Diarrhea and Constipation
Traveler’s Diarrhea
Etiology
Diarrheal disease in travelers may be caused by a variety of bacterial, viral, and parasitic organisms, which are most often transmitted by food and water. Bacteria account for 50% to 80% of TD in developing countries; the most common organism is enterotoxigenic Escherichia coli, followed by Salmonella species, Campylobacter jejuni, and Shigella species (Table 44-1).
Table 44-1
Major Pathogens in Traveler’s Diarrhea (Travel to Developing Tropical Regions)
| AGENT | FREQUENCY (%) |
| Bacteria | 50-80 |
| Enterotoxigenic Escherichia coli | 5-50 |
| Enteroaggregative E. coli | 5-30 |
| Salmonella species | 1-15 |
| Shigella species | 1-15 |
| Campylobacter jejuni | 1-30 |
| Aeromonas species | 0-10 |
| Plesiomonas shigelloides | 0-5 |
| Other | 0-5 |
| Viruses | 0-20 |
| Rotavirus | 0-20 |
| Norovirus | 1-20 |
| Protozoa | 1-5 |
| Giardia lamblia | 0-5 |
| Entamoeba histolytica | 0-5 |
| Cryptosporidium parvum | 0-5 |
| Unknown | 10-40 |
Signs and Symptoms
1. Acute diarrhea can be accompanied by nausea, loss of appetite, abdominal cramps, low-grade fever, and malaise (Table 44-2).
Table 44-2
Pathophysiologic Syndromes in Diarrheal Disease
| SYNDROME | AGENT |
| Acute watery diarrhea | Any agent, especially with toxin-mediated diseases (e.g., enterotoxigenic Escherichia coli, Vibrio cholerae) |
| Febrile dysentery | Shigella, Campylobacter jejuni, Salmonella, enteroinvasive E. coli, Aeromonas species, Vibrio species, Yersinia enterocolitica, Entamoeba histolytica, inflammatory bowel disease |
| Vomiting (as predominant symptom) | Viral agents, preformed toxins of Staphylococcus aureus or Bacillus cereus |
| Persistent diarrhea (>14 days) | Protozoa, small bowel bacterial overgrowth, inflammatory or invasive enteropathogens (Shigella, enteroaggregative E. coli) |
| Chronic diarrhea (>30 days) | Small-bowel injury, inflammatory bowel disease, irritable bowel syndrome (postinfectious), Brainerd diarrhea |
2. Symptoms begin as early as 8 to 12 hours after contaminated food or water has been ingested.
3. Dysentery (i.e., invasive disease) is present in 10% to 15% of cases, particularly associated with Shigella, C. jejuni, or Salmonella.
4. Dehydration (manifestations include tachycardia, orthostatic vital signs, dry mucous membranes, dark yellow urine and decreased urine output, lethargy, poor skin turgor) may be present and is most common in pediatric and geriatric populations.
5. Vomiting as the predominant symptom suggests food intoxication secondary to enterotoxin produced by Staphylococcus aureus, Bacillus cereus, or Clostridium perfringens, or gastroenteritis secondary to viruses, such as rotavirus in infants or norovirus in any age-group.
6. An abdominal examination of persons with TD often shows mild tenderness, but there should not be signs of peritonitis.
