Digestive System
Functions of the Digestive System
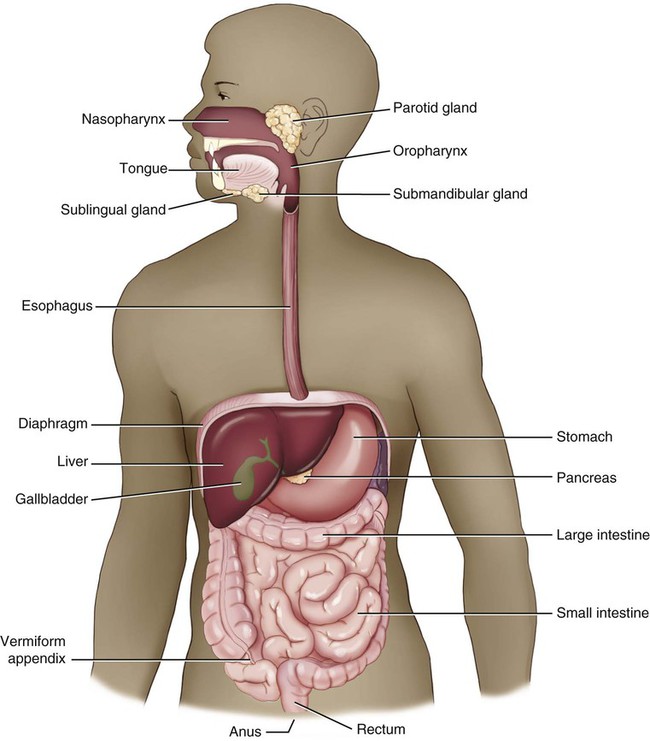
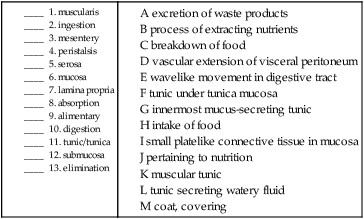
The digestive system (Fig. 5-1) provides the nutrients needed for cells to replicate themselves continually and build new tissue. This is done through several distinct processes: ingestion, the intake of food; digestion, the mechanical and chemical breakdown of food; absorption, the process of extracting nutrients; and elimination, the excretion of any waste products. Other names for this system are the gastrointestinal (GI) tract, which refers to the two main parts of the system (the stomach and intestines) and the alimentary canal, which refers to the function of the tubelike nature of the majority of the digestive system, which starts at the mouth and continues in varying diameters to the anus.
Anatomy and Physiology
Overview
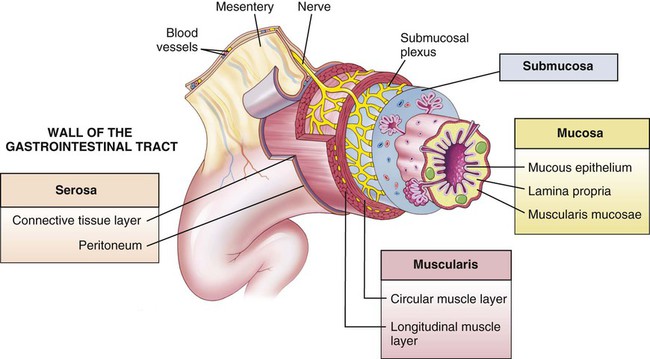
Most of the alimentary canal is in four coats, or tunics: the mucosa, the submucosa, the muscularis, and the serosa (Fig. 5-2). The inner tunic is the mucosa, which secretes gastric juices, absorbs nutrients, and protects the tissue through the production of mucus, a thick, slimy emission. This membrane is lined with a single layer of epithelial tissue that is attached to a platelike layer of connective tissue, the lamina propria. You might want to note that the combining form lamin/o, used to mean a “thin plate,” appears throughout many body systems. The term propria is from Latin and means “one’s own, or special” and is most likely used to designate this particular lamina from the many others in the body. The submucosa, the tunic underneath the tunica mucosa, holds blood, lymphatic, and nervous tissues that nourish, protect, and communicate. The next tunic is the muscularis, two layers of circular and longitudinal muscles that contract and relax around the tube in a wavelike movement termed peristalsis. If peristalsis is absent or delayed, the movement of food through the tract is impaired, causing disorders like constipation. The outermost tunic has different names in the digestive system, depending on whether it occurs within or outside of the peritoneal cavity. If outside, an outer tunic covering that binds a structure together is called the adventitia (also tunica externa). The tunic within the peritoneal cavity that emits a slippery fluid to counteract friction is termed the serosa. The serosa and visceral peritoneum are synonymous. All of these four layers are then attached to the body wall in the peritoneum by a rich vascular membrane which is an extension of the visceral peritoneum termed the mesentery.
Oral Cavity
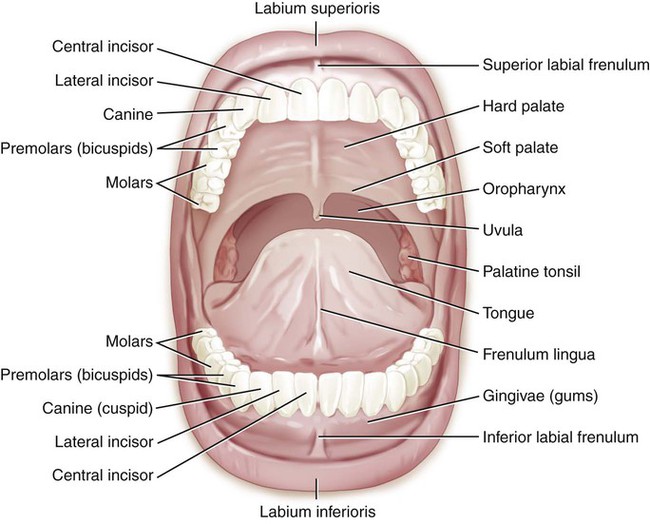
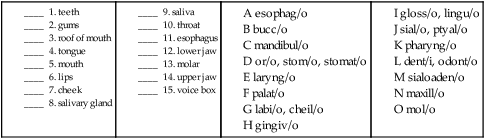
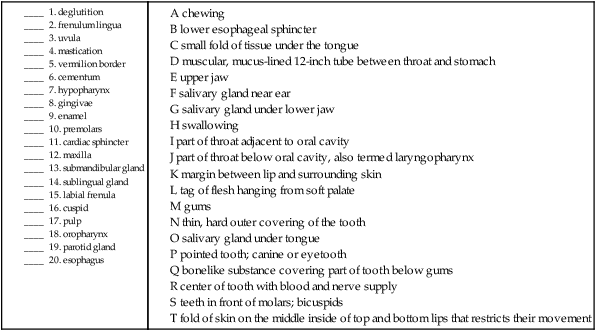
Food normally enters the body through the mouth, or oral cavity (Fig. 5-3). The digestive function of this cavity is to break down the food mechanically by chewing (mastication) and lubricate the food to make swallowing (deglutition) easier.
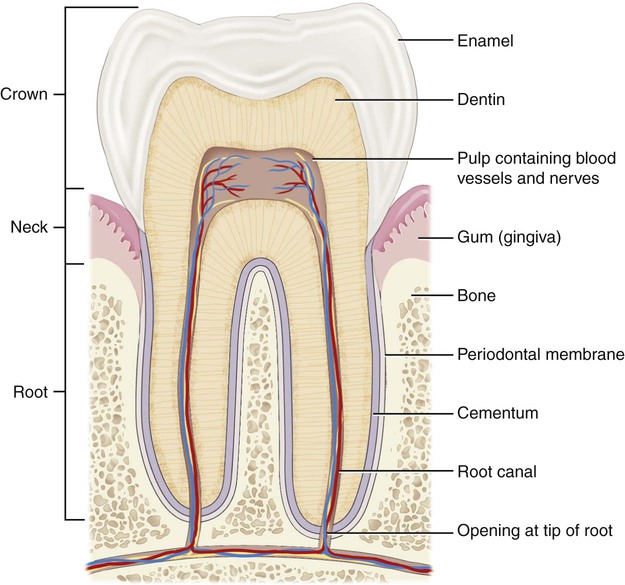
The upper and lower jaws (maxilla and mandible) hold approximately 32 permanent teeth that are set in the fleshy gums (gingivae) of the alveolar ridges of each bone. The thin, hard outer covering of the tooth is the enamel, while the dentin is the calcified second layer of the tooth (Fig. 5-4). The pulp is the center of the tooth with a blood and nerve supply. Cementum is a bonelike substance that covers the part of the tooth that is below the gums. The crown of the tooth is the visible enamel, the root is the area below the gums, and the neck is the area where both of these meet. The teeth are named by their function, location, or appearance. The central and lateral incisors are the front teeth that initially tear food to be chewed on the back teeth, the molars (derived from Latin for grinding). In between the incisors and the molars, the teeth are named for the number of points (cusps), either as cuspids or bicuspids (also called premolars because they are in front of the molars). Another name for the cuspids is the canines, because of the perceived similarity to the dentition of dogs. The upper cuspids were also called eyeteeth, because in the past, it was thought that the eyes and these teeth shared the same nerve supply. Molars have between 3-5 cusps, but their name is taken from their function, not the number of pointed projections. Periodontal ligaments anchor the teeth in their sockets to the alveolar bone of the upper or lower jaw. Note that the reason that periodontal disease causes a loosening of the teeth is that the tooth/bone bond has been compromised or destroyed.
