CHAPTER 71 Developmental and Functional Anatomy of the Thoracic Spine
The thoracic spine has long been treated as the ugly stepsister of the cervical and lumbar spine. It has received little research or review, mostly because thoracic spinal pain syndromes are relatively uncommon or underdiagnosed. The thoracic spine covers more segments than the cervical and lumbar spine, thus making exhaustive research difficult. In addition, the backdrop of rib articulations to the 12 thoracic spinal segments provides inherent stability to this region. Thus, the thoracic spine pain generators are not as susceptible to mechanical forces. Guidelines for the treatment of thoracic spinal pain are nonexistent and are ripe for research.1 However, to develop reasonable guidelines in a field of spine medicine without much research, a thorough understanding of the anatomy and biomechanics of the thoracic spine is needed.
DEVELOPMENTAL ANATOMY
Neuralization
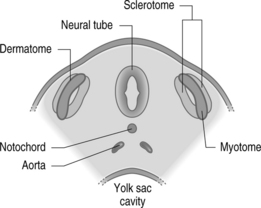
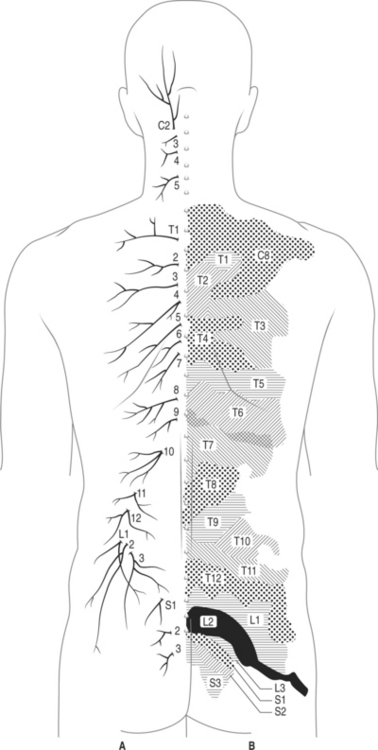
Neural tube development begins with the formation of the notochord around day 20 of embryogenesis. The neural tube will eventually develop into the spinal cord and brain. The surrounding mesoderm condenses to form somites.2 Somite differentiation in the early part of fetal development separates cells into the dermatome, myotome, and sclerotome cells (Fig. 71.1).
Sclerotome
The vertebrae and associated ligaments are formed by the development of sclerotome cells into a segmental centrum which forms cartilage and then the bony vertebral body.2 Primary and secondary ossification centers provide growth areas to turn cartilage into bone. The secondary ossification centers in the annular epiphysis (apophyseal rings) remain open through adolescence. Scheurmann disease or kyphosis may be caused by an insult to these secondary ossification centers. Eventually, Schmorl’s nodes can develop in these individuals with Scheurmann disease such that disc material herniates through the insulted vertebral endplate. Two other posterior primary ossification centers come together to form the neural arch. Rarely, particularly in the setting of poor folate intake, neural arch and tube defects (e.g. spina bifida and hemivertebrae) may arise.
Neural tube
The inferior portion of the neural tube differentiates into ependymal (central), mantle (neurons and glia), and marginal layers (axons of tract cells).2 These eventually form the future spinal cord. The neural crest develops into neurons of the peripheral nervous system.
Postural curves
Developmentally, the in utero spine is flexed so that the fetal position is achieved. However, with age and weight bearing, the primary curve of the spine gives way to secondary curves in the cervical and lumbar spine (i.e. lordosis). The thoracic spine remains with the primary curve and, thus, in kyphosis.3 Normal thoracic kyphosis allows for the anterior height of the thoracic vertebral body to be 1.5–2 cm shorter than the posterior height.3 Scoliosis is common in the thoracic spine region. Some have theorized that idiopathic scoliosis may be partly an embryogenesis problem with inadequate development of the junction between the centrum and the neural arch (i.e. neurocentral synchondrosis).
