Chapter 42
Diabetes and Cardiovascular Disease
1. What is the current global burden of diabetes, and what is its impact on the epidemiology of cardiovascular disease (CVD)?
2. What is the impact of diabetes on CVD outcomes?
3. What effect, if any, does diabetes have on the clinical manifestations and prognosis of peripheral arterial disease (PAD) and cerebrovascular disease?
Diabetes increases the risk of PAD about two- to fourfold. It is more commonly associated with femoral bruits and absent pedal pulses and with a high rate of abnormal ankle-brachial indices, ranging from 11% to 16% in different studies. The duration and severity of diabetes correlates with the incidence and extent of PAD. The pattern of PAD in diabetic patients is characterized by a preponderance of infrapopliteal occlusive disease and vascular calcification. Clinically, PAD in diabetic patients manifests more commonly with claudication and also a higher rate of amputation—the most common cause of nontraumatic amputations.
4. What is the overall impact of diabetes on the vascular tree?
5. What is the burden of additional CV risk factors in diabetic patients, and what is their cumulative impact on the atherosclerosis morphology and burden?
6. What characteristics of the atherosclerotic plaque in diabetic patients make it unstable compared with plaque in nondiabetic patients?
Diabetic patients harbor a proinflammatory and prothrombotic milieu with greater C-reactive protein (CRP), matrix metalloproteinase 3 and 9 (MMP-3 and MMP-9), intercellular adhesion molecule (ICAM), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), monocyte chemotactic protein-1 (MCP-1), plasminogen activator inhibitor-1 (PAI-1), and superoxide concentrations. In addition to its adverse effects on the endothelium, diabetes promotes processes that lead to monocyte transmigration across the endothelium into the vessel wall and uptake of oxidized LDLs into these cells, resulting in foam cell and fatty streak formation. In addition to plaque initiation, diabetes renders the atherosclerotic plaque unstable. Endothelial cells in diabetic patients release cytokines and enzymes (MMPs) that impair collagen synthesis by vascular smooth muscle cells and also accelerate its breakdown. Because collagen is an essential component of the plaque fibrous cap, weakening it renders the plaque unstable. Plaque rupture or erosion triggers an intense local prothrombotic milieu, resulting in thrombus formation. In addition, following plaque rupture, platelets of diabetic patients aggregate more aggressively and are more likely to disaggregate with more efficacious antiplatelet agents (especially prasugrel and ticagrelor, when compared to clopidogrel), as demonstrated in the diabetic cohorts of the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel Thrombolysis in Myocardial Infarction 38 (TRITON-TIMI 38) and Platelet Inhibition and Patient Outcomes (PLATO) trials. Diabetes also results in elevated factor VII levels (procoagulant) and reduced protein C and antithrombin III levels (naturally occurring anticoagulants). Finally, diabetic endothelial cells produce more tissue factor, the major procoagulant found in atherosclerotic plaques.
7. What broad management strategy is advocated for diabetic patients with CVD?
8. How does the treatment of hyperglycemia and insulin resistance impact outcomes in diabetic patients with CVD?
9. What are the currently recommended strategies for the management of diabetic dyslipidemia?
In addition to statins, fibric acid derivatives may be especially beneficial in diabetic patients because of their effects in lowering triglycerides and raising HDL levels. Treatment with gemfibrozil significantly reduced the risk of MI in the Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial (VA-HIT). In addition to the lipid-lowering effect, fibric acid derivatives may have antiatherogenic, antithrombogenic, and antiinflammatory effects. However, the role of fibric acid derivatives has been questioned in diabetic patients recently, following the results of the ACCORD lipid study in which adding a fibrate to a statin did not confer additional CV protection. Nicotinic acid also produces a similar favorable effect on the lipid profile in diabetic patients but needs investigation in a large study, following disappointing results from the Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglycerides: Impact on Global Health Outcomes (AIM-HIGH) trial. In addition, diabetic patients on niacin may require close monitoring of their glucose levels.
10. What do the current guidelines recommend for management of hypertension in diabetic patients?
11. What are the principles of management of chronic CAD in diabetic patients?
Diabetic patients are more likely to experience painless cardiac ischemia and suffer more silent MIs and sudden cardiac death. Evidence from observational studies and randomized trials has shown significant mortality benefit with β-blockers in diabetic patients. β-Blockers are well tolerated in diabetic patients; masking or prolongation of hypoglycemic symptoms is infrequent, particularly with cardioselective agents. Recommendations include continuing antiplatelet therapy; ACE inhibitors and ARBs should be used as appropriate for blood pressure control, and β-blockers are recommended in diabetic patients after an MI. However, routine screening for CAD in diabetic patients is not recommended, as demonstrated in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) trial. The multifaceted approach to the diabetic patient is illustrated in Figure 42-1.
