Dermatomes
What is a dermatome?
A dermatome is defined as the area of skin supplied by one spinal nerve root level. There are 31 pairs of spinal nerves leaving the spinal cord (S2.13) and each one supplies a different area of skin. Therefore the skin supplied by all the individual spinal nerve roots ultimately produces a dermatome map that represents the entire body (Fig. 24.1).
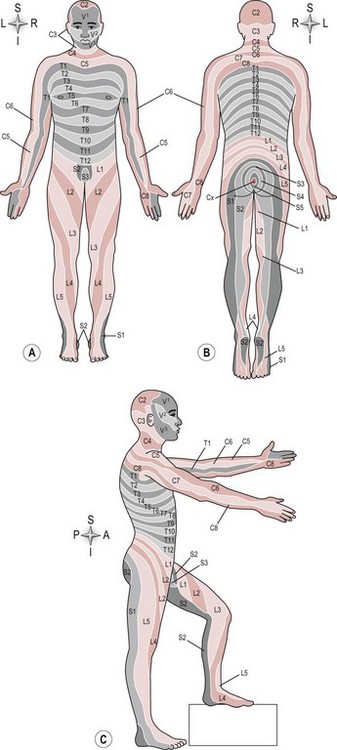
Figure 24.1 (A–C) Dermatome map.
Why do I need to assess dermatomes?
Assessing a dermatome gives information related to nerve integrity, in other words whether the nerve pathway from the skin to the spinal cord is intact. Knowledge of the cutaneous supply of both the spinal nerve root (dermatome) and the peripheral nerve allows the therapist to differentiate between lesions of each (Petty 2006). For example, a sensory loss of the area over the deltoid muscle at the shoulder is identified as dermatome C5. The same area of skin is also part of the sensory distribution of the radial nerve (posterior cutaneous nerve of the arm C5/6/7/8 T1). It is therefore likely, but not certain that the lesion is at the level of the spinal nerve root because a lesion of the peripheral nerve is likely to be more extensive. Accurate diagnosis is only possible with knowledge of anatomy and accurate assessment.
How do I assess a dermatome?
Therapist
1. The therapist can test various sensations.
• Light touch (cotton wool) (S3.23)
• Deep touch/pressure (pressure pen) (S3.23)
• Pain or temperature (neurotip at 45° or heat/non-noxious cold temperature device) (S3.23, 29).
2. These sensations are mapped using the dermatome distribution map (Fig. 24.1). However, as each dermatome originates from a single spinal cord level the dermatomes of consecutive levels tend to overlap making the ability to differentiate between different levels close to the spine (trunk) almost impossible. Therefore the larger, more distal portion of each dermatome is used for testing during the assessment (Fig. 24.2).

Figure 24.2 Testing a dermatome for light touch.
3. The same procedure is used to test for all sensations with the implement for testing changing accordingly. Light touch is described as an example.
4. Explain the procedure to the patient and check their understanding upon an unaffected area of skin.
5. Ask them to close their eyes.
6. Identify a dermatome to test (without telling the patient) and use the cotton wool to dab the centre of that dermatome (Fig. 24.2).
7. Compare the same dermatome on the left and right side of the body.
8. Repeat the procedure using a different dermatome.
9. Randomize the applications to avoid the patient being able to predict a pattern of testing. The therapist then maps out any area of altered or diminished sensation.
Are they able to feel anything? No, anaesthesia (loss of sensation) could indicate a complete lesion of the spinal root pathway.
What do they feel? Any tingling or burning sensations? Paraesthesia or abnormal sensation indicates abnormal transmission along the nerve pathway (S3.23). This could occur as a result of any condition which affects the transmission of action potentials along the neuron. For example, nerve compression, inflammation, infection, virus, reduced circulation or demyelination. Tactile hyperaesthesia or excessive sensation could be a result of peripheral sensitization (S3.29).
Is any sensory loss confined to the dermatome? Yes would implicate a single nerve root. However, if the loss is wider, more than one nerve root could be involved or the lesion may not be specific to the nerve root itself.
Does it feel the same both sides? No. Assuming a unilateral pathology the unaffected side can be used as a normative baseline to assess any abnormalities. In conditions where bilateral lesions are suspected this is not valid and the therapist should compare to an expected norm.