NEURAL ANATOMY
Thoracic spine pain generators
There have been no comprehensive studies on the innervation schemes of the thoracic spine other than some published descriptions of the dorsal rami of the thoracic spine.4 Innervation schemes must be understood so that pain generators of the thoracic spine can be precisely identified. To date, the thoracic zygapophyseal joints, intervertebral disc, costovertebral joints, and posterior thoracic muscles have been proven to have nerve supply.4 However, other thoracic structures are also likely to be sources of pain (e.g. costotransverse joint, vertebral body) (Table 71.1) In addition, the thoracic spine houses much of the autonomic nervous system of the human body, a well-known modulator of pain syndromes. Ligaments about the thoracic spine, such as the interspinous ligament and posterior longitudinal ligament, may also cause thoracic spine pain.5
| Thoracic zygapophyseal joints |
| Thoracic intervertebral disc |
| Costovertebral joints (e.g. synovitis from ankylosing spondylitis) |
| Posterior thoracic muscles (e.g. trigger points) |
| Costotransverse joint |
| Vertebral body (e.g. compression fractures) |
| Dura mater |
| Epidural blood vessels |
| Posterior longitudinal ligament |
| Sympathetic trunk |
Types of thoracic pain
Thoracic spine pain conditions can be differentiated by the classifying pain into superficial and deep pain (Table 71.2).6 Superficial pain is sharp pain that is fairly localized and occurs from irritation of the skin or mucosa. The so-called first pain is modulated by the A-delta fibers, followed by second pain modulated by C-fibers. Deep somatic pain may occur from irritation of structures such as periosteum, ligaments, joints, tendons, fascia, and muscles (in order of lower to higher pain threshold). Somatic structures have been shown, by Kellgren’s classic studies, to refer pain distal to the site of irritation.5 On the other hand, radicular pain is fairly precise, shooting, neuropathic pain that is along a two-inch band.7 Many cases of thoracic somatic referred pain are misdiagnosed as thoracic radicular pain. It must be remembered that thoracic disc herniations as causes of thoracic radicular pain are rare. Thoracic somatic referred pain is much more common than thoracic radicular pain.
Table 71.2 Types of Pain: Somatic vs. Autonomic Nervous System
| Superficial cutaneous pain |
| Somatic pain |
| Somatic localized pain |
| Somatic referred pain |
| Radicular pain |
| Visceral pain |
| True or localized visceral pain |
| Visceral referred pain |
| Localized parietal pain |
| Referred parietal pain |
Thoracic spinal cord and its primary divisions
Spinal cord
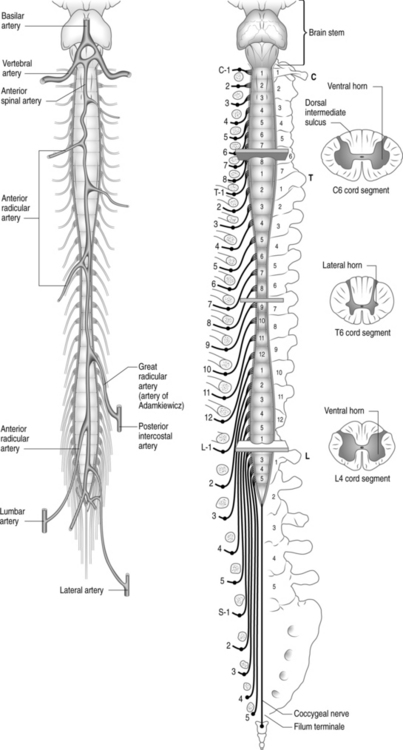
The spinal cord is housed within the thoracic vertebral canal, which has a relatively small diameter when compared to the cervical and lumbar canal (Fig. 71.2). The lower thoracic vertebral canal and spinal cord are wider to allow for the lumbar segment of the spinal cord. In addition, the vertebral column grows at a faster rate than the spinal cord. Consequently, the newborn spinal cord ends by the L3 vertebral, whereas the adult spinal cord ends between T12 and L2 vertebral bodies.2 Overall, the thoracic spinal cord is smaller in size and has less gray matter relative to the cervical and lumbar spinal cord. There is less relative room in the thoracic vertebral canal and sparse cord vascular supply; thus, the thoracic spinal cord is a precarious area for injury. For those reasons, posterior thoracic decompression (particularly laminectomies) carries a greater relative risk of neural injury.8 In addition, the thoracic spinal cord has an enlargement of the lateral horn due to the incorporation of cell bodies of the preganglionic fibers of the sympathetic nervous system.
