CHAPTER 85 Development of the pelvic girdle and lower limb
STAGES OF LOWER LIMB DEVELOPMENT
VESSELS IN THE LOWER LIMB
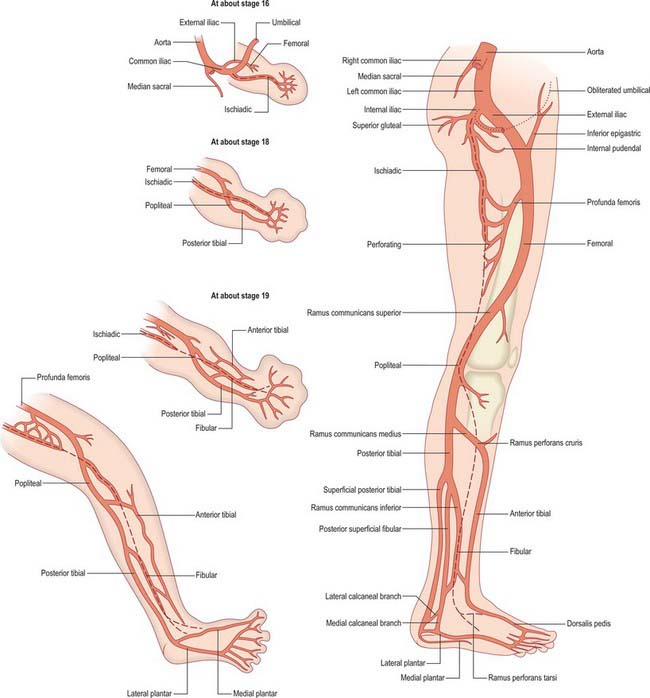
The axial artery of the lower limb arises from the dorsal root of the umbilical artery and courses along the dorsal surface of the thigh, knee and leg (Fig. 85.1). Below the knee it lies between the tibia and popliteus, and in the leg it lies between the crural interosseous membrane and tibialis posterior. It gives off a perforating artery that traverses the sinal tarsus to form a dorsal network and ends distally in a plantar network. The femoral artery passes along the ventral surface of the thigh, opening a new channel to the lower limb. It arises from a capillary plexus that is connected proximally with the femoral branches of the external iliac artery and distally with the axis artery. At the proximal border of popliteus the axis artery splits into primitive posterior tibial and fibular branches which run distally on the dorsal surface of popliteus and tibialis posterior to gain the sole of the foot. At the distal border of popliteus the axis artery gives off a perforating branch which passes ventrally between the tibia and the fibula and then courses to the dorsum of the foot, forming the anterior tibial and dorsalis pedis arteries. The primitive fibular artery communicates with the axis artery at the distal border of popliteus and in its course in the leg.
The proximal parts of the primitive posterior tibial and fibular arteries fuse but they remain separate distally. Ultimately, much of the primitive fibular artery disappears; a part of the axis artery is incorporated in the permanent fibular artery. The same considerations apply to anomalies and variations as were described for the developing forelimb (see Ch. 52).
NEONATAL LOWER LIMB
LOWER LIMB ANOMALIES
The categories of limb defects described by Swanson (1976) are given in Chapter 52. Although devised for the upper limb, they apply in the same manner to the lower limb.
Congenital talipes equinovarus, or club foot, derives its name from a combination of talus and pes, together with terms describing an elevated heel resembling that of a horse (equino), which is also turned inwards (varus). It is a common neonatal anomaly and occurs in approximately 1 per 1000 live births, with males affected twice as often as females. There is some degree of inheritance, so it is not entirely an effect of intrauterine positioning or of oligohydramnios (abnormally little amniotic fluid). Both bones and soft tissues are affected and it is difficult to tell which are primary effects and which are secondary. A number of theories have been proposed to explain the underlying pathogenetic mechanism(s), including abnormal tendon and ligament attachments and delayed muscle maturation. The most widely held theory is that the talus undergoes defective development and that all the other deformities arise as a consequence of this initial defect. The talus is decreased in size by up to 25%. It has a foreshortened neck and decreased body/neck angle, and the subtalar facets are medially rotated. The navicular is small and medially deviated relative to the talus. The calcaneus is also small and shows varus displacement and equinus tilt: the anterior facets correspond to those of the talus (Barlow & Clarke 1994). The entire affected foot and calf are smaller than their normal counterparts. The foot is inverted and supinated and the forefoot is adducted. The heel is small, rotated inwards and elevated. The calcaneus is inverted beneath the talus. Treatment varies between splintage and repeated complex surgery, which reflects the highly variable severity of the condition and individual response to therapy.