National Stockpile is modeled after components of this plan. In addition, it was used as a major source document for the development of the Medical Reserve Corps.
Toxic Disasters (Hazardous Material)
Hospitals in the vicinity of major chemical industries, transportation corridors, or probable terrorist targets (e.g., major theme parks or nationally symbolic buildings) should be aware of potential hazards from incidents involving chemical and radioactive substances and be prepared to decontaminate large numbers of individuals exposed to these hazardous substances. Effective decontamination of victims and the need for safety measures on the part of rescue personnel to prevent secondary contamination are critical.44 Decontamination equipment should be stored near the emergency department, and the staff must be trained in its use. This location must be known to personnel.45 When such an emergency occurs, there is little time to search the hospital for the necessary supplies.
Ideally, patients contaminated with hazardous chemicals should first be brought to a designated decontamination area containing a warm-water shower with a container to hold drainage water. Victims should remove all clothing. Clothing and valuables are bagged, tagged, and stored. Contaminated patients must never be brought into regular patient care areas because of the danger of contaminating other patients, hospital staff, and equipment. In 1994, paramedics unsuspectingly transported a patient contaminated with a degradation product of dimethyl sulfoxide to an emergency department in Riverside, California. Before the presence of the hazardous material was detected, six health care workers were exposed, including an emergency physician. The emergency physician experienced a near-fatal exposure and required intubation and an extensive stay in the hospital’s intensive care unit. Uncontrolled spread of the toxin resulted in evacuation and temporary closure of the emergency department.46
Chemical, Biologic, Radiologic, Nuclear, and Explosive Terrorism
In addition to the familiar threat from hazardous materials, there is another challenge: a potential attack by terrorists using biologic, radiologic, or chemical weapons (see Chapter 194). Although somewhat similar to hazardous materials situations, management of patients exposed to weapons of mass destruction (WMD) requires additional knowledge and skills. Expertise in the management of patients attacked with unconventional weapons is important, but emergency physicians should also be familiar with treatment of blast injuries. High-explosive events, including suicide bombers, remain the most probable type of terrorism.
Unlike radiologic or biologic weapons, chemical agents produce symptoms quickly. The challenge is decontamination and treatment. Approximately 80% of mass casualty decontaminations are performed at hospitals. Therefore, hospitals must be prepared to decontaminate patients outside the emergency department. Personal protective equipment is also essential for responders and hospital “first receivers” because of the risk of exposure during the decontamination process.45,46
Disaster Stress Management
If a critical incident has profoundly affected participants and if symptoms are still present many hours later, urgent assistance is provided in the form of defusing. The critical incident defusing process is coordinated by mental health and peer support staff and focuses on information and venting of emotions. This process often takes place away from public view to protect confidentiality. If the psychological stress is severe, the process transitions to formal care provided by psychiatrists or psychologists.47 Data from previous experiences suggest that such intervention can assist providers in maintaining job performance and satisfaction.
In addition to disaster health care providers, the victims themselves can suffer significant psychological trauma. Rapid identification of such individuals is a priority and can be facilitated by use of a recently developed psychological triage algorithm known as PsySTART. The tool itself has been previously validated and, in a recent trial, appears to assist health care workers in rapidly identifying patients who may benefit from acute psychological intervention.48
Disaster Management and Response Organizations Within the U.S. Government
Urban Search and Rescue (ESF #9 of the National Response Framework)
When a building collapses because of an earthquake, terrorist bombing, structural failure, or other reason, various challenges confront rescue and medical personnel.49 Some victims require field amputations to facilitate extrication,49 and use of urban search and rescue teams and effective emergency medical care may improve the outcomes of such lifesaving efforts. This national system of multidisciplinary task forces is designed for rapid deployment to the sites of collapsed structures.50 The medical team’s responsibilities include caring for task force members, victims recovered by search and rescue activities, and the search team’s dogs. There are also WMD urban search and rescue teams trained by FEMA to respond to nuclear, biologic, and chemical terrorist attacks.
Metropolitan Medical Response System
Metropolitan Medical Strike Teams (MMSTs) are highly trained, readily deployable, and fully equipped groups of medical, fire, and rescue professionals. As a component of the larger Metropolitan Medical Response System (MMRS), they support other local personnel in treating the victims of a chemical, biologic, or nuclear attack. In 2008 the MMRS expanded to include 124 participating jurisdictions. Although composed of local personnel, MMSTs are under the direction of the DHS. Their goal is to enhance local planning and response capability. However, hospital and community planners must still create an independent response because MMSTs require 90 minutes or longer to deploy.51 MMSTs are equipped with chemical agent monitoring devices, protective equipment, and pharmaceutical supplies.