Throat
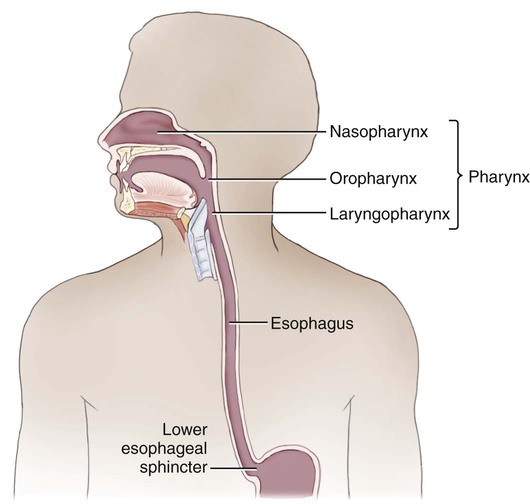
The throat, or pharynx, is the passageway that connects the oral and nasal cavities with the esophagus (Fig. 5-5). It can be divided into three main parts: the nasopharynx, the oropharynx, and the hypopharynx. The nasopharynx is the most superior part of the pharynx, located behind the nasal cavity. The oropharynx is the part of the throat directly adjacent to the oral cavity, and the hypopharynx (also called the laryngopharynx because of its proximity to the larynx, which is the voice box) is the part of the throat directly below the oropharynx. The piriform recess (sinus or fossa) is the pear-shaped cavity in the hypopharynx near the opening to the voice box. This site is significant because food has a propensity for becoming lodged there.
Peritoneum
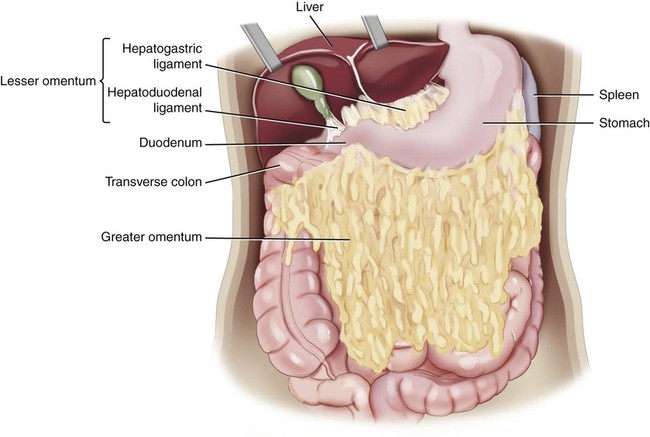
The peritoneal cavity is divided into two main regions: the greater sac and the lesser sac. These two regions are connected by an opening termed the epiploic foramen (also called the foramen of Winslow). The greater sac is the main cavity of the peritoneal cavity, while the lesser sac is formed by two separate folds termed omenta. The omenta (sing. omentum) are folds of peritoneum that extend from the stomach, further compartmentalizing the peritoneal cavity and serving as sites of fat deposition, protecting against trauma and infection, and providing an immune support function (Fig. 5-6). The greater omentum extends from the greater curvature of the stomach, covers the intestines, and merges into the parietal peritoneum. The lesser omentum (also termed the omental bursa) extends from the lesser curvature of the stomach and connects to the liver.
Stomach
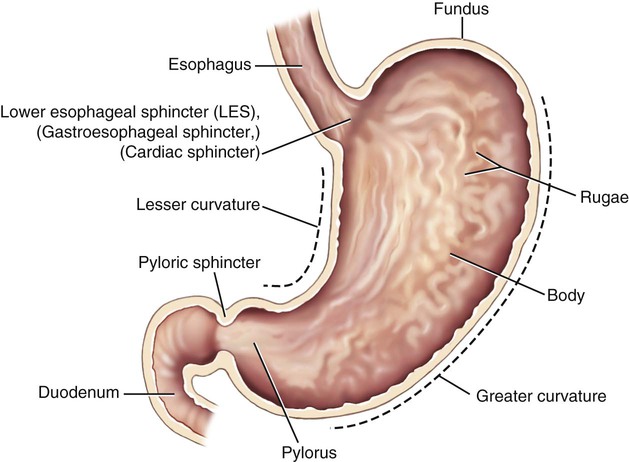
The stomach, an expandable saclike vessel located between the esophagus and the small intestines, has three main functions (Fig. 5-7). It begins the process of digesting proteins by storing the swallowed food and mixing it with gastric juices and hydrochloric acid to further the digestive process chemically. This mixture is called chyme. The smooth muscles of the stomach contract to aid in the mechanical digestion of the food. A continuous coating of mucus protects the stomach and the rest of the digestive system from the acidic nature of the gastric juices. Finally, the partially digested mixture is moved to the small intestines.
Small Intestine
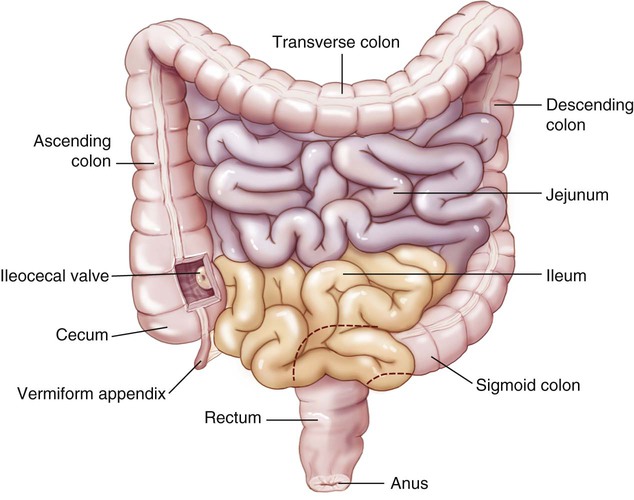
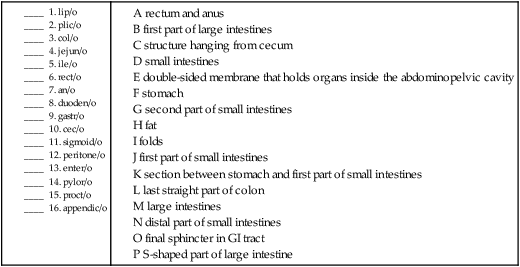
Once the chyme has been formed in the stomach, the pyloric sphincter relaxes a bit at a time to release portions of it into the first part of the small intestine, called the duodenum (Fig. 5-8). The small intestine gets its name, not because of its length (it is about 20 feet long), but because of the diameter of its lumen (a tubular cavity within the body). The second part of the small intestine is the jejunum and the distal part is the ileum. The duodenojejunal flexure is the border between the first two sections of the small intestines.
Large Intestine
In contrast to the small intestine, the large intestine (see Fig. 5-8) is only about 5 feet long, but it is much wider in diameter. The primary function of the large intestine is the elimination of waste products from the body. Some synthesis of vitamins occurs in the large intestine, but unlike the small intestine, the large intestine has no villi and is not well suited for absorption of nutrients. The ileocecal valve is the exit from the small intestine and the entrance to the colon. The first part of the large intestine, the cecum, has a wormlike appendage, called the vermiform appendix (pl. appendices), dangling from it. Although this organ does not seem to have any direct function related to the digestive system, it is thought to have a possible immunological defense mechanism.
