CHAPTER 41 Dermal Suspension and Parenchymal Breast Reshaping after Massive Weight Loss
Summary/Key Points
Patient Selection
Breast deformities after massive weight loss vary significantly. Common findings include breast ptosis, medialization of the nipple–areola complex, and extension to a lateral chest roll. Many procedures exist to treat the deflated breast after massive weight loss, including short scar mastopexy techniques and combined augmentation/mastopexy.1–7 However, achieving long-lasting results with these techniques in the setting of severe skin laxity can be challenging. The goals for mastopexy after massive weight loss include obtaining a youthful, well-contoured breast with upper pole fullness, proper nipple positioning, and a long-lasting aesthetic result.
Patient goals and expectations must be properly assessed before proceeding with surgery. A full history and physical is always performed, with an emphasis on history of breast disease and analysis of the deformities. Optimal patient criteria for the dermal suspension, parenchymal reshaping mastopexy include profound parenchymal volume loss, skin envelope redundancy, Grade 3 nipple ptosis, medialization of the nipple–areola complex, and the presence of a lateral skin/fat roll or lateral chest wall laxity.8
Indications
As noted above, the indications for dermal suspension, parenchymal reshaping with selective auto-augmentation include patients with deflated, flattened breasts. Patients tend to have dramatic skin laxity and skin excess. Additionally, many patients present with lateral chest rolls of excess skin and/or fat,9 a nd this procedure is very effective in treating that deformity. The goals of this operation include using all available breast tissue and recruitment of surrounding chest wall tissue for selective auto-augmentation, proper placement of the nipple, restoring upper pole fullness, reshaping and reducing the skin envelope without relying on it for support, and eliminating the lateral chest roll and restoring the lateral sweep of the breast.
Relatively few contraindications exist for this procedure. Patients who are active smokers or users of tobacco products are asked to stop one month prior to and after surgery. In accordance with the American Cancer Society, all patients are screened for breast cancer with mammography as appropriate given their individual histories.10 Patients who have had prior breast surgery may not be candidates for this procedure if the scars interfere with the planned procedure. Similarly, patients with severe fibrocystic disease or active intertrigo may not be ideal for surgery. Patients desiring a marked increase in breast volume may be better served by an augmentation/mastopexy technique.
Operative Technique
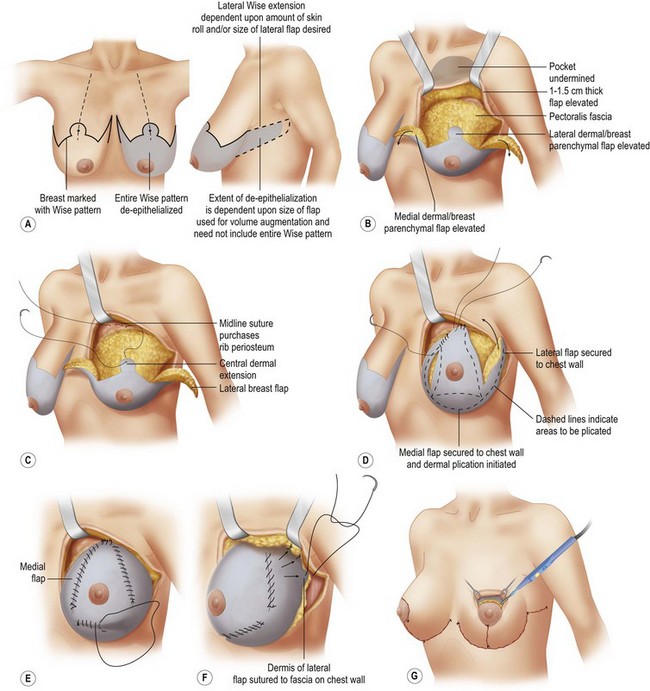
Markings for the dermal suspension, parenchymal reshaping mastopexy are based on an extended Wise pattern with the nipple–areola complex based on a central and inferior pedicle. The sternal notch is identified and marked. A point on the clavicle 5 cm lateral to the sternal notch is identified and a line is drawn down the breast meridian. Often the nipple–areola complex in the massive weight loss patient will lie medial to this mark. The nipple position is then assessed by palpating the inframammary fold and projecting this point onto the surface of the breast. The top of the keyhole Wise pattern is planned from 2 cm above this point. Five centimeter vertical limbs are measured from the keyhole pattern. The Wise pattern is then completed with extension of the lateral portion to encompass the lateral skin roll. This will aid in removal of the skin roll and use of this de-epithelialized portion for selective auto-augmentation. The de-epithelialized portion is limited to the posterior axillary line and robust perforators from the lateral thoracic region allow the flap to be mobilized. The nipple–areola complex is measured at 42 mm with a cookie cutter or washer and de-epithelialization of the entire Wise pattern is begun (Fig. 41.1A).
