W1 Difficult Airway Management for Intensivists
 Supraglottic Airway Placement: Before Procedure
Supraglottic Airway Placement: Before Procedure
Indications
Equipment
 After Procedure
After Procedure
Suggested Reading
 Bougie-Assisted Intubation: Before Procedure
Bougie-Assisted Intubation: Before Procedure
Indications
Equipment
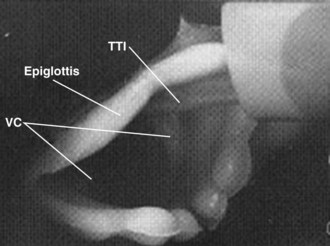
 Anatomy
Anatomy
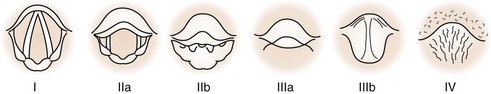
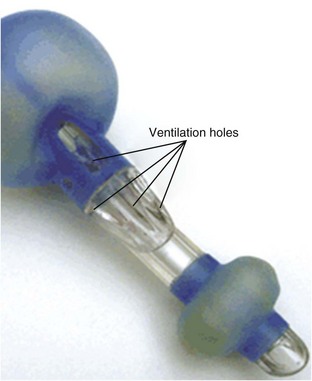
Though the bougie is capable of assisting intubation in nearly all airway situations except when “no view” is possible, it is most commonly used as an adjunct with Grade IIb, IIIa, and IIIb laryngeal views. Even when the laryngoscopy reveals a full view (grade I), the bougie may be useful when the hypopharyngeal opening is narrow (OSA, obesity, swelling) and passing the ETT may actually obstruct the view of the glottic opening. In this case, the narrower, more colorful tracheal tube introducer can be passed into the trachea with little visual obstruction taking place. Conversely, the floppy epiglottis is a challenge that may be technically difficult with many different airway adjuncts. The bougie may either be used to elevate the floppy epiglottis or be maneuvered around by virtue of the Coude tip. Though useful, the success rate is often less than 50%, and other alternatives may be needed (intubating laryngeal mask airway [ILMA], videolaryngoscope [VL], fiberoptic bronchoscope [FOB]) (Figure W1-7).
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
Complications
Suggested Reading
 Use of the Intubating Model of the LMA for Emergency Airway Rescue (Fastrach) ILMA: Before Procedure
Use of the Intubating Model of the LMA for Emergency Airway Rescue (Fastrach) ILMA: Before Procedure
 Anatomy
Anatomy
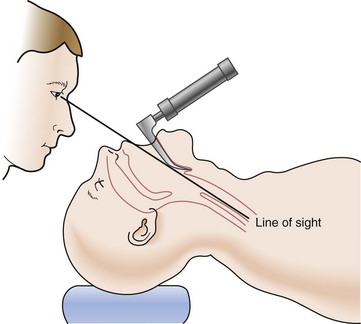
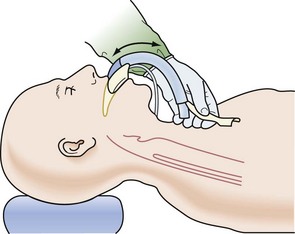
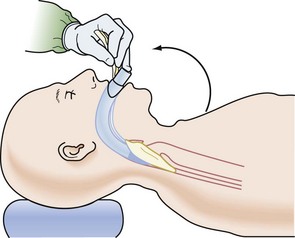
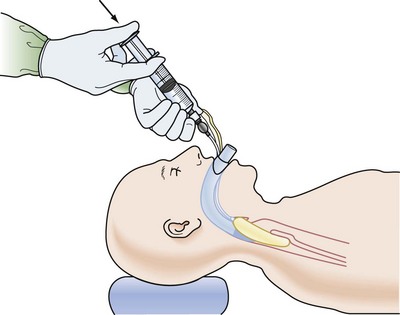
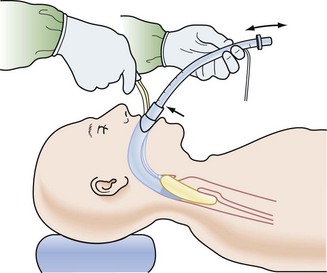
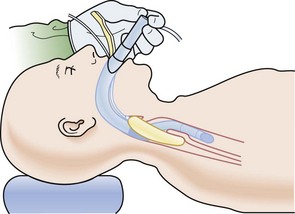
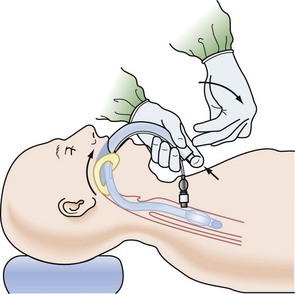
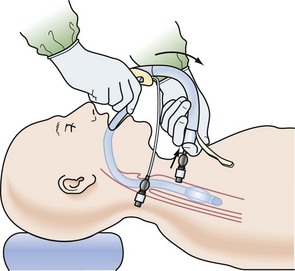
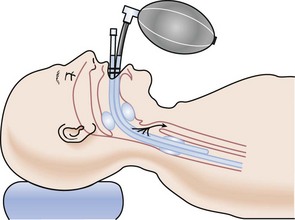
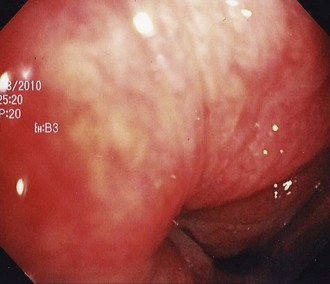