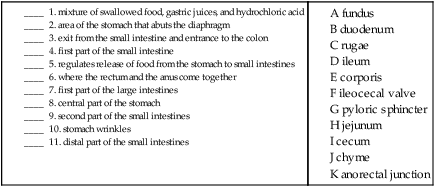
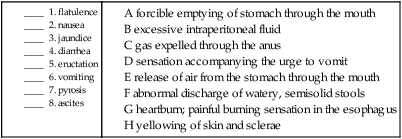
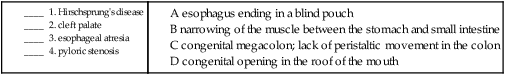
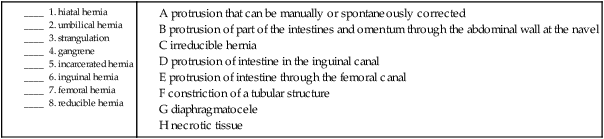
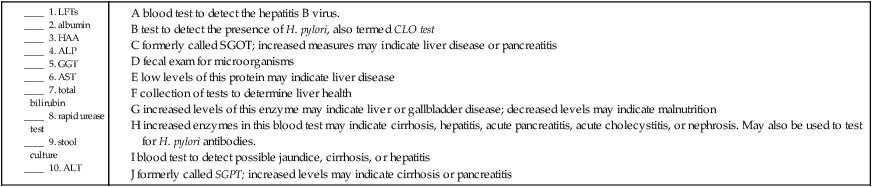
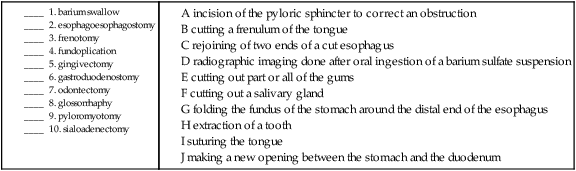
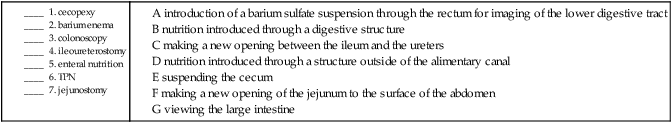
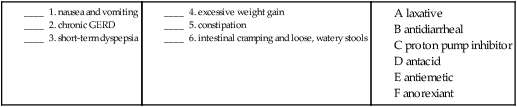
B. Match the term with the correct definition.
Accessory Organs (Adnexa)
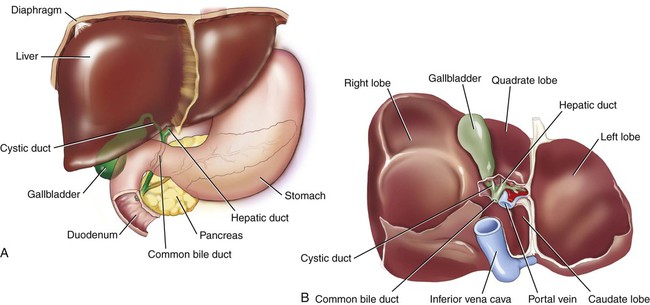
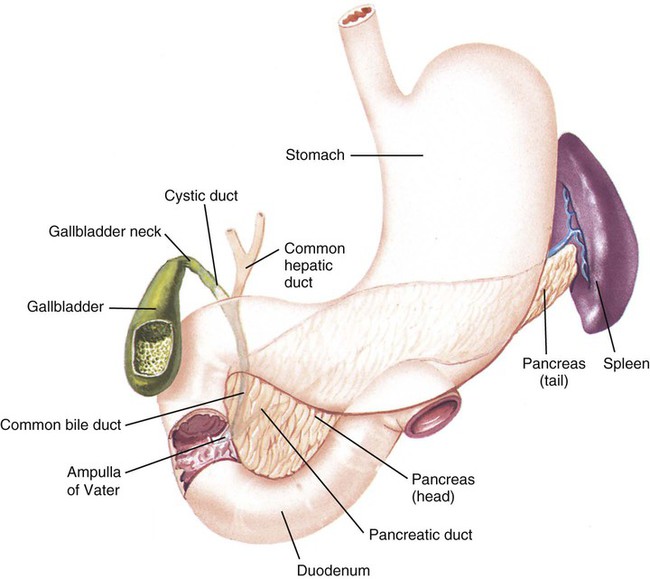
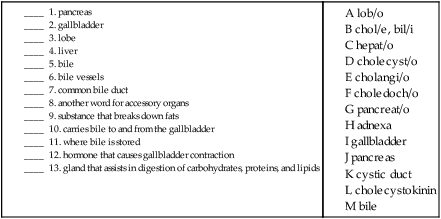
The accessory organs are the gallbladder (GB), liver, and pancreas (Fig. 5-9). These organs secrete fluid into the GI tract but are not a direct part of the tube itself. Sometimes accessory structures are referred to as adnexa.
The liver forms a substance called bile, which emulsifies, or mechanically breaks down, fats into smaller particles so that they can be chemically digested. Bile is composed of bilirubin, the waste product formed by the normal breakdown of hemoglobin in red blood cells at the end of their life spans, and cholesterol, a fatty substance found only in animal tissues (Fig. 5-10). Bile is released from the liver through the right and left hepatic ducts, which join to form the hepatic duct. The cystic duct carries bile to and from the gallbladder. When the hepatic and cystic ducts merge, they form the common bile duct, which empties into the duodenum. Collectively, all of these ducts are termed bile vessels. Bile is stored in the gallbladder, a small sac found on the underside of the right lobe of the liver. When fatty food enters the duodenum, a hormone called cholecystokinin is secreted, causing a contraction of the gallbladder to move bile out into the cystic duct, then the common bile duct, and finally into the duodenum.
The pancreas is a gland located in the upper left quadrant. It is involved in the digestion of the three types of food molecules: carbohydrates, proteins, and lipids. The pancreatic enzymes are carried through the pancreatic duct, which empties into the common bile duct. Pancreatic involvement in food digestion is an exocrine function because the secretion is into a duct. Pancreatic endocrine functions (secretion into blood and lymph vessels) are discussed in Chapter 15.
Combining Forms for the Anatomy of the Digestive System
| Meaning | Combining Form |
| abdomen | abdomin/o, celi/o, lapar/o |
| accessory | adnex/o |
| anus | an/o |
| appendix | appendic/o, append/o |
| bile | chol/e, bil/i |
| bile vessel | cholangi/o |
| bolus | bol/o |
| cecum | cec/o |
| cheek | bucc/o |
| cholesterol | cholesterol/o |
| common bile duct | choledoch/o |
| corporis, body | corpor/o |
| duodenum | duoden/o |
| enamel | amel/o |
| esophagus | esophag/o |
| fat, lipid | lip/o, lipid/o |
| feces | fec/a |
| fold, plica | plic/o |
| fundus | fund/o |
| gallbladder | cholecyst/o |
| glucose, sugar | gluc/o, glyc/o |
| gums | gingiv/o |
| ileum | ile/o |
| intestines | intestin/o |
| jejunum | jejun/o |
| large intestine, colon | col/o, colon/o |
| lips | cheil/o, labi/o |
| liver | hepat/o |
| lobe | lob/o |
| lower jaw | mandibul/o |
| lumen | lumin/o |
| mouth, oral cavity | or/o, stom/o, stomat/o |
| mucus | mucos/o |
| nose | nas/o, rhin/o |
| nutrition | aliment/o |
| omentum | epiplo/o |
| palate | palat/o |
| pancreas | pancreat/o |
| peritoneum | peritone/o |
| pharynx, throat | pharyng/o |
| pylorus | pylor/o |
| rectum | rect/o |
| rectum and anus | proct/o |
| rugae | rug/o |
| saliva | sial/o, ptyal/o |
| salivary duct | sialodoch/o |
| salivary gland | sialoaden/o |
| sigmoid colon | sigmoid/o |
| small intestine | enter/o |
| starch | amyl/o |
| stomach | gastr/o |
| teeth | dent/i, odont/o |
| tongue | gloss/o, lingu/o |
| upper jaw | maxill/o |
| uvula | uvul/o |
| villus | vill/o |
Prefixes for the Anatomy of the Digestive System
| Prefix | Meaning |
| endo- | within |
| exo- | outside |
| hypo- | below |
| par- | near |
| peri- | surrounding |
| retro- | behind |
| sub- | under |
Suffixes for the Anatomy of the Digestive System
| Suffix | Meaning |
| -al, -ar, -ary, -eal, -id, -ine, -ous, -ic | pertaining to |
| -ase | enzyme |
| -crine | to secrete |
| -kinin | movement substance |
| -stalsis | contraction |
Pathology
Terms Related to Symptoms and Signs Involving the Digestive System and Abdomen (R1Ø-R19)
| Term | Word Origin | Definition |
| ascites | Excessive intraperitoneal fluid. | |
| diarrhea | dia- through, complete -rrhea discharge, flow |
Abnormal discharge of watery, semisolid stools. |
| dysphagia | dys- difficult, bad -phagia condition of swallowing, eating |
Difficulty with swallowing that may be due to an obstruction (e.g., a tumor) or a motor disorder (e.g., a spasm). |
| eructation | Release of air from the stomach through the mouth. Eructation may be caused by rapid eating or by intentionally or unintentionally swallowing air (aerophagia). Also called burping or belching. | |
| flatulence | Gas expelled through the anus. Also called flatus. | |
| gastralgia | gastr/o stomach -algia pain |
Abdominal pain. Also called gastrodynia. |
| halitosis | halit/o breath -osis abnormal condition |
Bad-smelling breath. |
| hepatomegaly | hepat/o liver -megaly enlargement |
Enlargement of the liver. |
| jaundice | Yellowing of the skin and sclerae (whites of the eyes) caused by elevated levels of bilirubin. Also called icterus. | |
| nausea | Sensation that accompanies the urge to vomit but does not always lead to vomiting. The abbreviation N&V refers to nausea and vomiting. The term is derived from a Greek word meaning seasickness. | |
| pyrosis | pyr/o fire -osis abnormal condition |
Painful burning sensation in esophagus, usually caused by reflux of stomach contents, hyperactivity, or peptic ulcer. Also known as heartburn. |
| vomiting | Forcible or involuntary emptying of the stomach through the mouth. The material expelled is called vomitus or emesis. |
