Chapter 60 Dermatoses of pregnancy
Specific dermatoses of pregnancy
2. What is pruritic urticarial papules and plaques of pregnancy?
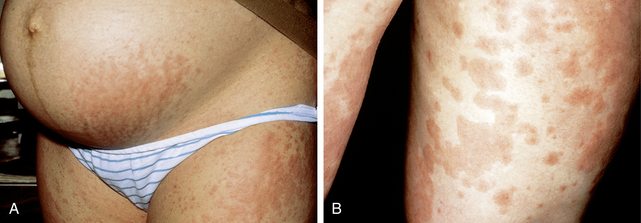
Pruritic urticarial papules and plaques of pregnancy (also known as polymorphic eruption of pregnancy, or PUPPP) has an incidence of 1/200 pregnancies. The onset of PUPPP is usually in the third trimester. The pruritic, erythematous, papules and plaques are usually first seen in the abdominal striae (stretch marks) and then spread to the chest, trunk, and extremities. The papules and plaques typically spare the palms, soles, face, and mucous membranes. Large vesicles or bullae are uncommon, though pinpoint vesicles may be seen (Fig. 60-1).
4. How is PUPPP treated?
6. What is pemphigoid gestationis?
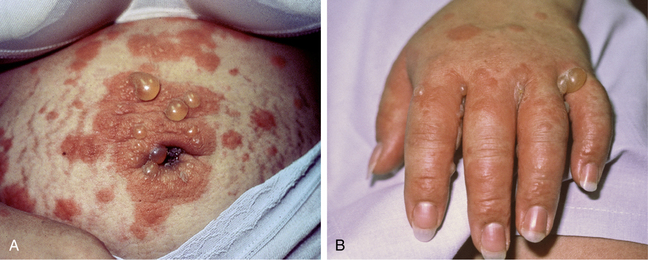
Pemphigoid gestationis (also called herpes gestationis or gestational pemphigoid) is an autoimmune subepidermal bullous disorder of pregnancy that may start in the 2nd trimester, the 3rd trimester, or in the postpartum period. The skin lesions are characterized by urticarial papules and plaques, which then progress into painful bullae. The lesions of pemphigoid gestationis initially present periumbilically (Fig. 60-2A), and then spread to involve the trunk and extremities (Fig. 60-2B), usually sparing the face.
7. What are the antigens associated with the development on pemphigoid gestationis?
Bullous pemphigoid antigen 2 (BPAG2) is a 180 kDal transcellular glycoprotein that is part of the hemidesmosome (a structure that binds epithelial cells to the basement membrane of the epidermis). IgG binds to BPAG2 and triggers the classic complement pathway leading to a deposition of C3 along the basement membrane zone (Fig. 60-3). Deposition of complement along the basement membrane zone leads to a recruitment of inflammatory cells, particularly eosinophils. This cascade ultimately leads to a release of proteolytic enzymes that cleave portions of the epidermis from the dermis.
Key Points: Pemphigoid Gestationis
1. Pemphigoid gestationis is an autoimmune disease that occurs during pregnancy, and it is characterized by IgG1 antibodies directed at bullous pemphigoid antigen–1 in the basement membrane zone.
2. Direct immunofluorescent study demonstrates linear C3 and/or IgG along the basement membrane zone and is the diagnostic test of choice to establish the diagnosis.
8. Which histocompatibility leukocyte antigen (HLA) types have been associated with pemphigoid gestationis?
9. Compare PUPPP and pemphigoid gestationis.
See Table 60-1.
Table 60-1. Compare and Contrast PUPPP and Pemphigoid Gestationis
| PUPPP | PEMPHIGOID GESTATIONIS | |
|---|---|---|
| Clinical presentation | Pruritic erythematous papules and plaques Initial lesions present in the abdominal striae, spreading to the trunk and extremities; vesicles may be present Usually spares the palms and soles |
Urticarial papules, plaques, and blisters Initial lesions start periumbilically and spread to the trunk and extremities The palms and soles are commonly involved |
| Direct immunofluorescence | Occasional complement deposition in a perivascular location or in a granular formation along the dermal–epidermal junction | Linear deposition of IgG (25% of the time) and complement (C3) at the dermal–epidermal junction. (see Fig. 60-3) |
| Fetal sequelae | None | Increased risk of intrauterine growth restriction and prematurity 3%–10% of newborns have lesions of neonatal pemphigus |
| Treatment | Topical corticosteroids Oral antihistamines |
Topical or oral corticosteroids (prednisone 0.5 mg/kg/day) Oral antihistamines Dapsone, cyclosporine (results are mixed) |
| Recurrence in future pregnancies | Usually does not recur | Usually recurs at an earlier gestation and is typically more severe |
10. What is atopic eruption of pregnancy?
Atopic eruption of pregnancy is classified to include eczema of pregnancy, prurigo gestationis, and folliculitis of pregnancy. According to the retrospective study by Ambros-Rudolph et al, it is the most common dermatoses of pregnancy, with a prevalence of 50.7%. In this study 20% of the patients were known to have preexisting atopic dermatitis, but 80% of the patients reviewed experienced symptoms de novo during pregnancy. It is known to start early in pregnancy, before the third trimester. The skin lesions are erythematous, excoriated papules, plaques, or nodules on the extensor surfaces of the limbs and on the trunk, and may appear crusted and eczematous. The treatment involves topical corticosteroids, and the disease usually resolves in the postpartum period.