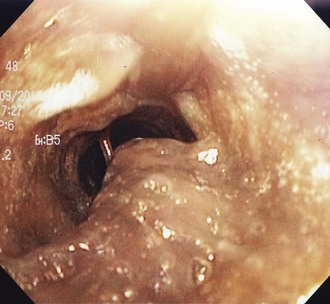
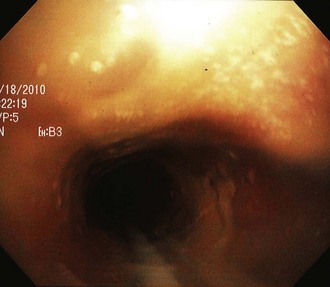
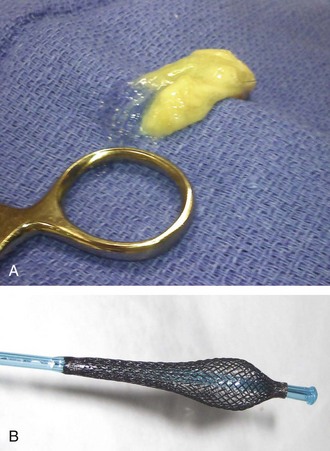
In general, placement of the ILMA can be performed in the exaggerated “sniff” position or the other extreme, a neutral cervical spine. The ILMA is lubricated and then passed along the roof of the mouth across the hard to soft palate, encouraging smooth advancement along the posterior throat so as to minimize getting hung up on the epiglottis or causing its downfolding. The distal tip of the ILMA typically comes to lie with its distal tip in the cricopharyngeal region. Unfortunately, the cuff end may buckle over on itself, come to lie over the glottic opening, or be displaced in a contorted position that impedes effective ventilation and oxygenation (Figures W1-9 through W1-16).
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
 Outcomes and Evidence
Outcomes and Evidence
Suggested Reading
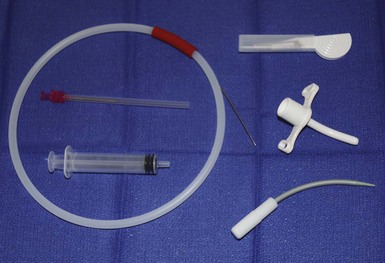
 Retrograde Wire Intubation: Before Procedure
Retrograde Wire Intubation: Before Procedure
Indications
 Anatomy
Anatomy
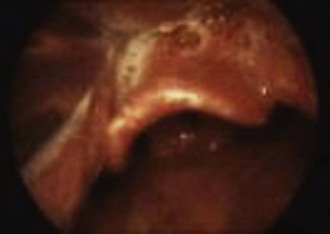
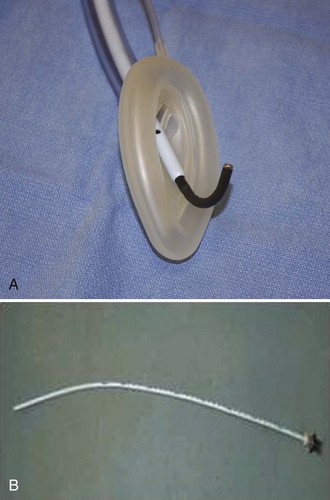
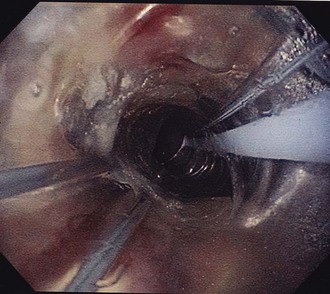
The cricothyroid membrane is located between the superior thyroid cartilage and the inferior cricoid ring. The cricothyroid membrane is located just 1.5 to 2 cm below the vocal cords, so care must be practiced when advancing a needle caudad, as the underside of the vocal cords could be impaled. Passing the ETT over the wire or obturator/wire may be met with resistance at the 16- to 17-cm depth, as the ETT tip may impinge on the vocal cords or arytenoids. This is the inherent danger of passing the ETT blindly over the wire or obturator/wire assembly. The location of the distal tip (having met resistance) may or may not be at the position below the vocal cords. This is the challenge of the retrograde wire method; knowing the location of the ETT tip is unknown when the decision is made to remove the wire. If the ETT tip is erroneously positioned above the glottis, then the access to the airway is denied with wire removal; hence, the advantage of using the FOB as an intubation guide (Figure W1-17).