The spinal cord receives its vascular supply via the anterior spinal artery (ventral two-thirds of the cord) and a pair of posterior spinal arteries (dorsal one-third of the cord). The anterior spinal artery in the thoracic spine is feed by 4–5 radicular arteries. The largest of these radicular arteries is the great radicular artery of Adamkiewicz, which usually courses with a lower thoracic root or upper lumbar root (see Fig. 71.2). It will give vascular supply to the lumbosacral spinal cord segments. The anatomic course and supply of this great radicular artery has become clinically important for spinal injectionists. Inadvertent injection of particulate matter (steroid) into the greater radicular artery while performing a thoracolumbar transforaminal epidural steroid injection may cause paraplegia.9 Other invasive procedures such as lumbar sympathectomy and aortic surgery, or a dissecting aneurysm, may also interrupt supply to the greater radicular artery.2
In addition, the venous plexus about the thoracic spine has been implicated with metastatic cancer. In fact, the thoracic region is the most common location for metastatic spinal spread of many cancers.10
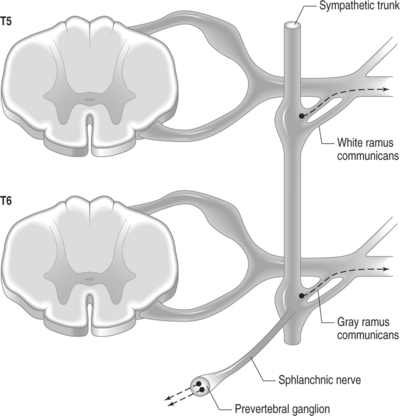
Branches of the thoracic spinal cord
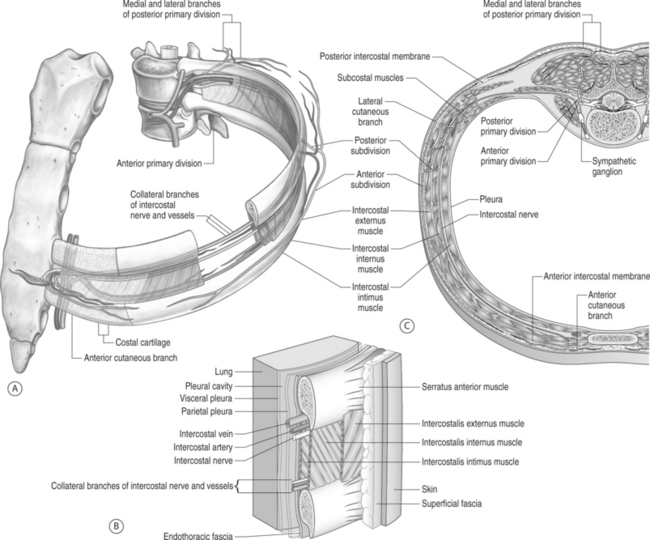
The thoracic spinal cord provides the afferent and efferent contributions to the thoracic dorsal and ventral rootlets, respectively (Fig. 71.3). The rootlets come together to form ventral and dorsal roots. Within the intervertebral foramen, the roots form the short spinal nerve. As the spinal nerve exits the foramen, it enters the thoracic paravertebral space. Within this space, various branches are formed. The large anterior (ventral rami) and posterior (dorsal rami) primary divisions are created and housed within this space. Just before dividing into the rami, the sinuvertebral nerve is formed and returns medially through the intervertebral foramen. Also before the primary divisions are formed, the white and gray rami communicantes branches to the sympathetic trunk (Fig. 71.4). A thoracic paravertebral block will anesthetize all of the above branches.11
The thick anterior primary division is referred to as the ventral rami as well as the segmental nerve. The first 11 thoracic segmental nerves are named the intercostal nerves while the twelfth segmental nerve is named the subcostal nerve. Notably, the anterior primary division of T1 contributes to the brachial plexus. The second and third intercostal nerves also form the intercostobrachial nerve, which provides cutaneous innervation to the axilla and upper medial arm. The intercostobrachial nerve may be injured during axillary surgery and dissection. Thoracotomy incisions may famously cause injury to other levels of intercostal nerves. In fact, up to 61% of individuals may have a degree of post-thoracotomy pain one year after surgery.12
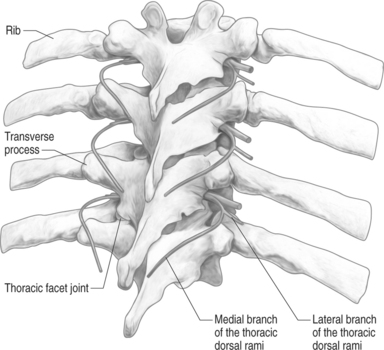
Thoracic posterior primary division (dorsal rami) and its medial branches
The posterior primary rami (dorsal rami) further divides into the medial and lateral branches. The posterior primary rami also provide cutaneous innervation to the skin overlying the spinous process, the paravertebral musculature, and the thoracic facet joints. Beginning at the T4 posterior primary rami, each division will travel further and further caudally to provide cutaneous innervation (Fig. 71.5).6
The thoracic dorsal rami are formed within 5 mm of the lateral intervertebral foramen. The thoracic transverse process acts as a good landmark for the medial branches of the thoracic dorsal rami. However, it must be remembered that the transverse process of the thoracic spine is a true process, whereas the transverse process of the lumbar spine is actually a costal remnant.13 Thus, the anatomical scheme of the thoracic medial branches will vary slightly as compared to the lumbar medial branches. The opening where the thoracic dorsal rami exits is also referred to as the costotransverse foramen of Cruveilhier.2 The superior border is the transverse process; the medial border is the thoracic facet joint; the inferior border is the inferior rib; and the lateral border is the superior costotransverse ligament.
