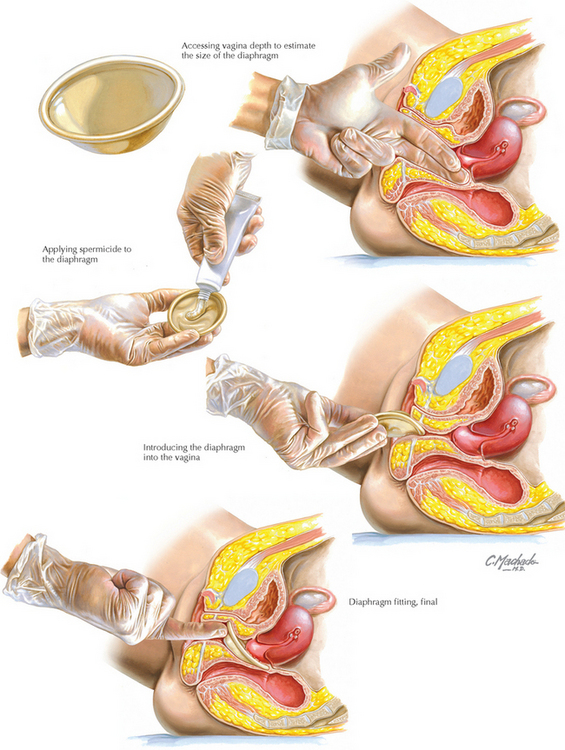
Chapter 241 Diaphragm Fitting
Bounds W, Guillebaud J, Dominik R, Dalberth B. The diaphragm with and without spermicide. A randomized, comparative efficacy trial. J Reprod Med. 1995;40:764.
Cook L, Nanda K, Grimes D. Diaphragm versus diaphragm with spermicides for contraception. Cochrane Database Syst Rev. 2001. CD002031.
Ferreira A, Araújo M, Regina C, et al. Effectiveness of the diaphragm, used continuously, without spermicide. Contraception. 1993;48:29.
Fihn S, Latham R, Roberts P, et al. Association between diaphragm use and urinary tract infection. JAMA. 1985;254:240.
Mauck C, Lai J, Schwartz J, Weiner D. Diaphragms in clinical trials: is clinician fitting necessary? Contraception. 2004;69:263.