9. pain in the stomach _____________________________________________________________________________
10. condition of difficulty with swallowing ___________________________________________________________
11. abnormal condition of the breath ________________________________________________________________
Terms Related to Congenital Conditions (QØØ-Q99)
| Term | Word Origin | Definition |
| ankyloglossia | ankyl/o stiffening gloss/o tongue -ia condition |
An inability to move the tongue freely as a result of a congenital shortened frenulum. Also referred to as being “tongue-tied.” |
| cleft palate | Failure of the palate to close during embryonic development, creating an opening in the roof of the mouth. Cleft palate often is accompanied by a cleft lip (Fig. 5-11). | |
| esophageal atresia | esophag/o esophagus -eal pertaining to a- no, not, without -tresia condition of an opening |
Esophagus that ends in a blind pouch and therefore lacks an opening into the stomach (Fig. 5-12). |
| gastroschisis | gastr/o stomach -schisis split |
A congenital opening in the anterior abdominal wall. |
| Hirschsprung’s disease | Congenital absence of normal nervous function in part of the colon, which results in an absence of peristaltic movement, accumulation of feces, and an enlarged colon. Also called congenital megacolon. | |
| omphalocele | omphal/o umbilicus -cele herniation, protrusion |
A congenital herniation at the umbilicus. Also called exomphalos. |
| pyloric stenosis | pylor/o pylorus -ic pertaining to stenosis narrowing |
Condition in which the muscle between the stomach and the small intestine narrows or fails to open adequately to allow partially digested food into the duodenum. |
5. gastroschisis ______________________________________________________________________________________
6. omphalocele _____________________________________________________________________________________
7. ankyloglossia _____________________________________________________________________________________
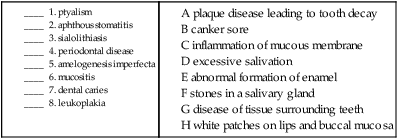
Terms Related to Diseases of Oral Cavity and Salivary Glands (KØØ-K14)
| Term | Word Origin | Definition |
| amelogenesis imperfecta | amel/o enamel -genesis production, origin |
An abnormal formation of tooth enamel, resulting in separation from the dentin beneath. |
| anodontia | an- no, not, without odont/o teeth -ia condition |
Either complete or partial lack of teeth. Also referred to as edentulous. |
| aphthous stomatitis | aphth/o ulceration -ous pertaining to stomat/o mouth -itis inflammation |
Recurring condition characterized by small erosions (ulcers), which appear on the mucous membranes of the mouth. Also called a canker sore (Fig. 5-13). |
| cheilitis | cheil/o lip -itis inflammation |
Inflammation of the lips. |
| dental caries | dent/i teeth -al pertaining to |
Plaque disease caused by an interaction between food and bacteria in the mouth, leading to tooth decay. Also called cavities. |
| gingivitis | gingiv/o gums -itis inflammation |
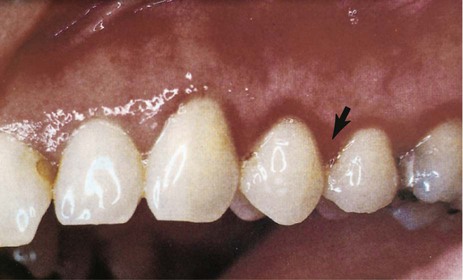
Inflammatory disease of the gums characterized by redness, swelling, and bleeding (Fig. 5-14). |
| glossitis | gloss/o tongue -itis inflammation |
Inflammation of the tongue. |
| oral mucositis | or/o mouth -al pertaining to mucos/o mucus -itis inflammation |
Inflammation of the mucous membranes of the mouth. Gastrointestinal mucositis may be an adverse effect of chemotherapy and can occur throughout the GI tract. |
| oral leukoplakia | or/o mouth -al pertaining to leuk/o white -plakia condition of patches |
Condition of white patches that may appear on the lips and buccal mucosa (Fig. 5-15). It usually is associated with tobacco use and may be precancerous. |
| periodontal disease | peri- surrounding odont/o tooth -al pertaining to |
Pathological condition of the tissues surrounding the teeth. |
| ptyalism | ptyal/o saliva -ism condition |
Condition of excessive salivation. |
| sialoadenitis | sialoaden/o salivary gland -itis inflammation |
Inflammation of a salivary gland. |
| sialolithiasis | sial/o saliva lith/o stone -iasis presence of, condition |
Condition of stones in a salivary gland or duct. |
9. gingivitis _______________________________________________________________________________________
10. glossitis _________________________________________________________________________________________
11. anodontia ______________________________________________________________________________________
12. sialoadenitis ____________________________________________________________________________________
13. cheilitis _________________________________________________________________________________________
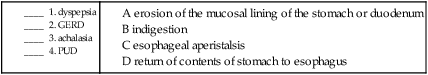
Terms Related to Diseases of Esophagus, Stomach, and Duodenum (K2Ø-K31)
| Term | Word Origin | Definition |
| achalasia | a- without -chalasia condition of relaxation |
Impairment of esophageal peristalsis along with the lower esophageal sphincter’s inability to relax. Also called cardiospasm, esophageal aperistalsis, and megaesophagus. |
| dyspepsia | dys- abnormal, bad -pepsia digestion condition |
Feeling of epigastric discomfort that occurs shortly after eating. The discomfort may include feelings of nausea, fullness, heartburn, and/or bloating. Also called indigestion. |
| esophagitis | esophag/o esophagus -itis inflammation |
Inflammation of the esophagus. |
| gastritis | gastr/o stomach -itis inflammation |
Acute or chronic inflammation of the stomach that may be accompanied by anorexia (lack of appetite), nausea, and vomiting, or indigestion. |
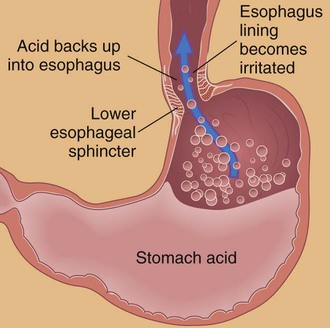
| gastroesophageal reflux disease (GERD) | gastr/o stomach esophag/o esophagus -eal pertaining to re- back -flux flow |
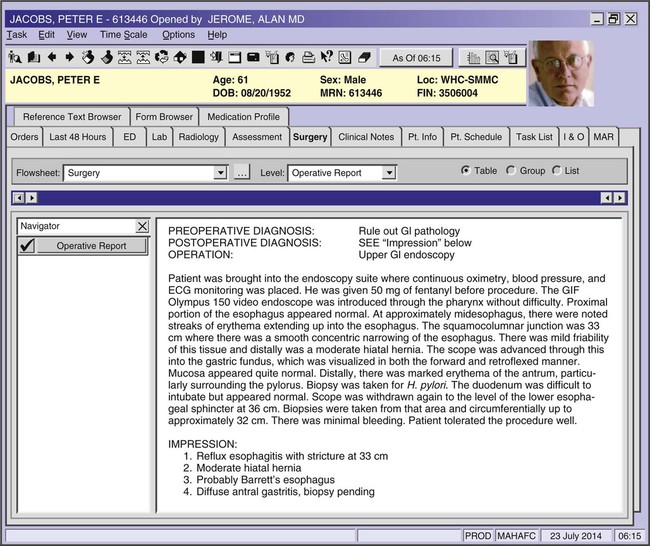