Department of Veterans Affairs
The VA has not traditionally been regarded as a disaster response entity. However, one of the VA’s four legally mandated missions is emergency management. A unique feature of the VA is that its facilities and personnel are situated nationwide, and these are used to support federal health and medical assistance to state and local governments during disasters. The VA has highly trained specialty personnel who can support disaster medical activities. In addition to the vast pool of human resources, the VA provides large amounts of the pharmaceuticals and expendable supplies for on-site disaster support. For example, the VA purchases the contents of the CDC’s Strategic National Stockpile. VA support is coordinated through the DHS and DHHS, as the lead federal agency for health and medical response. In addition to the VA’s role in the federal response to disasters, as the largest integrated health care system in the nation, it has a well-developed hospital emergency management program. The VA Emergency Management Program Guidebook is an open-source reference that provides up-to-date information on emergency management concepts and various templates for emergency operations plans and hazard vulnerability assessment tools for hospitals.52
Future Directions
The field of disaster medicine has become a major subspecialty within emergency medicine, and standing committees and membership sections for disaster medicine are now organized within the American College of Emergency Physicians and the Society for Academic Emergency Medicine. There are also numerous national and international forums for the presentation of disaster medical research results. Since the American College of Emergency Physicians first defined a disaster medicine curriculum suitable for residencies and fellowships, a number of disaster medicine fellowships have been established in the United States and elsewhere.53 Disaster medicine textbooks and journals are increasing. In the 21st century, disaster medicine will continue to develop as a professional activity and unique academic specialty.
References
1. Waeckerle, JF, et al. Executive summary: Developing objectives, content, and competencies for the training of emergency medical technicians, emergency physicians, and emergency nurses to care for casualties resulting from nuclear, biological, or chemical (NBC) incidents. Ann Emerg Med. 2001;37:587.
2. American College of Emergency Physicians. Clinical Policies: Disaster Medical Services. www.acep.org/disaster, October 2006.
3. Kaji, AH, Koenig, KL, Lewis, RJ. Current hospital disaster preparedness. JAMA. 2007;298:2188.
4. Kaji, A, Koenig, KL, Bey, T. Surge capacity for healthcare systems: A conceptual framework. Acad Emerg Med. 2006;13:1157.
5. Barbisch, D, Koenig, KL. Understanding surge capacity: Essential elements. Acad Emerg Med. 2006;13:1098.
6. California Department of Public Health. Standards and Guidelines for Healthcare Surge During Emergencies. www.bepreparedcalifornia.ca.gov.
7. Barbisch, D, Haik, J, Tessone, A, Hanfling, D. Surge capacity. In: Koenig KL, Schultz CH, eds. Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press, 2010.
8. Koenig, KL, Dinerman, N, Kuehl, AE. Disaster nomenclature: A functional impact approach: The PICE system. Acad Emerg Med. 1996;3:723.
9. Nocera, A. Australian major incident nomenclature: It may be a “disaster” but in an “emergency” it is just a mess. Aust N Z J Surg. 2001;71:162.
10. Burkle, FM. Integrating international responses to complex emergencies, unconventional war, and terrorism. Crit Care Med. 2005;33:S7.
11. Auf der Heide, E, Resource management, Disaster Response: Principles of Preparation and Coordination. Mosby: St. Louis, 1989. http://orgmail2.coe-dmha.org/dr/DisasterResponse.nsf/section/31219255A624812F0A25691A00671909?opendocument&home=flash.
12. Department of Health and Human Services. Medical Surge Capacity and Capability: A Management System for Integrating Medical and Health Resources During Large Scale Emergencies. Washington, DC: Department of Health and Human Services; 2004.
13. Cone, DC, Koenig, KL. Mass casualty triage in the chemical, biological, radiological, or nuclear environment. Eur J Emerg Med. 2003;12:287.
14. Garner, A, Lee, A, Harrison, K, Schultz, CH. Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med. 2001;38:541.
15. Kahn, CA, Lerner, EB, Cone, DC. Triage. In: Koenig KL, Schultz CH, eds. Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press, 2010.
16. Waeckerle, JF. Disaster planning and response. N Engl J Med. 1991;324:815.
17. Critical Illness and Trauma Foundation, START: Simple Triage and Rapid Treatment. Newport Beach, Calif:Critical Illness and Trauma Foundation, Newport Beach Fire Department; 2001. www.citmt.org/start/default.htm.
18. Wallis, LA, Carley, S. Comparison of pediatric major incident primary triage tools. Emerg Med J. 2006;23:475–478.
19. Romig, LE. The JumpSTART Pediatric MCI Triage Tool. www.jumpstarttriage.com.
20. Sanddal, TL, Loyacono, T, Sanddal, ND. Effect of JumpSTART training on immediate and short-term pediatric triage. Pediatr Emerg Care. 2004;20:749.
21. Kahn, CA, Schultz, CH, Miller, KT, Anderson, CL. Does START triage work? An outcomes assessment after a disaster. Ann Emerg Med. 2009;54:424–430.
22. Lerner, EB, et al. Mass casualty triage: An evaluation of the data and development of a proposed national guideline. Disaster Med Public Health Prep. 2008;2(Suppl 1):S25–S34.
23. Benson, M, Koenig, KL, Schultz, CH. Disaster triage: START then SAVE—a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11:117.