The thoracic medial branches pass within the intertransverse space, i.e. the interval between consecutive transverse processes (Fig. 71.6).13 Depending on the thoracic level, the medial branches pass at different mediolateral points within the intertransverse space.14 After crossing the transverse process, the medial branch will head medially and inferiorly. It will then serve to innervate the zygapophyseal joint at the level of its spinal nerve and the joint below. At T1–3 and T9–10, the medial branches cross the superior and lateral aspect of the transverse process. At T4–8, the medial branches may be suspended within the intertransverse space. At T11–12, the medial branch has a course akin to the lumbar medial branches such that they pass at the medial aspect of the transverse process, at the root of the superior articular process (Table 71.3). Thoracic medial branch blocks can be performed for the treatment and diagnosis of thoracic facet-mediated spinal pain. The target site for these blocks, based on the above described anatomy, is typically at the superolateral aspect of the thoracic transverse process.14 These blocks are technically easier to perform than thoracic facet intra-articular injections; thus, the medial branch anatomy needs to be well understood.
Table 71.3 Target Sites for Blocking Thoracic Medial Branches
| Thoracic Level | MB Description | Target Site |
|---|---|---|
| T1–3 | Superolateral TP | |
| T4–8 | ‘Suspended medial branch’ | Intertransverse space |
| T9–10 | Superolateral TP | |
| T11–12 | ‘Lumbar-like’ | Junction of the SAP and TP |
TP, transverse process; SAP, superior articular process.
The lateral branches provide innervation to erector spinae muscles and midline skin. Beginning at the T4 posterior primary rami, each division will travel further and further caudally to provide cutaneous innervation.6 The lateral branches may descend up to 4 ribs before providing cutaneous innervation superficial to the spinous process.
Thoracic sinuvertebral nerves
The thoracic sinuvertebral nerve (SVN or recurrent meningeal nerve) is similar in origin to the lumbar and cervical sinuvertebral nerves. They arise from both a somatic and autonomic root. The origin of the SVN actually begins outside of the neural foramen, and then it proceeds back through the foramen to form its terminal branches (see Fig. 71.3). Contributions of segmental spinal nerve (somatic root) and gray rami communicantes/sympathetic trunk (multiple autonomic roots) to the SVN explain the vast referral pattern of thoracic disc pain. The SVN provides nerve supply to the following: the posterior longitudinal ligament, dural sac, anterior surface of vertebral lamina, and posterior aspect of the vertebral body.4 The thoracic SVN presumably innervates the outer annulus of thoracic discs; however, this is extrapolated from dissection studies of the lumbar spine.4 The thoracic intervertebral disc will be innervated multisegmentally and bilaterally, further explaining its vast referral pattern.
Thoracic sympathetic trunk
The autonomic nerve system has an enormous role in the modulation of pain, particularly visceral pain. The thoracic spine houses nearly the entire peripheral sympathetic nervous system. The anatomy of the sympathetic and parasympathetic nerves needs to be wholly understood by pain medicine practioners. The sympathetic division of the autonomic nervous system is also termed the thoracolumbar division because the cell bodies of the preganglionic fibers are typically housed from T1 to L2 inclusive. These cell bodies are located in the intermediolateral column of the spinal cord (i.e. lateral horn). The preganglionic fibers are incorporated within the anterior root and traverse through the white rami communicantes. The preganglionic fibers end or synapse in the paravertebral sympathetic trunks. Some preganglionic fibers may ascend or descend two levels before synapsing in the sympathetic trunks. Postganglionic fibers have cell bodies in the sympathetic trunks and may pass through the somatic nerves (traversing through the gray rami communicantes) or the visceral nerves.