7. With persistent diarrhea (longer than 14 days’ duration), consider possible infection with intestinal parasites such as Giardia lamblia, Entamoeba histolytica, Cryptosporidium, Isospora, Cyclospora, or less common entities including the following:
a. Pseudomembranous enterocolitis (Clostridium difficile) after recent antibiotic use or spontaneously
b. Lactase deficiency induced by small-bowel pathogens
c. Viral enteropathogens such as rotavirus or Norwalk virus
d. Small-bowel bacterial overgrowth syndrome
e. Strongyloides stercoralis or Trichuris trichiura
Treatment (Tables 44-3 and 44-4)
Table 44-3
Nonspecific Drugs for Symptomatic Therapy in Adults
| AGENT | THERAPEUTIC DOSE |
| Attapulgite | 3 g initially, then 3 g after each loose stool or every 2 hr (not to exceed 9 g/day); should be safe during pregnancy and childhood. (available in 600-mg tablets or liquid 600 mg/tsp) |
| Loperamide | 4 mg initially; this is usually sufficient. If nonresponsive, can give 2 mg (one capsule) after each loose stool not to exceed 8 mg (four capsules)/day; do not use in dysenteric or febrile diarrhea |
| Bismuth subsalicylate | 30 mL or two 262-mg tablets every 30 min for eight doses; may repeat on day 2 |
| Probiotics | Dose according to package, because products and formulations vary. Daily dose may make diarrhea less severe and shorten its duration; consider in postinfectious or postantibiotic diarrhea |
Table 44-4
Oral Agents for Self-Treatment of Traveler’s Diarrhea
| AGENT | ADULT DOSE | PEDIATRIC DOSE* |
| Norfloxacin | 400 mg bid for up to 3 days | Not recommended |
| Ciprofloxacin† | 500 mg bid for up to 3 days | 20 to 30 mg/kg/day in two divided doses for up to 3 days; maximum dose 500 mg |
| Ofloxacin† | 200 mg bid for up to 3 days | 7.5 mg/kg q12h for up to 3 days; maximum dose 200 mg |
| Levofloxacin† | 500 mg once daily for up to 3 days | 10 mg/kg once daily for up to 3 days; maximum dose 500 mg |
| Azithromycin‡ | 1000 mg single dose | 10 mg/kg once daily (single dose); maximum dose 1000 mg |
| Rifaximin | 200 mg tid for up to 3 days | ≥12 years: 200 mg tid for up to 3 days |
bid, Twice a day; tid, three times a day.
*Self-treatment of traveler’s diarrhea in children is controversial.
†Not licensed for this indication in children younger than 18 years.
‡Preferred agent for children.
Courtesy UpToDate.
1. TD typically runs a self-limited course of less than 1 week. Although recovery without antimicrobial treatment normally occurs in healthy adults, most travelers choose to avoid the inconvenience and discomfort of diarrhea by seeking medical treatment.
2. Severe, watery TD can cause life-threatening fluid loss. Treating serious dehydration is an urgent priority, especially in older persons, young children, and infants. Fluid replacement is the cornerstone of therapy.
a. Treating dehydration often significantly decreases malaise.
b. Urine volume (decreased urine output for an adult is less than 500 mL in a 24-hour period) and color (one field indicator of dehydration is dark-yellow urine) can serve as markers of adequate hydration and should be monitored.
c. If patients are otherwise healthy and not dehydrated, adequate oral intake can be achieved with soft drinks, fruit juice, broth, and soup, along with salted crackers. In those with excessive fluid losses and dehydration, oral rehydration therapy with electrolyte solutions containing glucose should be instituted. Reduced osmolarity (245 mOsm/L compared with the previous 311 mOsm/L) oral rehydration solutions (ORSs) are now recommended by the World Health Organization (WHO) for treating acute diarrhea (Table 44-5). The lower osmolarity reduces stool output (volume), vomiting, and the need for intravenous (IV) therapy. Rehydration Project is a nonprofit, international development group that maintains an up-to-date website on rehydration options (http://rehydrate.org/ors/low-osmolarity-ors.htm).
Table 44-5
Reduced Osmolarity Oral Rehydration Solution
| REDUCED OSMOLARITY ORS | mmol/L |
| Sodium | 75 |
| Chloride | 65 |
| Glucose, anhydrous | 75 |
| Potassium | 20 |
| Citrate | 10 |
| Total Osmolarity | 245 |
• Add one packet of ORS to 1 L (1 qt) of clean drinking or boiled water (after cooled). Many pharmacies or clinics may still stock the “old” WHO 1975 formula. It can be used to make a lower osmolarity solution that still meets new WHO parameters by mixing it in 1.2 L (1.2 qt) of water rather than in 1 L.