Flowing back, or return, of the contents of the stomach to the esophagus caused by an inability of the lower esophageal sphincter (LES) to contract normally; characterized by pyrosis with or without regurgitation of stomach contents to the mouth (Fig. 5-16). Barrett’s esophagus is a condition caused by chronic reflux from the stomach. It is associated with an increased risk of cancer. |
| peptic ulcer disease (PUD) | An erosion of the protective mucosal lining of the stomach or duodenum (Fig. 5-17). Also called a gastric or duodenal ulcer, depending on the site. |
5. gastritis __________________________________________________________________________________________
6. achalasia _________________________________________________________________________________________
7. dyspepsia ________________________________________________________________________________________
8. esophagitis _______________________________________________________________________________________
Terms Related to Diseases of Appendix (K35-K38)
| Term | Word Origin | Definition |
| appendicitis | appendic/o appendix -itis inflammation |
Inflammation of the vermiform appendix (Fig. 5-18). May be acute or chronic, with or without peritonitis. |
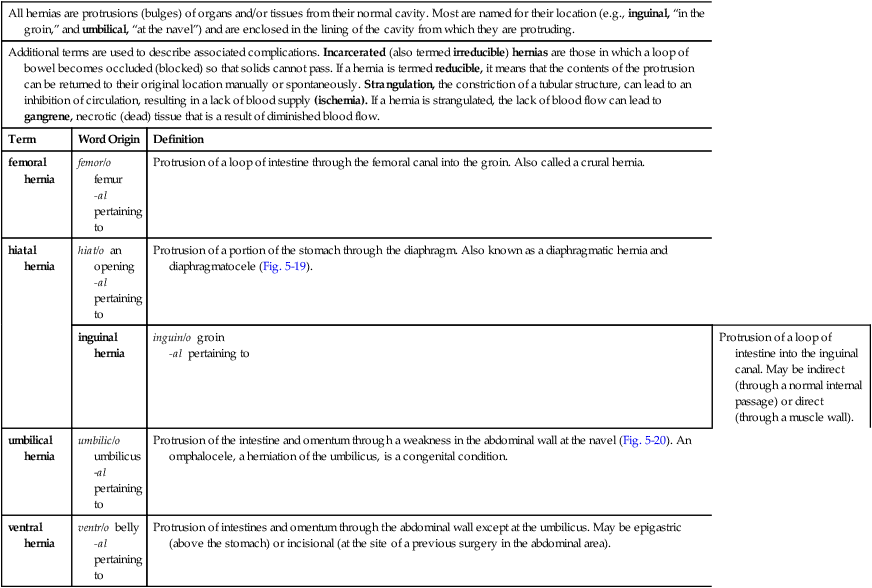
Terms Related to Hernias (K4Ø-K46)
| All hernias are protrusions (bulges) of organs and/or tissues from their normal cavity. Most are named for their location (e.g., inguinal, “in the groin,” and umbilical, “at the navel”) and are enclosed in the lining of the cavity from which they are protruding. | ||
| Additional terms are used to describe associated complications. Incarcerated (also termed irreducible) hernias are those in which a loop of bowel becomes occluded (blocked) so that solids cannot pass. If a hernia is termed reducible, it means that the contents of the protrusion can be returned to their original location manually or spontaneously. Strangulation, the constriction of a tubular structure, can lead to an inhibition of circulation, resulting in a lack of blood supply (ischemia). If a hernia is strangulated, the lack of blood flow can lead to gangrene, necrotic (dead) tissue that is a result of diminished blood flow. | ||
| Term | Word Origin | Definition |
| femoral hernia | femor/o femur -al pertaining to |
Protrusion of a loop of intestine through the femoral canal into the groin. Also called a crural hernia. |
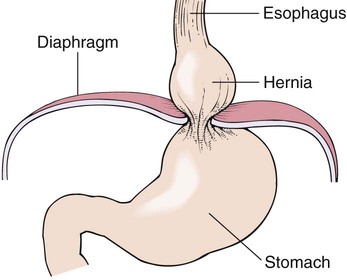
| hiatal hernia | hiat/o an opening -al pertaining to |
Protrusion of a portion of the stomach through the diaphragm. Also known as a diaphragmatic hernia and diaphragmatocele (Fig. 5-19). |
| inguinal hernia | inguin/o groin -al pertaining to |
Protrusion of a loop of intestine into the inguinal canal. May be indirect (through a normal internal passage) or direct (through a muscle wall). |
| umbilical hernia | umbilic/o umbilicus –al pertaining to |
Protrusion of the intestine and omentum through a weakness in the abdominal wall at the navel (Fig. 5-20). An omphalocele, a herniation of the umbilicus, is a congenital condition. |
| ventral hernia | ventr/o belly -al pertaining to |
Protrusion of intestines and omentum through the abdominal wall except at the umbilicus. May be epigastric (above the stomach) or incisional (at the site of a previous surgery in the abdominal area). |
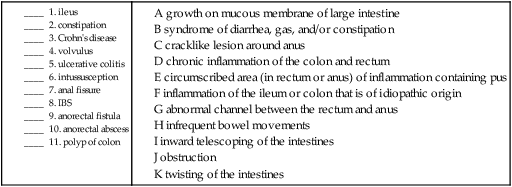
Terms Related to Noninfective Enteritis and Colitis (K5Ø-K52)
| Term | Word Origin | Definition |
| colitis | col/o colon -itis inflammation |
Inflammation of the large intestine. |
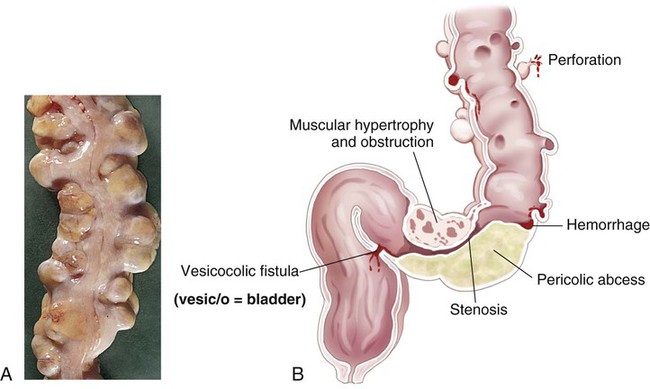
| Crohn’s disease | Inflammation of the ileum or the colon that is of idiopathic origin. Also called regional or granulomatous enteritis. | |
| ulcerative colitis | col/o colon -itis inflammation |
Chronic inflammation of the colon and rectum manifesting with bouts of profuse, watery diarrhea. Both Crohn’s disease and ulcerative colitis are types of inflammatory bowel disease (IBD). |
Terms Related to Other Diseases of the Intestines (K55-K63)
| Term | Word Origin | Definition |
| anal fissure | an/o anus -al pertaining to |
Cracklike lesion of the skin around the anus. |
| anorectal abscess | an/o anus rect/o rectum -al pertaining to |
Circumscribed area of inflammation in the anus or rectum, containing pus. |
| anorectal fistula | an/o anus rect/o rectum -al pertaining to |
Abnormal channel between the rectum and the anus. Fistulas may occur between organs or between an organ and the surface of the body. |
| constipation | Infrequent, incomplete, or delayed bowel movements. Obstipation is intractable (difficult to manage) constipation or an intestinal obstruction. | |
| diverticulitis | diverticul/o diverticulum -itis inflammation |
Inflammation occurring secondary to the occurrence of diverticulosis. |
| diverticulosis | diverticul/o diverticulum -osis abnormal condition |
Development of diverticula, pouches in the lining of the intestines (Fig. 5-21), both large and small. |
| ileus | Obstruction. Paralytic ileus is lack of peristaltic movement in the intestinal tract. Also called adynamic ileus. | |
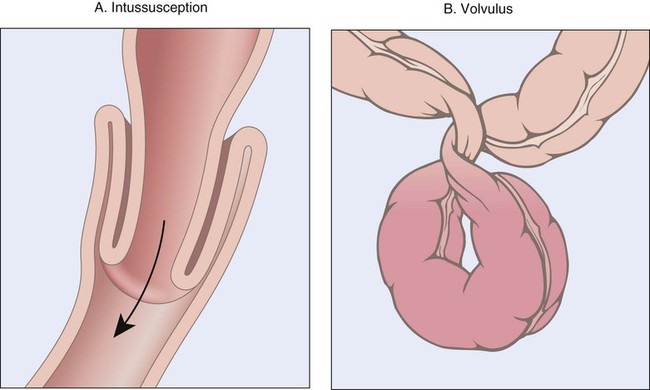
| intussusception | Inward telescoping of the intestines (Fig. 5-22). | |
| irritable bowel syndrome (IBS) | Diarrhea, gas, and/or constipation resulting from stress with no underlying disease. | |
| polyp of colon | Benign growth on the mucous membrane of large intestine. | |
| proctitis | proct/o rectum and anus -itis inflammation |
Inflammation of the rectum and anus. Also called rectitis. |
| proctoptosis | proct/o rectum and anus -ptosis drooping, prolapse |
Prolapse of the rectum outside of the anus. |
| volvulus | Twisting of the intestine (see Fig. 5-22). |
12. drooping of the rectum and anus ________________________________________________________________
13. inflammation of a diverticulum __________________________________________________________________