The sympathetic trunk in the thoracic spine lies more posterior.13 In fact, the trunk sits just anterior to the ribs, in close proximity to the pleura and segmental nerve (thoracic ventral rami). Thus, sympathetic nerve blocks are inherently more risky than in the lumbar spine. The thoracic sympathetic trunks form intermittent ganglia at each thoracic vertebral level. The first thoracic ganglion typically fuses with the lower cervical ganglia to form the stellate ganglion. In addition, the first thoracic ganglion is the sole location for the preganglionic sympathetic fibers of the head and neck. Interruption to these fibers will result in Horner’s syndrome (ptosis, miosis, and anhidrosis).6 The upper 4–5 thoracic ganglia form visceral and vascular branches to the thoracic viscera and aorta, respectively.
BONE AND JOINT ANATOMY
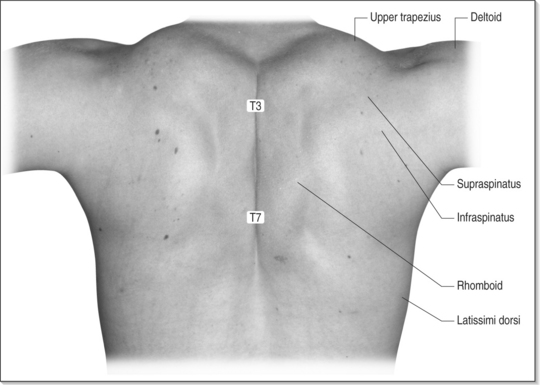
Surface anatomy: bony landmarks
The T1 spinous process is easily palpated by identifying the relatively mobile C7 spinous process on top of it. The spine of the scapula is usually located at the level of the T3 spinous process (Fig. 71.7). The inferior angle of the scapula corresponds to the level of T6 spinous process in the prone position and T7 in the standing position. The apex of the thoracic kyphosis is usually located at the level from T4 to T6.2
Vertebral column
The thoracic bony architecture provides for a stable and compact portion of the vertebral column (Fig. 71.8). Posteriorly, the thoracic laminae are arranged like overlapping shingles on a roof. Anteriorly, each of the 12 thoracic vertebral bodies is cortical bone surrounding cancellous (trabecular) bone. The anterior height of the thoracic vertebral body is normally 1.5–2 cm shorter than the posterior height, creating the thoracic kyphosis.3 A loss of kyphosis, referred to as straight back syndrome, may be associated with a systolic heart murmur.15 The cancellous bone is particularly susceptible to osteoporosis. In particular, the mid and lower thoracic vertebral bodies are common locations of osteoporotic fractures. The attaching ligaments, such as the anterior longitudinal ligament and posterior longitudinal ligament, are arranged similarly to the rest of the spine.
The thoracic transverse processes are also ‘formidable structures.’13 They serve as useful landmarks for thoracic spinal injections. The direction of the thoracic transverse process is in a cranial and marked posterior manner. They are more easily seen on radiography with a mild contralateral oblique projection.13
Thoracic intervertebral disc
Provocation thoracic discography has shown that pain can emanate from the thoracic discs.16 The intervertebral disc is composed of two main structures. The outer component of the disc is the anulus fibrosus, made of concentric lamellae that encapsulate the gelatinous nucleus pulposis. Thoracic discs are thinner than their respective cervical and lumbar counterparts. They also have a greater tendency to calcify. Innervation of the thoracic intervertebral disc (IVD) may come from the sinuvertebral nerve or rami communicantes.17 Disruptions of the thoracic IVD are rare when compared to the lumbar and cervical spine. They account for 0.15–1.8% of all disc herniations.2,18 Typically, thoracic disc herniations are noted in the mid and lower thoracic spine. Therefore, typical thoracic radicular pain radiates to the abdomen (Table 71.4). Because the thoracic spinal nerves exit at the level below the corresponding vertebral level, a T10–11 lateral disc herniation will affect the T10 spinal nerve. The rarity of thoracic radiculopathy may also be due to the fact that thoracic spinal nerves occupy less relative space (1/12) in the intervertebral foramen when compared to the cervical (1/5) and lumbar spine (1/3).2
| T6 | Xiphoid |
| T8 | Lower rib cage |
| T10 | Umbilicus |
| T12 | Inguinal line |
Thoracic zygapophyseal joints