• Sports drinks such as Gatorade also provide adequate fluid replacement if diluted to about to about one-half their strength (add 0.5 L [0.5 qt] of water to 1 L [1 qt] of Gatorade). Full-strength sports drinks are often more hypertonic than 245 mOsm/L (the osmolality of Gatorade is approximately 360 mOsm/L) and may delay gastric absorption.
• A number of other ORSs are also available for children, including Pedialyte, Rehydralyte, Ricelyte, Infalyte, and Resol.
3. To make an improvised ORS, one of the following methods can be used:
a. Add 30 mL (6 tsp) of sugar and 2.5 mL ( tsp) of salt to 1 L (1 qt) of clean drinking water (or boiled water that has cooled).
tsp) of salt to 1 L (1 qt) of clean drinking water (or boiled water that has cooled).
b. Add 2.5 mL ( tsp) salt, 5 mL (1 tsp) baking soda, 40 mL (8 tsp) sugar, and 236 mL (8 oz) orange juice, diluted to 1 L (1 qt) with water.
tsp) salt, 5 mL (1 tsp) baking soda, 40 mL (8 tsp) sugar, and 236 mL (8 oz) orange juice, diluted to 1 L (1 qt) with water.
4. Fluids should be given at rates of 50 to 200 mL/kg/24 hr, depending on the patient’s hydration status.
5. Treatment with IV fluids is indicated for patients with severe dehydration and for those who cannot tolerate oral fluids.
6. Total food abstinence is unnecessary and not recommended. Patients should be encouraged to eat easily digested foods such as bananas, applesauce, rice, potatoes, noodles, crackers, toast, and soups. Dairy products should be avoided, because transient lactase deficiency can be caused by enteric infections. Caffeinated beverages and alcohol, which can enhance intestinal motility and secretions, should be avoided.
Symptomatic Therapy
Symptomatic medications are useful for treatment of diarrhea because they decrease symptoms and fluid loss and allow patients to return more quickly to normal activities (see Table 44-3).
a. Narcotic analogs related to opiates are the major antimotility drugs. In addition to slowing intestinal motility, these drugs alter water and electrolyte transport, probably affecting both secretion and absorption. Use over-the-counter agent loperamide (Imodium) or prescription agent diphenoxylate plus atropine (Lomotil) to offer relief to patients with watery diarrhea and cramps. Of the two drugs, loperamide is better tolerated and has fewer central opiate effects.
b. The adult dose for loperamide is 4 mg for the initial dose and 2 mg after every loose stool, up to a total dose of 8 mg/day
c. These drugs can be valuable for long bus rides or summit bids where social constraints make frequent rest stops impractical.
d. Antimotility drugs can be important for controlling fluid balance in a patient with profuse diarrhea who is unable to tolerate sufficient oral fluids to maintain a positive fluid balance.
e. Avoid antimotility drugs alone (i.e., without antibiotics) if blood or mucus is present in the stool or if patient has signs of serious illness (high fever, recurrent vomiting, severe abdominal pain) because the inhibition of gut motility may facilitate intestinal infection by invasive bacterial enteropathogens. This theoretically deleterious effect does not appear to be an issue when loperamide is used concurrently with an effective antimicrobial agent.
f. Antimotility drugs should be used only up to a maximum of 48 hours in acute diarrhea.
2. Bismuth subsalicylate (BSS; Pepto-Bismol) reduces the number of stools passed in TD by approximately 16% to 18%. Although BSS is recommended for mild diarrhea, for moderate to severe disease, loperamide works better and with a faster onset of action.
