24. DiGeorge Syndrome
Definition
DiGeorge syndrome is a congenital disorder involving hypoplasia or aplasia of the thymus and parathyroid glands secondary to defective development of the third and fourth pharyngeal pouches.
Incidence
DiGeorge syndrome occurs very sporadically. The prevalence is the subject of much debate; however, current estimates of the incidence range from 1:4000 to 1:6395. Male to female ratio is 1:1.
Etiology
The anomaly results from deletion of the DiGeorge syndrome chromosome region (DGCR), represented as deletion on chromosome 22q11.2.
Conditions Associated with DiGeorge Syndrome
• 22q11 deletion syndromes
• Cayler syndrome∗
∗See Appendix G: Rare Syndroms.
• CHARGE syndrome (see box)
• Conotruncal anomaly face syndrome∗
• Opitz-GBBB syndrome∗
• Velocardiofacial syndrome
CHARGE Association
Coloboma of the iris, choroid, and/or microphthalmia
Heart defect
Atresia of the choanae
Retarded growth and development
Genitourinary abnormalities (cryptorchidism, microphallus, hydronephrosis)
Ear defects associated with deafness
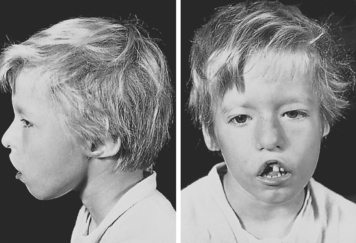 |
| DiGeorge Syndrome. Facial anomalies associated with DiGeorge syndrome. Note the wide-set eyes, low-set ears, and shortened structure of the upper lip. |
Signs and Symptoms
Cardiac
• Aberrant right subclavian artery
• Right aortic arch
• Tetralogy of Fallot
• Truncus arteriosus
• Type B aortic arch interruption
Facial
• Bulbous nose with square tip
• Choanal atresia
• Cleft lip (rare)
• Cleft palate
• Downward slanting eyes
• Hypernasal voice
• Hypertelorism
• Low-set ears with deficient vertical diameter
• Micrognathia
• Short philtrum
• Small mouth
• Telecanthus with short palpebral fissures
• Upward slanting eyes
GastrointestinaI
• Esophageal atresia
• Imperforate anus
• Intestinal malrotation
• Tracheoesophageal (TE) fistula
Genitourinary
• Renal cystic dysplasia
• Ureterohydronephrosis
Immunologic
• Frequent infections
• Immunodeficiencies
Intellectual/Psychiatric
• Affective disorders
• Major depressive disorders
• Mental retardation
• Mild-to-moderate learning difficulties
• Paranoid schizophrenia
Nervous System
• Holoprosencephaly
• Hydrocephalus
• Meningocele
• Neural crest disturbances
Skeletal
• Short stature
Medical Management
DiGeorge syndrome is characterized by hypoparathyroidism and hypocalcemia. Both of these can be effectively treated by administration of calcium supplements as well as vitamin D.
The hypoplastic or aplastic thymus results in immunodeficiency. The deficiencies in T-cells and/or B-cells may be treated with standard prophylactic regimens. Early thymus transplantation may hasten recovery of immune function.
There are numerous clinical features of DiGeorge syndrome (see Signs and Symptoms). Many of these associated features can be rectified surgically, particularly the cardiac anomalies, such as tetralogy of Fallot or truncus arteriosus.
Complications
• Cardiac dysrhythmias secondary to hypocalcemia
• Immunodeficiency
• Recurrent infections
Anesthesia Implications
Securing the airway of the patient with DiGeorge syndrome may be difficult. The patient typically has micrognathia and a small mouth, both of which contribute to making direct laryngoscopy difficult. Direct glottis visualization may prove impossible. It may be necessary to use the laryngeal mask airway (LMA) where appropriate for the proposed surgical procedure. For more complex surgical procedures, the intubating LMA may be required. It may be necessary to use the fiberoptic bronchoscope for intubating purposes. Because the patient may have choanal atresia, the nasal route for intubation may not be available, leaving only the oral route for intubation purposes. The difficult airway cart must be immediately at hand, and a surgeon should be available to surgically secure the airway if necessary.
The hypocalcemia associated with DiGeorge syndrome can affect the delivery of anesthesia. The patient’s response to neuromuscular blocking drugs may be significantly altered. Acute hypocalcemia secondary to hypoparathyroidism can contribute to hemodynamic instability. Hypocalcemia may be exacerbated by hyperventilation and the resultant respiratory alkalosis. The worsening hypocalcemia may further affect response to neuromuscular blockade.
The patient with DiGeorge syndrome is prone to develop infections because the hypoplastic or aplastic thymus gland suppresses cell-mediated immunity.
Hypocalcemia can delay ventricular repolarization, resulting in a prolonged Q-T interval. As a result, the patient may develop a 2:1 heart block. Hypocalcemia may culminate in seizures, which can be exacerbated by the administration of anticonvulsants.