14. inflammation of the rectum and anus ____________________________________________________________
15. abnormal condition of a diverticulum ____________________________________________________________
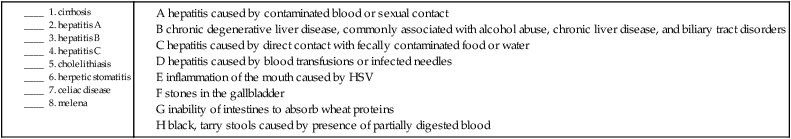
Terms Related to Diseases of Peritoneum and Retroperitoneum (K65-K68) and Diseases of Liver (K7Ø-K77)
| Term | Word Origin | Definition |
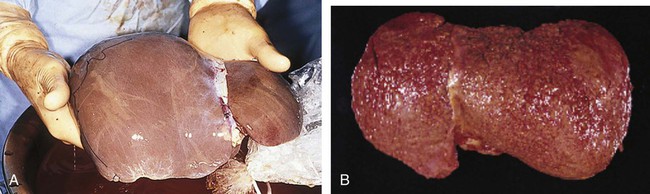
| cirrhosis | cirrh/o orange-yellow -osis abnormal condition |
Chronic degenerative disease of the liver, commonly associated with alcohol abuse, chronic liver disease, and biliary tract disorders (Fig. 5-23). |
| peritonitis | peritone/o peritoneum -itis inflammation |
Inflammation of the peritoneum that most commonly occurs when an inflamed appendix ruptures. An additional code is needed to identify an infectious agent. |
Terms Related to Diseases of Gallbladder, Biliary Tract, and Pancreas (K8Ø-K87)
| Term | Word Origin | Definition |
| cholangitis | cholangi/o bile vessel -itis inflammation |
Inflammation of the bile vessels. |
| cholecystitis | cholecyst/o gallbladder -itis inflammation |
Inflammation of the gallbladder, either acute or chronic. May be caused by choledocholithiasis or cholelithiasis. |
| choledocholithiasis | choledoch/o common bile duct lith/o stones -iasis presence of |
Presence of stones in the common bile duct (Fig. 5-24). |
| cholelithiasis | chol/e gall, bile lith/o stones -iasis presence of |
Presence of stones (calculi) in the gallbladder, sometimes characterized by right upper quadrant pain (biliary colic) with nausea and vomiting (Fig. 5-25). |
| pancreatitis | pancreat/o pancreas -itis inflammation |
Inflammation of the pancreas, which may be acute or chronic. |
Terms Related to Other Diseases of Digestive System (K9Ø-K94)
| Term | Word Origin | Definition |
| celiac disease | celi/o abdomen -ac pertaining to |
Inability of intestines to absorb wheat proteins. Also called celiac sprue. |
| hematemesis | hemat/o blood -emesis vomiting |
Vomiting of blood. |
| melena | melan/o black, dark | Black, tarry stools caused by the presence of partially digested blood. |
Terms Related to Viral Infections Characterized by Skin and Mucous Membranes (BØØ-BØ9) and Viral Hepatitis (B15-B19)
| Term | Word Origin | Definition |
| herpetic stomatitis | stomat/o mouth -itis inflammation |
Inflammation of the mouth caused by the herpes simplex virus (HSV). Also known as a cold sore or fever blister. |
| hepatitis | hepat/o liver -itis inflammation |
Inflammatory disease of the liver that is caused by an increasing number of viruses. Currently named by letter, hepatitis A to G, the means of viral transmission is not the same for each form. The most common forms, A to C, are discussed below. |
| hepatitis A (HAV) | hepat/o liver -itis inflammation |
Virus transmitted through direct contact with fecally contaminated food or water. |
| hepatitis B (HBV) | hepat/o liver -itis inflammation |
Virus transmitted through contaminated blood or sexual contact. |
| hepatitis C (HCV) | hepat/o liver -itis inflammation |
Virus transmitted through blood transfusion, percutaneous inoculation, or sharing of infected needles. |
9. inflammation of the gallbladder __________________________________________________________________
10. inflammation of the liver ________________________________________________________________________
11. presence of stones in the common bile duct ______________________________________________________
12. inflammation of the bile vessels __________________________________________________________________
13. inflammation of the peritoneum _________________________________________________________________
14. inflammation of the pancreas ____________________________________________________________________
15. vomiting of blood _______________________________________________________________________________
Terms Related to Benign Neoplasms (D1Ø-D36)
| Term | Word Origin | Definition |
| cystadenoma | cyst/o bladder, cyst aden/o gland -oma tumor |
Glandular tumors that are filled with cysts; these are the most common benign tumors in the pancreas. |
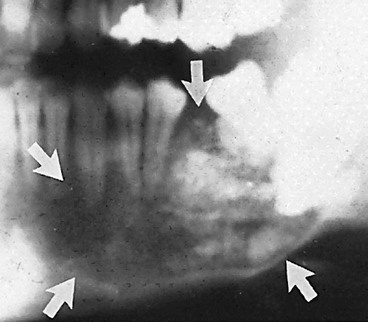
| odontogenic tumor | odont/o tooth -genic pertaining to produced by |
Benign tumors that arise around the teeth and jaw (Fig. 5-26). |
| polyps, adenomatous or hyperplastic | aden/o gland -omatous pertaining to tumor hyper- excessive plas/o formation, growth -tic pertaining to |
Adenomatous (growths that arise from glandular tissue, have potential to become malignant) or hyperplastic (generally, small growths that have no tendency to become malignant) tumors occurring throughout the digestive tract. Polyps may be sessile (flat) or pedunculated (having a stalk) (Fig. 5-27). |
Terms Related to Malignant Neoplasms (CØØ-C96)
| Term | Word Origin | Definition |
| adenocarcinoma | aden/o gland -carcinoma cancerous tumor of epithelial origin |
A malignant tumor of epithelial origin that either originates from glandular tissue or has a glandular appearance. Adenocarcinomas occur throughout the gastrointestinal tract, but especially in the esophagus, stomach, pancreas, and colon. |
| hepatocellular carcinoma/hepatoma | hepat/o liver cellul/o cell -ar pertaining to |
Malignant tumors of epithelial origin that originate in the liver cells. Hepatocellular carcinoma (also called hepatoma) is the most common type of primary liver cancer worldwide. |
| squamous cell carcinoma | squam/o scaly -ous pertaining to |
Cancers that have a scalelike appearance. Squamous cell carcinomas arise from the cells that cover the surfaces of the body. These occur throughout the digestive system. |
Procedures
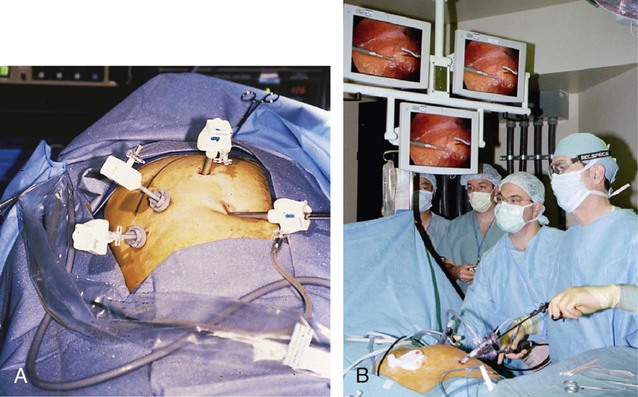
A, A lensed telescope with camera and long instruments are introduced into small incisions. B, The camera image is projected to central monitors.