3. Probiotics appear to reduce stool frequency and shorten the duration of acute infectious diarrhea by 1 day. The most extensively studied probiotics for diarrhea are Lactobacillus, Bifidobacterium, and Saccharomyces; however, optimal species and dosing have not been established. Potential mechanisms for their therapeutic action include protection of intestinal epithelial cells and barrier function, prevention of enterotoxin binding to intestinal epithelial cells, and regulation of intestinal microbial environment.
Antimicrobial Therapy
1. TD can be relieved in a little over 1 day after empiric antibiotic therapy is instituted. With the concurrent use of loperamide, relief is realized in a matter of hours. With reports of increasing resistance among enteric enteropathogens worldwide, trimethoprim/sulfamethoxazole can no longer be recommended. Until recently, one of the fluoroquinolones had been the drug of choice for empiric treatment of TD. With recognition that C. jejuni is a common cause of traveler’s diarrhea in Southeast Asia and that there is emerging resistance (up to 90%) to fluoroquinolones for Campylobacter in this region, the preferred agent for the empiric treatment of TD has become azithromycin for countries such as Thailand and India. Rifaximin, a nonabsorbed agent with broad activity against enteric pathogens, is effective in the treatment of TD in regions of the world where enterotoxigenic E. coli is the predominate pathogen. It is not recommended for treatment of bloody diarrhea or when an invasive pathogen is suspected, limiting its usefulness as a therapeutic agent in regions like Southeast Asia. However, because rifaximin can prevent diarrhea, including that caused by invasive pathogens, the most appropriate use of rifaximin might be as a chemoprophylactic agent. Recommended dosages of antimicrobial agents are shown in Table 44-4. Often a single dose suffices. Travelers who do not respond to empiric antibiotic treatment or who have persistent diarrhea of more than 1 week’s duration should seek medical attention. In the wilderness, Giardia can be an important cause of ongoing diarrhea unresponsive to antibiotics (see later).
2. Travelers with severe and incapacitating symptoms, or with dysentery, should be treated with empiric antimicrobial therapy immediately after the first passage of unformed stool.
3. Additional considerations follow:
a. Azithromycin is an effective antibiotic for the treatment of TD and is the preferred agent for children. Azithromycin administered as a single 1-g oral dose has as high a cure rate as does 500 mg/day for 3 days.
b. Loperamide 4 mg should be administered concomitant with an antibiotic.
c. If the patient has begun initial treatment of diarrhea with BSS therapy, at least 8 hours must elapse before optimum antibiotic therapy can occur because BSS impairs absorption of oral antimicrobial agents.
d. Advise any patient who does not respond to empiric antibiotic treatment or who has diarrhea for more than 1 week to obtain clinical follow-up that includes a complete workup for bacterial and parasitic pathogens.
Prevention
1. Take dietary precautions. The risk for illness is lowest when a traveler’s meals are self-prepared in a private home, highest when food is obtained from street vendors, and intermediate when food is consumed at public restaurants. Unfortunately, many studies evaluating risk have found little correlation between routine precautions and illness. Dietary recommendations to decrease the potential for transmission of fecal pathogens through food and water are as follows:
a. Avoid tap water and ice made from untreated water (most enteric organisms can survive freezing).
b. Bottled noncarbonated water may be contaminated with fecal coliforms.
c. Bottled and carbonated drinks, beer, and wine are probably safe.
d. Boiled or chemically disinfected water is safe.
e. Alcohol in mixed drinks does not disinfect.
f. Homemade beverages may not be safe.
g. Ice in block form is often handled with unsanitary methods.
h. Avoid unpasteurized cheese and dairy products.
i. Avoid raw vegetables and salads, which may be contaminated by fertilization with human waste or washing with contaminated water.
j. Anything that can be peeled or have the surface removed is generally safe.
k. Fruits and hearty vegetables can be disinfected by immersion and washing in iodinated water or by exposure to boiling water for 30 seconds.
l. Avoid raw seafood and fish.
m. Avoid raw meat because adequate cooking kills all microorganisms and parasites. If the meat is left at room temperature and recontaminated, cooked food can incubate pathogenic bacteria. Casseroles are notorious for reheating and contamination.
n. Avoid eating foods upon which you have observed many flies to be resting.