Several distinct synovial joints (discussed below) that exist within the thoracic spine are enveloped by thin capsules.6 The zygapophyseal joints (facet joints) are the major connections between the thoracic segments. Their joint lines lie mostly in the frontal plane to limit flexion and extension. With a normal X-ray of the thoracic spine, the superior and inferior articular processes are indistinguishable.13 They form a wide articular pillar that is located lateral to the vertebral body. Specifically, the lateral aspect of the thoracic facet joint is slightly anterior, and the medial aspect is slightly posterior.19 The anterior aspect of the thoracic facet joint is formed by the ligamentum flavum. The posterior aspect of the capsule must be penetrated for an intra-articular injection of the thoracic facet joint. Clinically, the thoracic facet joints have been proven to be sources of pain. Dreyfuss et al. demonstrated that the referral zone for the thoracic facet joints is localized to no more than 2.5 segments inferior to the provoked joint.19 As well, the lower thoracic facet joints have been theorized to refer to the lumbar spine, iliac crest, and buttock (i.e. Maigne’s syndrome).20
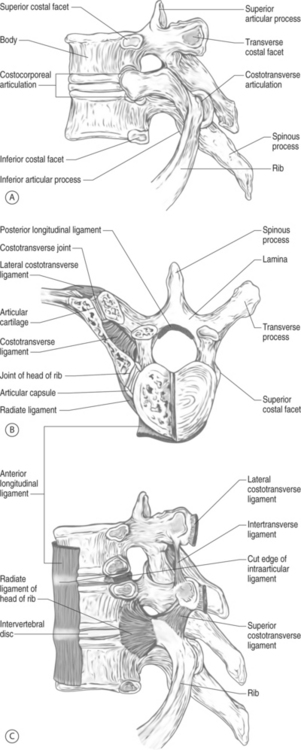
Costovertebral and costotransverse joints
The costovertebral (CV) joints have been implicated as pain generators in individuals with ankylosing spondylitis and osteoarthritis, yet CV joint pain is extremely rare (see Fig. 71.8).17,21 They are innervated by the sympathetic trunks which lie just anterior to the CV joints.22 Often, they are pictured as a circular shadow in the lateral aspect of the superior vertebral endplate.13 This shadow should not be confused for the thoracic pedicle. The CV joint may have two articulations to the vertebral body yet only one synovial capsule.6 The radiate ligament serves to further secure CV rib articulation to the thoracic spine. Degenerative osteoarthritis is most commonly found in the T1, T6–8, and T11–12 levels but is typically asymptomatic.17 CV pain in patients with ankylosing spondylitis is typically found in individuals who also have other spondyloarthritic features such as sacroiliitis.4
The costotransverse (CT) joints are potential sources of pain that are not easily diagnosed by clinical examination. They have yet to be confirmed as pain generators in any published literature.14 They are absent at T1, T11, and T12 levels. They are innervated by the lateral branches of the thoracic dorsal rami.17 A debate exists whether a single lateral branch or up to three innervate a single CT joint.14
MUSCLE AND FASCIA ANATOMY
Surface anatomy
The trapezius, latissimus dorsi, and periscapular muscles encompass the superficial muscles of the thoracic spine region (see Fig. 71.7). The trapezius is a diamond-shaped muscle innervated by the accessory nerve. It works as a force couple to provide various scapular triplanar motions. The latissimus dorsi originates from the thoracolumbar fascia and inserts onto the humerus. It is often described as the swimmer’s muscle as it provides for shoulder extension and internal rotation. The other periscapular muscles include the serratus anterior and posterior, rhomboids, levator scapulae, and rotator cuff musculature. All of these muscles are derived from embryogenic hypomeres and thus are innervated by ventral rami. At the lower, lateral portion of the posterior trunk, the quadratus lumborum sits as a quadrangular-shaped muscle that has direct insertions to the thoracic and lumbar spine. McGill states the quadratus lumborum is a major stabilizer of the spine, typically working isometrically.23
The thoracolumbar fascia and its muscular attachments
The thoracolumbar fascia acts as ‘nature’s back belt.’ It works as a retinacular strap of muscles of the thoracic and lumbar spine. The thoracolumbar fascia consists of three layers: the anterior, middle, and posterior layers. Of these layers, the posterior layer has the most important role in supporting the spine and abdominal musculature. The posterior layer consists of two laminae: a superficial lamina with fibers passing downward and medially and a deep lamina with fibers passing downward and laterally. The transversus abdominis has large attachments to the middle and posterior layers of the thoracolumbar fascia.24 The transversus abdominis fibers run horizontally around the abdomen, allowing for hoop-like stresses with contraction. The internal oblique also has similar fiber orientation to the transversus abdominis, yet receives much less attention with regard to its creation of hoop stresses. Together, the internal oblique, external oblique, and transversus abdominis increase the intra-abdominal pressure from the hoop created via the thoracolumbar fascia, thus imparting functional stability of the thoracolumbar spine.