Terms Related to Laboratory Tests
| Term | Word Origin | Definition |
| alanine transaminase (ALT) | Increased measurement of this particular enzyme usually indicates cirrhosis or pancreatitis. ALT was formerly referred to as SGPT (serum glutamic-pyruvic transaminase). | |
| albumin | A blood test that reveals decreased measurement of this protein formed by the liver. May be low when liver disease occurs. | |
| alkaline phosphatase (ALP) | An increase in this liver enzyme may indicate liver or gallbladder disease. A decrease may indicate malnutrition. | |
| aspartate transaminase (AST) | Increased measurement of AST may indicate liver disease or pancreatitis. A decreased amount may mean uncontrolled diabetes mellitus with ketoacidosis. AST was formerly referred to as SGOT (serum glutamic oxaloacetic acid transaminase). | |
| gamma-glutamyl transferase (GGT) | Blood test to detect increased enzymes that can indicate cirrhosis, hepatitis, acute pancreatitis, acute cholecystitis, or nephrosis, and to test for Helicobacter pylori antibodies. | |
| gastric analysis | gastr/o stomach -ic pertaining to ana- up, apart -lysis breakdown |
Examination to determine the amount of blood, bile, bacteria, and hydrochloric acid in the stomach. Decreased hydrochloric acid may indicate stomach cancer. |
| hepatitis-associated antigen (HAA) | Blood test to detect the hepatitis B virus. | |
| liver function tests (LFTs) | A collection of tests to determine the health of the liver. Includes albumin, total bilirubin, prothrombin time, ALP, ALT, and GGT. | |
| prothrombin time (PT) | pro- before thromb/o clot -in substance |
Blood test to measure the time it takes blood to clot. Prothrombin is a protein that is instrumental in the clotting process and is formed in the liver. Liver disease can decrease the production of prothrombin, which can cause an increased clotting time. |
| rapid urease test | A test to detect the presence of Helicobacter pylori (H. pylori). A gastroscopic biopsy is taken from the gastric antrum. Also termed a CLO test (Campylobacter-like organism test). | |
| stool culture | Fecal exam to test for microorganisms in the feces, such as worms, amoebae, bacteria, and protozoa. | |
| stool guaiac, hemoccult test | hem/o blood -occult hidden |
Fecal specimen exam to detect hidden blood, which may indicate gastrointestinal bleeding. Also referred to as a fecal occult blood test (FOBT). |
| total bilirubin | Blood test to detect possible jaundice (yellowing of the skin), cirrhosis, or hepatitis. |
Terms Related to Upper GI Procedures
| Term | Word Origin | Definition |
| barium swallow (BS) | Radiographic imaging done after oral ingestion of a barium sulfate suspension; used to detect abnormalities of the esophagus and stomach (Fig. 5-28). | |
| esophagoesophagostomy | esophag/o esophagus esophag/o esophagus -stomy making a new opening |
A rejoining of two ends of a cut esophagus, usually as a result of surgery to remove an esophageal defect. |
| esophagogastroduodenoscopy (EGD) | esophag/o esophagus gastr/o stomach duoden/o duodenum -scopy viewing |
Viewing the esophagus, stomach, and first part of the duodenum to aid in the diagnosis of reasons for digestive bleeding, vomiting, and weight loss. |
| frenotomy, frenulotomy | fren/o, frenul/o frenulum –tomy cutting |
Cutting a frenulum of the tongue to treat ankyloglossia. |
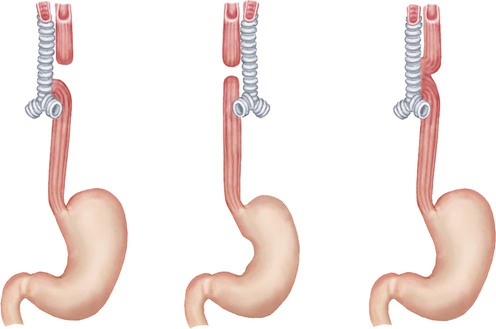
| fundoplication, gastroesophageal | fund/o fundus -plication folding |
Folding the fundus of the stomach around the distal end of the esophagus. Done to treat gastroesophageal reflux. |
| gastroduodenostomy | gastr/o stomach duoden/o duodenum –stomy making a new opening |
A new opening between the stomach and the duodenum (Fig. 5-29). The figure also demonstrates an anastomosis, a new connection between two (usually hollow) structures. |
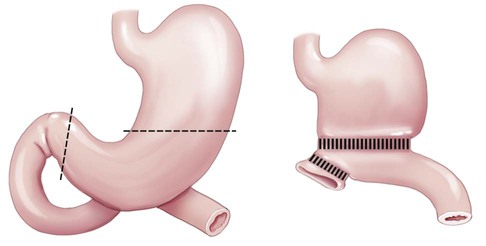
| gastroplasty | gastr/o stomach –plasty surgically forming |
Surgically forming the stomach for the purpose of repair or reshaping. Usually performed as a type of bariatric (weight reduction) surgery. The stomach may be banded, stapled, or cut to reduce its size. |
| gastrostomy | gastr/o stomach –stomy making a new opening |
A new opening in the stomach. A percutaneous endoscopic gastrostomy (PEG) is an opening in the stomach for the purpose of placing a tube for enteral feeding. |
| gingivectomy | gingiv/o gums –ectomy cutting out |
Cutting out part or all of the gums, usually as part of a treatment for periodontal disease. |
| glossorrhaphy | gloss/o tongue -rrhaphy suturing |
Suturing the tongue, usually to repair a lesion or wound. |
| hyperalimentation | hyper- excessive aliment/o nutrition -ation process of |
The therapeutic use of nutritional supplements that exceed recommended daily requirements. |
| manometry, esophageal | man/o pressure -metry measuring |
Test that measures the motor function (muscle pressure) of the esophagus. A manometer is the instrument used to measure pressure. |
| odontectomy | odont/o tooth -ectomy cutting out |
Extraction of a tooth. |
| palatoplasty | palat/o palate -plasty surgically forming |
Surgical correction of the roof of the mouth. May be done to correct a cleft palate or as part of a procedure to treat snoring. |
| pyloromyotomy | pylor/o pylorus my/o muscle -tomy cutting |
An incision of the pyloric sphincter to correct an obstruction, such as pyloric stenosis. |
| sialoadenectomy | sialoaden/o salivary gland -ectomy cutting out |
Removal of a salivary gland (usually the submandibular) due to inflammation of the gland, stones, or cancer. |
| sialodochoplasty | sialodoch/o salivary duct -plasty surgically forming |
Surgical correction of a salivary duct, often following the removal of a stone in a salivary grand. |
| stomatoplasty | stomat/o mouth -plasty surgically forming |
Surgical reconstruction of the mouth to correct malformation due to trauma, disease, or congenital causes. |
| uvulectomy | uvul/o uvula -ectomy cutting out |
Removal of part or all of the uvula, usually to correct snoring. |
11. palatoplasty _____________________________________________________________________________________
12. esophagogastroduodenoscopy ____________________________________________________________________
13. gastroplasty _____________________________________________________________________________________
14. stomatoplasty ___________________________________________________________________________________
Terms Related to Lower GI Procedures
| Term | Word Origin | Definition |
| appendectomy | append/o appendix -ectomy cutting out |
Cutting out the vermiform appendix. If termed an incidental appendectomy, the removal was secondary to another surgery. |
| barium enema (BE) | Introduction of a barium sulfate suspension through the rectum for imaging of the lower digestive tract to detect obstructions, tumors, and other abnormalities. | |
| cecopexy | cec/o cecum -pexy suspension |
Fixation of the cecum to prevent or correct volvulus of the cecum. |
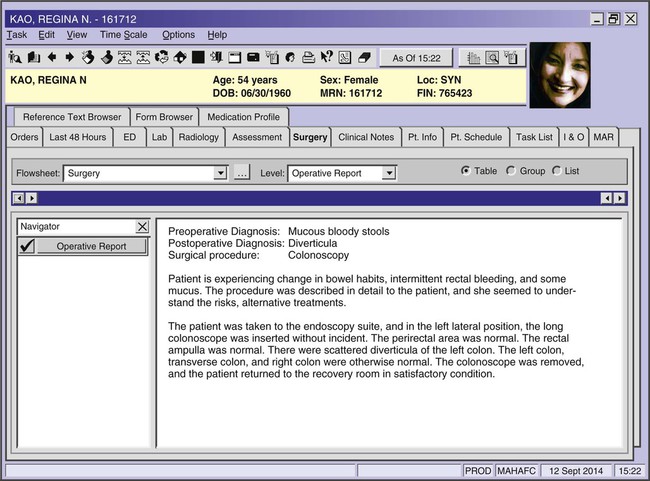
| colonoscopy | colon/o colon, large intestine -scopy viewing |
Viewing the lining of large intestine for screening for cancer, diverticulitis, or other abnormalities. |
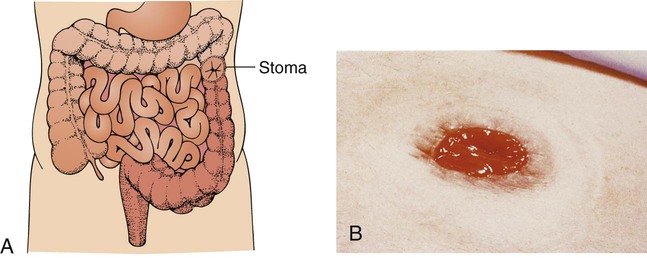
| colostomy | col/o colon, large intestine -stomy making a new opening |
Surgical redirection of the bowel to a stoma, an artificial opening, on the abdominal wall (Fig. 5-30). |