 Procedure
Procedure
 After Procedure
After Procedure
Suggested Reading
 Needle Cricothyrotomy with Transtracheal Jet Ventilation: Before Procedure
Needle Cricothyrotomy with Transtracheal Jet Ventilation: Before Procedure
Indications
Contraindications
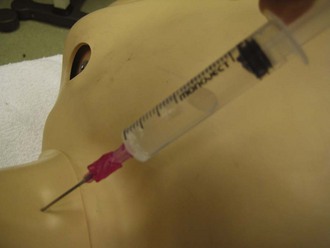
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
 Outcomes and Evidence
Outcomes and Evidence
Suggested Reading
 Needle and Surgical Cricothyrotomy: Before Procedure
Needle and Surgical Cricothyrotomy: Before Procedure
Indications
Contraindications
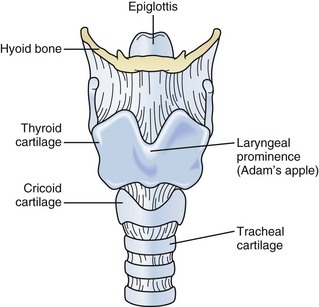
 Anatomy
Anatomy
The thyroid cartilage consists of two approximately quadrilateral-shaped laminae of hyaline cartilage that fuse anteriorly to form the laryngeal prominence. The anterior superior edge of the thyroid cartilage, the laryngeal prominence, is known as the Adam’s apple and is usually easily seen in men. It is probably the most important landmark in the neck when performing a cricothyrotomy. The cricoid cartilage is shaped like a signet ring with the shield located posteriorly and forms the inferior border of the cricothyroid membrane. The thyroid cartilage forms the superior border of the cricothyroid membrane (Figure W1-27).
 Procedure: Conventional Approach
Procedure: Conventional Approach
 Procedure: Stylet-Dilator Method
Procedure: Stylet-Dilator Method
 Procedure: Seldinger Technique–Melker Cook Critical Care
Procedure: Seldinger Technique–Melker Cook Critical Care
 Procedure: Surgical Approach–Rapid Four-Step or Modified Three-Step
Procedure: Surgical Approach–Rapid Four-Step or Modified Three-Step
 After Procedure
After Procedure
Postprocedure Care
 Outcomes and Evidence
Outcomes and Evidence
Suggested Reading
 Esophageal-Tracheal Combitube: Before Procedure
Esophageal-Tracheal Combitube: Before Procedure
Contraindications
Equipment
 Procedure: Combitube
Procedure: Combitube
 Procedure: King Laryngeal Tube
Procedure: King Laryngeal Tube
 After Procedure
After Procedure
Postprocedure Care
Suggested Reading
 Evaluation of a Cuff Leak in the ICU: Before Procedure
Evaluation of a Cuff Leak in the ICU: Before Procedure
Indications
Contraindications
 Procedure
Procedure
Suggested Reading
 Extubation of the Difficult Airway: Before Procedure
Extubation of the Difficult Airway: Before Procedure
Indications
Contraindications
 Anatomy
Anatomy
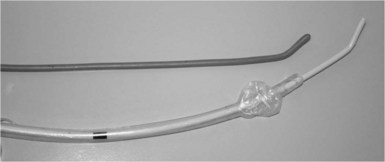
 Procedure
Procedure
TABLE W1-1 Time Frame* for Maintaining the Well-Tolerated Airway Exchange Catheter
| Difficult airway only, no respiratory issues or airway swelling | 1-4 hours |
| Difficult airway, no direct respiratory issues, potential for airway swelling | 2-6 hours |
| Difficult airway, cardiopulmonary issues, multiple extubation failures | 2-24 hours |
* Time frame will vary according to patient condition, airway assessment, and tolerance of the presence of the airway exchange catheter.