2. Use of prophylactic medications to prevent TD
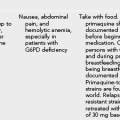
a. Of the nonantibiotic drugs, only BSS has been shown by controlled studies to offer reasonable protection and safety. The current recommended dose of BSS (for prevention) is 2 tablets 4 times per day. Mild side effects include constipation, nausea, and blackened tongue or stools. BSS taken concurrently with antibiotics should be avoided because of the potential binding of BSS to the antibiotic, which prevents absorption.
b. Do not give BSS to someone with a history of aspirin allergy.
c. Give BSS with caution to small children; people with gout or renal insufficiency; and those taking probenecid, methotrexate, anticoagulants, or products containing aspirin.
3. Antimicrobial prophylaxis for TD
a. A broad-spectrum antibiotic taken during travel can effectively prevent illness, but resolution of TD within a few hours can usually be obtained after oral antibiotic therapy with an appropriate antibiotic. It is probably unnecessary for the average traveler to ingest an antibiotic for the full duration of a trip.
b. Antimicrobial prophylaxis of TD might be a reasonable strategy for residents of a low-risk country going to a high-risk area for fewer than 5 weeks with one or more of the following:
• Underlying illness such as acquired immunodeficiency syndrome (AIDS); inflammatory bowel disease; or a cardiac, renal, or central nervous system disorder
• An itinerary that is so rigid and critical that a person cannot tolerate any inconvenience caused by TD; such travelers include competitive athletes, politicians, sales representatives, and people going to special events
c. For specific antibiotic therapy recommended to prevent TD see Table 44-6.
Table 44-6
Prophylactic Medications for Prevention of Traveler’s Diarrhea*
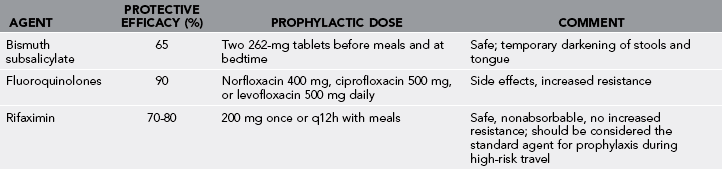
*Not generally recommended for travelers; used only in special situations (see text) and for no longer than 3 weeks.
d. Despite its protection against diarrhea, the routine use of antimicrobial prophylaxis by travelers is not recommended because of the following:
Food Poisoning
Infection Caused by Intestinal Protozoa
Giardia lamblia
Signs and Symptoms
1. The severity of clinical manifestations is variable. In general, about half of exposed individuals clear the infection without clinical symptoms, and approximately 5% to 15% of individuals shed cysts asymptomatically
2. Average incubation period of 7 to 14 days (range 1 to 45 days)
3. Sometimes abrupt onset of explosive, watery diarrhea accompanied by abdominal cramps, foul flatus, vomiting, fever, and malaise; typically lasts 3 to 4 days before transition to subacute syndrome
4. Onset usually insidious, with symptoms that wax and wane
5. Stools becoming mushy and malodorous
6. Watery diarrhea alternating with soft stools and even constipation
7. Middle and upper abdominal cramping, substantial burning acid indigestion, sulfurous belching, nausea, bowel distention, early satiety, foul flatus
8. Dysenteric symptoms (blood and pus in the stool) are not features of giardiasis; fever and vomiting are infrequent except during initial onset.
9. May develop into a chronic process associated with malabsorption and weight loss
Treatment
1. Treatment in the wilderness is usually initiated empirically based on the typical manifestations listed earlier.
2. Note that a cure can be achieved with one of several drugs. However, no drug is effective in all cases. In resistant cases, longer courses of two drugs taken concurrently may be effective.