In essence, the thoracolumbar fascia provides a link between the lower limb and the upper limb.25 With contraction of the muscular contents, the thoracolumbar fascia acts as an activated proprioceptor, like a back belt providing feedback in lifting activities.
Paraspinals
All paraspinal musculature were originally segmental muscles. But, through the course of ontogenetic and phylogenetic development, the larger superficial muscles became muscle masses that extended the length of the spine.26 There are no paraspinal muscles that are purely confined to the thoracic spine, so a general discussion of all back musculature follows. For example, the splenius muscles originate from the spinous process of the upper thoracic spinous processes and extend into the cervical spine. They act mainly to rotate the head and neck. The paraspinal muscles also have the commonality of being derived from the embryogenic epimeres, and thus, they are all innervated by the dorsal rami. Division of these muscles is purely arbitrary as they work in concert. They act mainly to rotate the head and neck. For the sake of convenience, the paraspinals are further divided into two major groups: (1) the erector spinae (global) muscles and (2) and the transversospinalis (local) muscles.
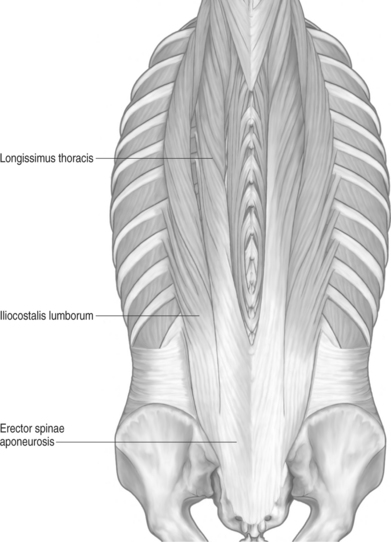
All muscles of the erector spinae have a common tendinous and fleshy origin from pelvis and spinous process of the thoracolumbar region.26 The erector spinae becomes three distinct subgroups of muscles. In the thoracic region, the lateral two subgroups become evident: longissimus system and iliocostalis (lateral) system (Fig. 71.9). These are actually primarily thoracic muscles that act on the lumbar via a long tendon that attaches to the pelvis. This long moment arm is ideal for lumbar spine extension and for creating posterior shear with lumbar flexion.23 Medial to these two systems of muscles lies the slender and poorly developed spinalis thoracis which is also considered an erector spinae muscle. Together the spinalis, longissimus, and iliocostalis form the erector spinae muscles (also termed the SLI muscles).
Deep and medial to the erector spinae muscles lay the local transversospinalis muscles. These so-called local ‘fine-tuning’ muscles include the semispinalis, multifidi, rotators, and intertransversi muscles. They do not have a great moment arm and likely represent length transducers or position sensors of a spinal segment by way of their rich composition of muscle spindles. Of this transversospinalis group, the semispinalis crosses the most spine segments (from 5 to 8) while the multifidi pass the fewest segments (2–3 spinal levels).26 The multifidi are theorized to work as segmental stabilizers rather than being involved in gross spinal movement.7 They are well developed in the lumbar spine but poorly developed in the thoracic spine. The rotatores, on the other hand, are more developed in the thoracic spine and less developed in the lumbar spine.2 The rotatores also have very short muscle fibers and extend 1–2 spinal levels. They act similarly to the multifidi.
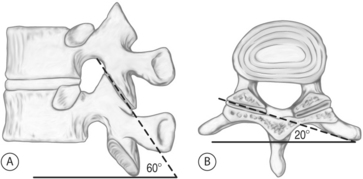
BIOMECHANICS
Movement of the thoracic spine is minimal. The orientation of the thoracic facet joints in the frontal plane will dictate directions of movement freedom (Fig. 71.10). In general, the thoracic spine is free to move in the transverse plane and somewhat in the frontal plane. Side-bending (frontal plane) motion is prevented by the ribs and sternum. Rotatory (transverse) motion is the dominant motion. Flexion and extension is limited to about 10 degrees of motion due to the orientation of the facet joints. The lower thoracic spine, without definitive articulations to the ribs and sternum, has the most freedom of movement. The lower thoracic segments, acting as a transition to the lumbar spine, have an increased ability to flex and extend.