 After Procedure
After Procedure
Postprocedure Care
Suggested Reading
 Videolaryngoscope-Assisted Intubation: Before Procedure
Videolaryngoscope-Assisted Intubation: Before Procedure
Indications
Videolaryngoscopy (VL)
Equipment
(Figures W1-43 through W1-50)
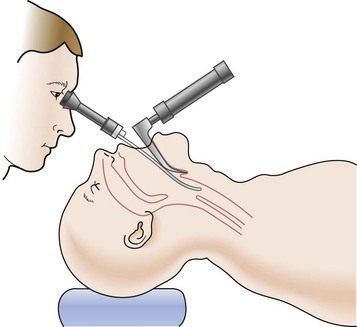
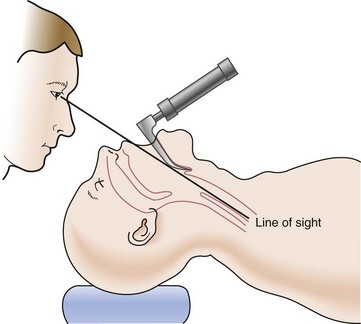
Figure W1-48 Combining direct laryngoscopy with the optical stylet to achieve laryngeal visualization.

Figure W1-50 Same patient as Figure W1-49 but with video-laryngoscope-assisted view, allowing operator full view of epiglottis, arytenoids, and glottic opening.
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
 Outcomes and Evidence
Outcomes and Evidence
Phillips SS, Celenza A. Comparison of the Pentax AWS videolaryngoscope with the Macintosh laryngoscope in simulated difficult airway intubations by emergency physicians. Am J Emerg Med. 2010 Oct 13. Epub
Corso RM, Piraccini E, Terzitta M, et al. The use of Airtraq videolaryngoscope for endotracheal intubation in Intensive Care Unit. Minerva Anestesiol. 2010 Jul 1. Epub
Noppens RR, Möbus S, Heid F, et al. Evaluation of the McGrath Series 5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia. 2010 Jul;65(7):716-720.
Hirabayashi Y, Fujita A, Seo N, et al. Distortion of anterior airway anatomy during laryngoscopy with the GlideScope videolaryngoscope. J Anesth. 2010 Jun;24(3):366-372.
Xue FS, Xiong J, Yuan YJ, et al. Pentax-AWS videolaryngoscope for awake nasotracheal intubation in patients with a difficult airway. Br J Anaesth. 2010 Apr;104(4):505.
Hirabayashi Y, Otsuka Y, Seo N. GlideScope videolaryngoscope reduces the incidence of erroneous esophageal intubation by novice laryngoscopists. J Anesth. 2010 Apr;24(2):303-305.
Uslu B, Damgaard Nielsen R, Kristensen BB. McGrath videolaryngoscope for awake tracheal intubation in a patient with severe ankylosing spondylitis. Br J Anaesth. 2010 Jan;104(1):118-119.
Cavus E Cavus E, Kieckhaefer J, Doerges V, et al. The C-MAC videolaryngoscope: first experiences with a new device for videolaryngoscopy-guided intubation.
Walker L, Brampton W, Halai M, et al. A randomized controlled trial of intubation with the McGrath Series 5 videolaryngoscope by inexperienced anaesthetists. Br J Anaesth. 2009 Sep;103(3):440-445.
Thong SY, Shridhar IU, Beevee S. Evaluation of the airway in awake subjects with the McGrath videolaryngoscope. Anaesth Intensive Care. 2009 May;37(3):497-498.
Stroumpoulis K, Pagoulatou A, Violari M, et al. Videolaryngoscopy in the management of the difficult airway: a comparison with the Macintosh blade. Eur J Anaesthesiol. 2009 Mar;26(3):218-222.
Komatsu R, Kamata K, Hoshi I, et al. Airway scope and gum elastic bougie with Macintosh laryngoscope for tracheal intubation in patients with simulated restricted neck mobility. Br J Anaesth. 2008 Dec;101(6):863-869.
Lim HC, Goh SH. Utilization of a GlideScope videolaryngoscope for orotracheal intubations in different emergency airway management settings. Eur J Emerg Med. 2009 Apr;16(2):68-73.
Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007 Jan;54(1):54-57.
Cooper RM, Pacey JA, Bishop MJ, et al. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005 Feb;52(2):191-198.
Mort TC. Tracheal tube exchange: feasibility of continuous glottic viewing with advanced laryngoscopy assistance. Anesth Analg. 2009 Apr;108(4):1228-1231.
* Relative contraindications may be overlooked in the emergency situation.
* Relative contraindications may be overlooked in the true emergency situation, because it is more important to obtain an airway and avoid hypoxemia.
* Relative contraindications may be overlooked in the true emergency situation, because it is more important to obtain an airway and avoid hypoxemia.
* Based on personal preference, experience, the patient’s clinical condition.