11. What is intrahepatic cholestasis of pregnancy?
Intrahepatic cholestasis of pregnancy (ICP) is characterized symptomatically by an intense pruritus, most often starting on the palms and soles, and then becoming generalized. There are no other dermatologic findings except excoriations. ICP usually occurs in the third trimester of pregnancy. The etiology of intrahepatic cholestasis of pregnancy is not completely understood, but there is a strong indication that there is interplay between a rise in pregnancy hormones (estrogen and progesterone), accumulation of bile acids secondary to liver dysfunction, and genetic susceptibility contributing to development of this disease.
13. Are there specific laboratory findings to establish the diagnosis?
Yes. The most specific laboratory derangements are found when measuring bile acids, specifically cholic acid and deoxycholic acid, which may be elevated more than 100 times (upper end of normal: 10 μmol/L). Liver transaminases (aspartate transaminase [AST], alanine transaminase [ALT]) may also be elevated, but ALT is thought to be the more sensitive marker, with an increase of 2 to 10 times the upper limit of normal. Bilirubin levels may be elevated, but total bilirubin levels do not often exceed 6 mg/dL.
14. What risks and outcomes are associated with intrahepatic cholestasis of pregnancy?
The main risks are to the fetus; the fetus is unable to excrete cholic acid, resulting in toxicity. Sudden intrauterine fetal death occurs in 1% to 2% of pregnancies affected by ICP. Other complications include respiratory distress syndrome, meconium staining of amniotic fluid membranes, and premature delivery. The risk of fetal complications increases with bile acids levels >40 μM/L. There are not usually any long-term maternal sequelae. The pruritus associated with ICP usually resolves within 48 hours to 2 weeks, after delivery.
Hepburn I: Pregnancy-associated liver disorders, Dig Dis Sci (53):2334–2358, 2008.
15. How is cholestasis of pregnancy treated?
See Table 60-2.
Table 60-2. Treatment Regimens of ICP
| Ursodeoxycholic acid 15 mg/kg/day | Decreases bile acid concentration Aids in transplacental transport of bile acids |
| S-adenosyl-methionine | Reverses estrogen induced cholestasis in experimental animals Minimally improves bile acid laboratory values and pruritus Studies show conflicting evidence regarding the efficacy of this drug |
| Cholestyramine | Generally not shown to be effective |
| Dexamethasone | Inhibits placental estrogen synthesis Does not improve pruritus or transaminase levels Repeated doses may be associated with decreased birth weight and other fetal complications |
| Delivery | Delivery is the cure for ICP Most authors recommend early delivery by 38 weeks (∼36 weeks for severe laboratory derangements) |
Hepburn I: Pregnancy-associated liver disorders, Dig Dis Sci (53):2334–2358, 2008.
16. Is impetigo herpetiformis a distinct clinical disease?
Impetigo herpetiformis is a rare disorder that typically presents in the third trimester. This disease is characterized by sterile pustules on an erythematous plaque initially presenting on the flexural and intertriginous areas, and then progressing to involve the trunk and remaining surfaces of the extremities. Impetigo herpetiformis can involve the mucous membranes. There also can be nail involvement, as well as systemic symptoms such as fever and malaise. It is associated with an increased risk of intrauterine growth restriction and stillbirth. Clinically and histologically, impetigo herpetiformis resembles pustular psoriasis, and it is debated whether or not impetigo herpetiformis is a distinct disease.
18. What is the treatment for impetigo herpetiformis?
Physiologic skin changes in pregnancy
20. What are some of the normal pigmentary changes that can be associated with pregnancy?
21. Why do these pigmentary changes occur?
22. How does pregnancy affect patients with melanoma?
23. Is pregnancy associated with changes in hair growth?
In pregnancy, women experience a prolonged anagen phase, which leads to clinical thickening of the hair. The hairs shift into a telogen phase 1 to 5 months following delivery, and these patients then experience a telogen effluvium. Hirsutism (male pattern facial and body terminal hair growth) may also increase in pregnancy, and usually resolves 6 months postpartum.
26. Discuss two cutaneous tumors often associated with pregnancy.
1. Pyogenic granuloma of pregnancy (granuloma gravidarum) is a cutaneous tumor consisting of a vascular proliferation, most often of the gingival tissue in pregnant women. These tumors may ulcerate and become painful. Pyogenic granuloma usually spontaneously regresses after pregnancy, and if not, can be treated with an ND:YAG laser.
Winton GB: Skin diseases aggravated by pregnancy, J Am Acad Dermatol 20:1–13, 1989.