3. Relapse may occur up to several weeks after treatment, which requires a second course of the same medication or an alternative drug.
4. Three antimicrobial drugs are currently recommended: tinidazole, metronidazole, and nitazoxanide.
5. Tinidazole (2000 mg adult dose; 50 mg/kg for children in a single dose) is highly effective and approved by the Food and Drug Administration (FDA) for treatment of giardiasis in persons older than 3 years. It should be taken with food. Tinidazole has a longer half-life than metronidazole and offers the advantage of a single-dose treatment. For those unable to swallow tablets, Tinidazole tablets may be compounded into an oral suspension.
a. Procedure for compounding of the oral suspension of tinidazole (66.7 mg/mL):
• Crush 4 tinidazole 500-mg tablets into a fine powder with a mortar and pestle.
• Add approximately 10 mL of cherry syrup to the powder, and mix until smooth.
• Transfer the suspension to a container using additional cherry syrup (30 mL total).
• The suspension of crushed tablets in cherry syrup is stable for 7 days at room temperature.
6. Metronidazole can be used in children and adults (although giardiasis is not an FDA-approved indication for metronidazole). Adult dose is 250 mg tid for 5 to 7 days, and for children the dose is 15 mg/kg/day. Side effects are common and include nausea, gastrointestinal discomfort, and a metallic taste. Metronidazole may have a disulfiram-like effect, so alcohol consumption should be avoided.
7. Nitazoxanide, a nitrothiazolyl-salicylamide derivative, has been approved by the FDA for the treatment of giardiasis in children older than 1 year. In clinical trials it has been shown to be more effective than metronidazole in relieving symptoms in individuals with giardiasis. In addition, nitazoxanide is effective in treating multiple other infections caused by intestinal parasites (e.g., cryptosporidiosis and amebiasis). Nitazoxanide is available in liquid and tablet form but is expensive, and many pharmacies do not stock it. The recommended oral doses are as follows:
a. Adults: 500 mg q12h for 3 days
b. Children 1 to 3 years: 100 mg q12h for 3 days
8. The nonabsorbable drug paromomycin (Humatin, 25 to 30 mg/kg in three divided doses for 5 to 10 days) has been effective and may be used during pregnancy. When considering treatment during pregnancy, when possible, withhold treatment until after discussing with an obstetrician because none of the treatment options is considered completely safe.
Dysenteric (Invasive) Disease
Signs and Symptoms
1. Dysentery developing suddenly or after a period of mild symptoms
2. Symptoms developing in as few as 8 to 10 days, but more often after weeks to months
3. Ill appearance, with frequent bloody stools, tenesmus, moderate to severe abdominal pain and tenderness, and fever (considerable variation in severity)
5. Complications in 1% to 4% of patients: bowel perforation, toxic megacolon, strictures, or an ameboma (inflammatory lesion containing trophozoites that develops in the colon)
6. Amoebic liver abscess acutely or years after infection
7. In the wilderness, diagnosis considered in any patient with dysentery who is not responding to an appropriate antibiotic
8. Asymptomatic cyst shedding and active gastrointestinal illness that persist for years if amebiasis is not treated
Treatment
1. Invasive colitis is treated with metronidazole (alternative therapies include tinidazole or nitazoxanide), followed by a luminal agent (such as paromomycin, diiodohydroxyquin, or diloxanide furoate) to eliminate entraluminal cysts.
a. Dosing for metronidazole is 500 to 750 mg PO q8h for 7 to 10 days in adults and 35 to 50 mg/kg/day in three divided doses for 7 to 10 days in children.
b. Dosing for tinidazole is 2 g PO daily for 3 days in adults. The dose for children older than 3 years is 50 mg/kg/day for 3 days (maximum dose: 2 g/day).
c. Dosing for nitazoxanide is the same as for giardiasis (see earlier).
d. Dosing for paromomycin is 25 to 30 mg/kg/day PO in three divided doses for 7 days.
e. Dosing for diiodohydroxyquin is 650 mg PO q8h for 20 days for adults and 30 to 40 mg/kg/day in three divided doses for 20 days for children. This drug causes frequent systemic side effects, including cardiac arrhythmias requiring hospitalization for cardiac monitoring. Because this drug is related to ipecac, it may also cause vomiting.