24. Burkle, FM. Population-based triage management in response to surge-capacity requirements during a large-scale bioevent disaster. Acad Emerg Med. 2006;13:1118.
25. Phillips, BD. Special needs populations. In: Koenig KL, Schultz CH, eds. Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press, 2010.
26. National Commission on Children and Disasters. 2010 Report to the President and Congress. Rockville, Md: Agency for Healthcare Research and Quality; October 2010.
27. Emergency Management Institute, IS-100.b: Introduction to Incident Command System, ICS-100. Emmitsburg, Md:Emergency Management Institute, Federal Emergency Management Agency; 2010. http://training.fema.gov/EMIWeb/IS/IS100b.asp.
28. U.S. Department of Homeland Security, National Response Framework. Washington, DC:Department of Homeland Security; 2008. www.fema.gov/pdf/emergency/nrf/nrf-core.pdf.
29. Schultz, CH, Mothershead, JL, Field, M. Bioterrorism preparedness I: The emergency department and hospital. Emerg Med Clin North Am. 2002;20:437.
30. Joint Commission. Comprehensive Accreditation Manual for Hospitals. Oak Brook Terrace, Ill: Joint Commission; 2007.
31. Schultz, CH, Koenig, KL, Lewis, RJ. Implications of hospital evacuation after the Northridge, California, earthquake. N Engl J Med. 2003;348:1349.
32. Andress, K, Downey, E, Schultz, CH. Implications of hospital evacuation after hurricane Rita [abstract]. Acad Emerg Med. 2007;14(Suppl 1):S190.
33. Hoyle, JD. Healthcare facility disaster management. In: Koenig KL, Schultz CH, eds. Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press, 2010.
34. California Emergency Medical Services Authority, Hospital Incident Command System. Sacramento, Calif:Emergency Medical Services Authority; 2006. www.emsa.ca.gov/hics.
35. Schultz, CH, Koenig, KL. State of research in high-consequence hospital surge capacity. Acad Emerg Med. 2006;13:1153.
36. Superfund Amendments and Reauthorization Act of 1986 (SARA), Title III, Section 305(a), Emergency Training; Homeland Security Act of 2002, Codified in 6 U.S. Code, Public Law 107-296. www.fema.gov/government/grant/sara.shtm.
37. Reynolds, BS, Shenhar, G. Crisis and emergency risk communication. In: Koenig KL, Schultz CH, eds. Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press, 2010.
38. Keim, ME, Noji, E. Emergent use of social media: A new age of opportunity for disaster resilience. Am J Disaster Med. 2011;6:47–54.
39. Cone, DC, Weir, SD, Bogucki, S. Convergent volunteerism. Ann Emerg Med. 2003;41:457.
40. Schultz, CH, Stratton, SJ. Improving hospital surge capacity: A new concept for emergency credentialing of volunteers. Ann Emerg Med. 2007;49:602.
41. Kaji, AH, Langford, V, Lewis, RJ. Assessing hospital disaster preparedness: A comparison of an on-site survey, directly observed drill performance, and video analysis of teamwork. Ann Emerg Med. 2008;52:195–201.
42. Schultz, CH, Koenig, KL, Noji, EK. A medical disaster response to reduce immediate mortality following an earthquake. N Engl J Med. 1996;334:438.
43. Kazzi, AA, et al. Earthquake epidemiology: The 1994 Los Angeles earthquake emergency department experience at a community hospital. Prehosp Disaster Med. 2000;15:12.
44. Koenig, KL, et al. Healthcare facility–based decontamination of victims exposed to chemical, biological, and radiological material. Am J Emerg Med. 2008;26:71.
45. Koenig, KL, et al. Health care facilities’ “war on terrorism”: A deliberate process for recommending personal protective equipment. Am J Emerg Med. 2007;25:185.
46. Koenig, KL. Strip and shower: The duck and cover for the 21st century. Ann Emerg Med. 2003;42:391.
47. Oster, NS, Doyle, CJ. Critical incident stress. In: Hogan DE, Burstein JL, eds. Disaster Medicine. Philadelphia: Lippincott Williams & Wilkins; 2007:30–37.
48. Schreiber, M, et al. PsySTART Rapid Disaster Mental Health Triage System: Performance during a full scale terrorism exercise in Los Angeles County hospitals [abstract]. Acad Emerg Med. 2011;18:S26.
49. Schultz, CH, Koenig, KL. Preventing crush syndrome: Assisting with field amputation and fasciotomy. J Emerg Med Services. 1997;22:30.
50. Better, OS, Stein, JH. Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. N Engl J Med. 1990;322:825.
51. Institute of Medicine and National Research Council. Chemical and Biological Terrorism: Research and Development to Improve Civilian Medical Response. Washington, DC: National Academy Press; 1999.
52. U.S. Department of Veterans Affairs, Emergency Management Strategic Health Care Group. 2008 Emergency Management Program Guidebook. www1.va.gov/emshg/page.cfm?pg=114.
53. European Master in Disaster Medicine. http://www.dismedmaster.com.