| diverticulectomy | diverticul/o pouch, diverticulum –ectomy cutting out |
Cutting out a diverticulum. |
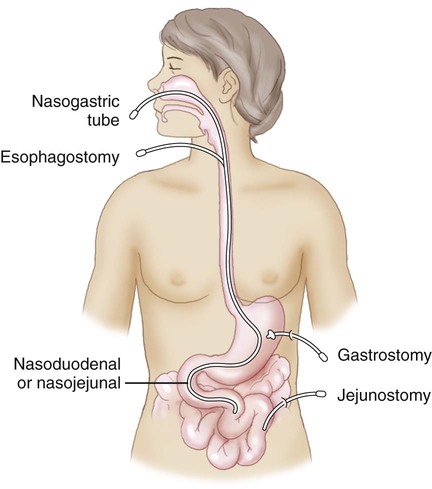
| enteral nutrition | enter/o small intestine -al pertaining to |
Nutrition introduced through a digestive structure (Fig. 5-31). |
| herniorrhaphy | herni/o hernia -rrhaphy suturing |
Suturing a hernia. Approaches may be through an open incision or laparoscopically and may be simply sutured or include a mesh. |
| ileoureterostomy | ile/o ileum ureter/o ureter -stomy making a new opening |
New opening between (anastomosis) the ileum and the ureters in order to conduct urine into the third section of the small intestines when the bladder and urethra are not functional. |
| jejunostomy | jejun/o jejunum -stomy making a new opening |
New opening of the jejunum to the surface of the abdomen for the placement of a feeding tube. |
| omentectomy, omentumectomy | oment/o omentum -ectomy cutting out |
Cutting out part or all of the omentum. Done as part of treatment for ovarian cancer to remove cancer cells that have spread there. |
| peritoneocentesis | peritone/o peritoneum -centesis surgical puncture |
Surgical puncture of the peritoneum to remove fluid. Often used to treat ascites. |
| polypectomy, GI | polyp/o polyp -ectomy cutting out |
Cutting out sessile or pedunculated polyps from the gastrointestinal system. |
| proctoclysis | proct/o rectum and anus -clysis washing |
Cleansing the rectum and anus. An enema. |
| proctoscopy | proct/o rectum and anus -scopy viewing |
Process of viewing the rectum and anus. Used to view hemorrhoids or rectal polyps. |
| pyloromyotomy | pylor/o pylorus my/o muscle -tomy cutting |
An incision of the pyloric sphincter to correct an obstruction, such as pyloric stenosis. |
| sigmoidoscopy | sigmoid/o sigmoid colon -scopy viewing |
Process of viewing the sigmoid colon. |
| total parenteral nutrition (TPN) | par- near, beside enter/o small intestine -al pertaining to |
Nutrition introduced through a structure outside of the alimentary canal, usually by IV because the GI tract is nonfunctional. Enteral nutrition provides sustenance through a feeding tube to the stomach or intestines. |
8. appendectomy __________________________________________________________________________________
9. colonoscopy ____________________________________________________________________________________
10. colostomy ______________________________________________________________________________________
11. peritoneocentesis ________________________________________________________________________________
12. proctoclysis _____________________________________________________________________________________
13. herniorrhaphy __________________________________________________________________________________
Terms Related to Procedures of the Adnexa
| Term | Word Origin | Definition |
| cholangiography | cholangi/o bile vessel -graphy recording |
Process of recording the bile vessels. Radiographic procedure that captures images of the common bile vessel through injection of a contrast medium into the bile duct, after which a series of images is taken. |
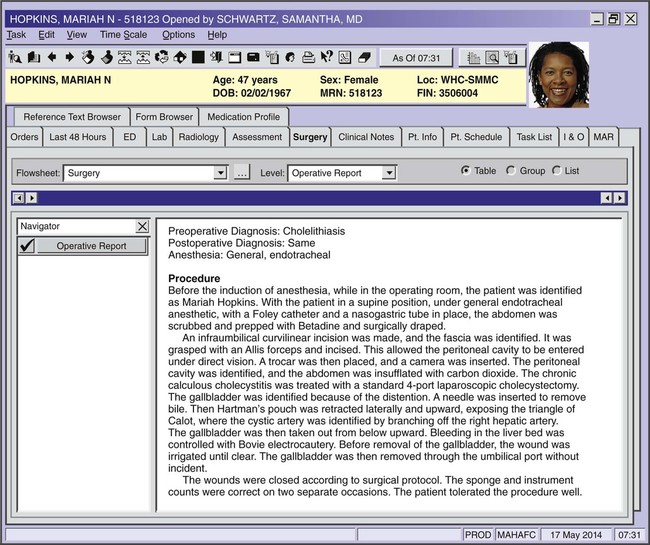
| cholecystectomy | cholecyst/o gallbladder –ectomy cutting out |
Cutting out the gallbladder. If done laparoscopically, the gallbladder is removed through the use of small incisions in the abdomen (Fig. 5-32). |
| choledochectomy | choledoch/o common bile duct –ectomy cutting out |
Cutting out part or all of the common bile duct as part of a procedure to treat cancer in the proximal duodenum. |
| choledocholithotomy | choledoch/o common bile duct –lithotomy cutting out a stone |
Cutting out a stone from the common bile duct. May be done via an open or a laparoscopic approach. |
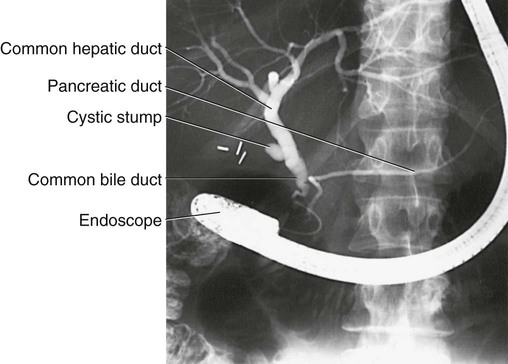
| endoscopic retrograde cholangiopancreatography (ERCP) | endo- below -scopic pertaining to viewing cholangi/o bile vessel pancreat/o pancreas –graphy recording |
Recording the bile vessels and pancreas (Fig. 5-33). An x-ray of the pancreas and bile ducts that is enhanced through the use of radio-opaque dyes; used to diagnose stones, strictures (narrowings), and neoplasms. |
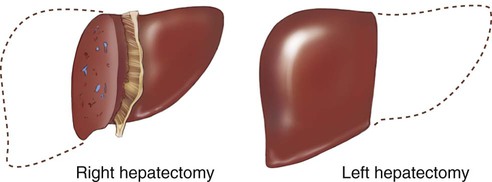
| hepatectomy | hepat/o liver -ectomy cutting out |
Cutting out part or all of the liver. A total hepatectomy is performed for the purpose of a liver transplant. A partial hepatectomy is done for treatment of neoplasms (Fig. 5-34). |
Pharmacology
anorexiants: Appetite suppressants designed to aid in weight control, often in an attempt to treat morbid obesity (an amount of body fat that threatens normal health). Examples of anorexiants are phendimetrazine (Bontril) and phentermine (Adipex-P).
antacids: A buffer (neutralizer) of hydrochloric acid in the stomach to temporarily relieve symptoms of GERD, pyrosis, and ulcers. Examples include calcium carbonate (Tums, Rolaids), and aluminum hydroxide with magnesium hydroxide (Maalox).
antidiarrheals: Provide relief from diarrhea by reducing intestinal motility, inflammation, or loss of fluids and nutrients. Examples include loperamide (Imodium), bismuth subsalicylate (Pepto Bismol), and diphenoxylate with atropine (Lomotil).
antiemetics: Prevent or alleviate nausea and vomiting. Examples include scopolamine (Scopace), ondansetron (Zofran), and promethazine (Phenergan).
gastrointestinal stimulants: Promote motility of smooth muscles in gastrointestinal tract. An example is metoclopramide (Reglan).
histamine-2 receptor antagonists (H2RAs): Reduce hydrochloric acid production in the stomach for moderate-lasting acid suppression. Examples include famotidine (Pepcid) and ranitidine (Zantac).
laxatives: Promote evacuation of the bowel by increasing the bulk of the feces, softening the stool, or lubricating the intestinal wall. Examples include fiber and docusate (Colace). Simulant laxatives cause more direct bowel evacuation by stimulating peristalsis. Examples include senna (Ex-Lax) and bisacodyl (Dulcolax).
proton pump inhibitors: Reduce production of hydrochloric acid in the stomach for long-lasting acid suppression of disorders like GERD. Examples include omeprazole (Prilosec) and pantoprazole (Protonix).
Recognizing Suffixes for PCS
Suffixes and Root Operations for the Digestive System
| Suffix | Root Operation |
| -centesis | Drainage |
| -ectomy | Excision, resection |
| -lithotomy | Extirpation |
| -pexy | Repair, reposition |
| -plasty | Repair, supplement, replacement |
| -plication | Restriction |
| -rrhaphy | Repair, supplement |
| -scopy | Inspection |
| -stomy | Bypass, drainage |
| -tomy | Drainage, release, division |
| Abbreviation | Meaning |
| BE | barium enema |
| BM | bowel movement |
| BS | barium swallow |
| CLO | Campylobacter-like organism test |
| EGD | esophagogastroduodenoscopy |
| ERCP | endoscopic retrograde cholangiopancreatography |
| FOBT | fecal occult blood test |
| GB | gallbladder |
| GERD | gastroesophageal reflux disease |
| GI | gastrointestinal |
| HAV | hepatitis A virus |
| HBV | hepatitis B virus |
| HCV | hepatitis C virus |
| HSV | herpes simplex virus |
| IBD | inflammatory bowel disease |
| IBS | irritable bowel syndrome |
| LES | lower esophageal sphincter |
| N&V | nausea and vomiting |
| PEG | percutaneous endoscopic gastrostomy |
| PUD | peptic ulcer disease |
| TPN | total parenteral nutrition |