1 Bogduk N. Thoracic spinal pain: where do we stand. Paper presented at: International Spinal Injection Society 11th Annual Scientific Meeting, 2003; Orlando, Florida.
2 Cramer G, Darby S. Basic and clinical anatomy of the spine, spinal cord, and ANS. St. Louis: Mosby, 1995.
3 Levangie PK, Norkin CC. Joint structure and function, 3rd edn. Philadelphia: FA Davis, 2001.
4 Bogduk N. Innervation and pain patterns of the thoracic spine. In: Grant R, editor. Physical therapy of the cervical and thoracic spine. 3rd edn. New York: Churchill Livingstone; 2002:73-81.
5 Kellgren J. On the distribution of pain arising from deep somatic structures with charts of segmental pain areas. Clin Sci. 1939;4:35-46.
6 Bonica J, Graney D. General considerations of pain in the chest. In: Loeser J, editor. Bonica’s management of pain. 3rd edn. Philadelphia: Lippincott Williams & Wilkins; 2001:1113-1148.
7 Bogduk N. Clinical anatomy of the lumbar spine and sacrum, 3rd edn. New York: Churchill Livingston, 1997.
8 Leventhal M. Fractures, disclocations, and fracture-dislocations of spine. In: Canale S, editor. Campbell’s operative orthopaedics. St. Louis: Mosby; 2003:1597-1690.
9 Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002;2(1):70-75.
10 Aebi M. Spinal metastasis in the elderly. European Spine Journal. 2003;12:S202-S203.
11 Karmakar MK. Thoracic paravertebral block. Anesthesiology. 2001;95(3):771-780.
12 Perttunen K, Tasmuth T, Kalso E. Chronic pain after thoracic surgery: a follow-up study. Acta Anaesthesiol Scand. 1999;43(5):563-567.
13 Sluijter M. Radiofrequency part 2: thoracic and cervical region, headache, and facial pain. Meggen, Switzerland: FlivoPress, 2003.
14 Chua WH, Bogduk N. The surgical anatomy of thoracic facet denervation. Acta Neurochirurgica. 1995;136(3–4):140-144.
15 Spapen HD, Reynaert H, Debeuckelaere S, et al. The straight back syndrome. Neth J Med. 1990;36(1-2):29-31.
16 Schellhas KP, Pollei SR, Dorwart RH. Thoracic discography. A safe and reliable technique. Spine. 1994;19(18):2103-2109.
17 Chua W. Thoracic spinal pain – a review. Austr Musculoskel Med. 1996;4:280-289.
18 Wood KB, Blair JM, Aepple DM, et al. The natural history of asymptomatic thoracic disc herniations. Spine. 1997;22(5):525-529.
19 Dreyfuss P, Tibiletti C, Dreyer SJ. Thoracic zygapophyseal joint pain patterns. A study in normal volunteers. Spine. 1994;19(7):807-811.
20 Akuthota V, Willick S, Harden R. The adult spine: a practical approach to low back pain. In: Rucker K, Cole A, Weinstein S, editors. Low back pain: a symptom-based approach to diagnosis and treatment. Woburn, MA: Butterworth-Heinemann; 2001:15-42.
21 Pascual E, Castellano JA, Lopez E. Costovertebral joint changes in ankylosing spondylitis with thoracic pain. Br J Rheumatol. 1992;31(6):413-415.
22 Erwin WM, Jackson PC, Homonko DA. Innervation of the human costovertebral joint: implications for clinical back pain syndromes [erratum appears in J Manip Phys Ther 2000; 23(8):530]. J Manip Phys Ther. 2000;23(6):395-403.
23 McGill S. Low back disorders: evidence-based prevention and rehabilitation. Champaign, Illinois: Human Kinetics, 2002.
24 Richardson C, Jull G, Hodges P, et al. Therapeutic exercise for spinal segmental stabilization in low back pain. Edinburgh, Scotland: Churchill Livingstone, 1999.
25 Vleeming A, Pool-Goudzwaard AL, Stoeckart R, et al. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine. 1995;20(7):753-758.
26 Jenkins D. Hollinshead’s functional anatomy of the limbs and back, 7th edn. Philadelphia: WB Saunders, 1998.