2. In general, treatment is effective for invasive infections but disappointing for luminal infections (no regimen is completely effective in eradicating intestinal infection).
Cryptosporidium
Signs and Symptoms
1. Incubation period usually 7 to 10 days (range 3 to 28 days)
2. Syndrome generally mild and self-limited (typical duration of 5 to 6 days, range 2 to 26 days)
3. Asymptomatic infection may occur
4. Watery diarrhea (without blood or pus); abdominal cramps; nausea; flatulence; and, at times, vomiting and low-grade fever
5. Immunocompromised hosts experience more frequent and prolonged infections, with profuse chronic watery diarrhea, malabsorption, and weight loss lasting months to years.
6. Definitive diagnosis by stool examination or serologic techniques
Treatment
1. Recovery from infection depends upon the immune status of the patient. Immunocompetent patients usually recover without treatment within 1 to 2 weeks while receiving supportive therapy for vomiting and dehydration.
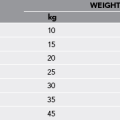
2. When therapy is required, nitazoxanide is the preferred drug. The adult dose is 500 mg q12h for 3 days. Dosing for children is as follows:
Cyclospora Cayetanensis
Treatment
1. Cyclospora resists halogen-based (e.g., iodine and chlorine) water disinfection methods.
2. It is best killed by bringing drinking water to a boil.
3. The treatment of choice is trimethoprim/sulfamethoxazole; adult dose is one double-strength 160 mg/800 mg tablet PO q12h for 7 to 10 days. Ciprofloxacin 500 mg PO q12h for 7 days may be used as an alternative therapy for patients with a sulfa allergy.
Constipation
Treatment
1. Increase fluid intake (approximately 2 L of fluid daily in adults).
2. Patients should try to drink an extra glass of water for every glass of diuretic beverage (i.e., coffee, tea, or alcohol).
a. It is helpful to bring along bran or psyllium seed (e.g., Metamucil) or methylcellulose (Citrucel) for this purpose.
b. Patients should drink plenty of water; otherwise, ingesting fiber can be counterproductive.
c. Fiber is not a laxative and will not typically induce an immediate bowel movement.
d. Fiber-containing products, such as psyllium or methylcellulose, may cause gas or bloating.
4. Stool softeners such as docusate sodium (Colace 50 to 500 mg/day PO in one to four divided doses) enhance absorption of water and fat into stool, causing stool to soften. These drugs can be helpful, but they often lose their effectiveness over time.
5. At times a stronger stimulant medication may be indicated.
6. Bisacodyl (Dulcolax) is generally safe and effective.
a. Bisacodyl should be taken with a full glass of water.
b. The patient should swallow the tablets or capsules whole (i.e., do not chew or crush them).
7. Bisacodyl is also available as a rectal suppository. To use a rectal suppository, follow these steps:
a. If the suppository is soft (such as in warm weather), insert it (in its wrapping) into cold water for 1 or 2 minutes before use.
b. After removing the wrapper, moisten the suppository with water or petroleum jelly.
c. The patient should lie on his or her side.
d. With the pointed end first, push the suppository into the rectum.
8. Polyethylene glycol 3350 is available as MiraLax. The dose is one heaping teaspoon of this osmotic laxative in at least 236 mL (8 oz) of beverage once a day. It may require 2 to 4 days for the first bowel movement to occur. Because it can be habit forming, it should not be used consecutively for more than 2 weeks.