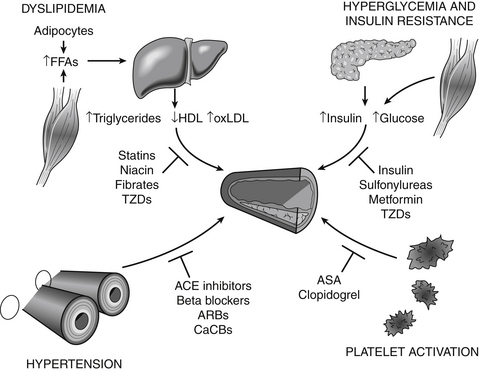
Figure 42-1 Diabetes requires therapy for each metabolic abnormality to stem the onset and progression of atherosclerosis. Statins improve the lipid profile and decrease the risk of MI and death. Treatment of hypertension decreases the rate of myocardial infarction (MI) and stroke in patients with diabetes. Therapy should include angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) for their microvascular and possible atherosclerosis benefits. The heightened thrombotic potential of the diabetic state supports the use of platelet antagonists, such as aspirin or clopidogrel. Although strict treatment of hyperglycemia does not significantly reduce the incidence of MI or death, the improvement in microvascular outcomes itself warrants vigorous pursuit of rigorous glycemic control in diabetes. (Modified from Libby P, Plutzky J: Diabetic macrovascular disease: the glucose paradox? Circulation 106:2760, 2002.) ASA, Aspirin; CaCBs, calcium channel blockers; FFAs, free fatty acids; HDL, high-density lipoprotein; oxLDL, oxidized low-density lipoprotein; TZDs, thiazolidinediones.
12. What strategies for coronary revascularization are currently recommended for the management of multivessel CAD in diabetic patients?
Bibliography, Suggested Readings, and Websites
1. ADVANCE Collaborative Group, Patel, A., MacMahon, S., et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–2572.
2. American Diabetes Association. Standards of medical care in diabetes—2006. Diabetes Care. 2006;29(Suppl 1):S4–S42.
3. Aneja A, Tang WH, Bansilal S, et al: Diabetic cardiomyopathy: insights into pathogenesis, diagnostic challenges, and therapeutic options, Am J Med 121(9):748–757
4. Beckman, J.A., Creager, M.A., Libby, P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–2581.
5. Berry, C., Tardif, J.C., Bourassa, M.G. Coronary heart disease in patients with diabetes. Part I: Recent advances in prevention and noninvasive management. J Am Coll Cardiol. 2007;49:631–642.
6. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet. 2000;355:253–259.
7. Farkouh, M.E., Domanski, M., Sleeper, L.A., et al. FREEDOM Trial Investigators: Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375–2384. Dec 20
8. Gaede, P., Lund-Andersen, H., Parving, H.H., et al. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–591.
9. Gerstein, H.C., Miller, M.E., Byington, R.P., et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–2559.
10. Goldberg, R.B., Mellies, M.J., Sacks, F.M., et al. Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the cholesterol and recurrent events (CARE) trial: the CARE investigators. Circulation. 1998;98:2513–2519.
11. Grundy, S.M., Cleeman, J.I., Merz, C.N., et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732.
12. Gu, K., Cowie, C.C., Harris, M.I. Diabetes and decline in heart disease mortality in US adults. JAMA. 1999;281:1291–1297.
13. Khardori, R. Diabetes mellitus, type 2. Available at http://emedicine.medscape.com/article/117853-overview. Accessed February 27, 2013
14. Malmberg, K., Yusuf, S., Gerstein, H.C., et al. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) registry. Circulation. 2000;102:1014–1019.
15. McCullock DK: Overview of medical care in adults with diabetes mellitus. In Basow, DS, editor: UpToDate, Waltham, MA, 2013, UpToDate. Available at http://www.uptodate.com/contents/overview-of-medical-care-in-adults-with-diabetes-mellitus. Accessed March 26, 2013
16. Nesto RW: Coronary artery revascularization for angina in patients with diabetes mellitus and multivessel coronary artery disease. In Basow, DS, editor: UpToDate, Waltham, MA, 2013, UpToDate. Available at http://www.uptodate.com/contents/coronary-artery-revascularization-in-patients-with-diabetes-mellitus-and-multivessel-coronary-artery-disease. Accessed March 26, 2013
17. Pyorala, K., Pedersen, T.R., Kjekshus, J., et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. Diabetes Care. 1997;20:614–620.
18. Smith, S.C., Jr., Allen, J., Blair, S.N., et al. ACC/AHA guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363–2372.
19. Skyler, J.S., Bergenstal, R., Bonow, R.O., et al. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a Scientific Statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol. 2009;53:298–304.