A pedicle base of 10 cm is measured approximately 6–7 cm from the medial aspect of the Wise pattern. All portions of the incision are then scored through dermis except at its base and the breast parenchyma is then raised as skin flaps with a thickness of 1 to 1.5 cm (Fig. 41.1B). The flaps are constantly assessed by feel to make sure they are of uniform thickness. The flaps are raised until pectoralis fascia is reached and then elevation continues up to the level of the clavicle. Skin flap attachments to the chest wall medially and laterally are released to allow for the dermal suspension and parenchymal reshaping with appropriate redraping of the overlying tissue flaps. Care is taken not to release attachments in the midline over the sternum, which could result in synmastia. Medial and lateral parenchymal flaps are then raised (the flaps usually discarded in a Wise pattern breast reduction) maintaining their attachments to the central pedicle and preserving the 10 cm pedicle base with no undermining.
The first step in the dermal suspension is to secure the top of the de-epithelialized key-hole dermis to the level of the second rib along the breast meridian (Fig. 41.1C). If the central dermal extension is short from the nipple, then the pedicle may need to be secured at a lower rib level to prevent excessive nipple elevation. Fingers of the non-dominant hand are placed in the intercostal spaces surrounding the rib, making sure that the zero-braided nylon suture is safely hitting rib periosteum. Sutures are buried in a mattress fashion. Two sutures are usually placed to ensure stability at this first point of fixation and at the point of fixation for both lateral and medial flaps. Next, the lateral breast flap is secured to the chest wall with periosteal sutures. The first suture is usually placed at one rib level below where the previous central pedicle was suspended (i.e. the third rib). This suture is placed as medially as possible, usually directly under the central pedicle. This is secured with two mattress sutures as well for reinforcement. The length of this flap can be reduced to selectively reduce the amount of auto-augmentation desired. The medial flap is then rotated up to approximately the fourth rib and sutured with periosteal sutures. Redraping of the skin flaps periodically help to assess whether accurate levels of dermal suspension have been achieved.
Parenchymal reshaping is performed using 2-0 absorbable polyglactin suture. The lateral flap is approximated to the central dermal extension (Fig. 41.1D) first using interrupted sutures and then overlayed with a running suture. The same process is repeated medially. To increase nipple projection and shorten the distance from the nipple to the inframammary fold, an inferior plication is created to set a distance of 5 cm (Fig. 41.1E).
To shape the lateral curvature of the breast, the lateral breast flap is secured to the chest wall fascia (Fig. 41.1F), and not to rib periosteum, to avoid injury to the lateral thoracic nerves and vessels. Securing this side of the flap prevents lateral bulging and further enhances nipple projection. Final projection and shape is assessed continuously by redraping the skin flaps to assess contour. The skin flaps are first approximated with a 2-0 polypropylene suture over a petroleum-gauze bolster to protect the skin and secure the T-point during the first postoperative week. Staples are then used to approximate the rest of the skin closure. Skin closure is then performed with two-layer absorbable suture in the deep and superficial dermis. A drain is placed laterally. Sometimes the nipple will be tethered in a lateral, medial, or inferior position and will need to be released to fit into the keyhole pattern. The nipple–areola complex is retracted with a double hook and an Army-Navy retractor holds the skin in the keyhole back to allow release of the tethered dermis with cautery (Fig. 41.1G). The dermis can be safely scored halfway around the circumference of the areola, due to the robust blood supply of the central pedicle.
Representative cases are shown in Figs 41.2–41.5.

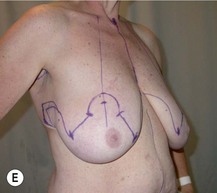

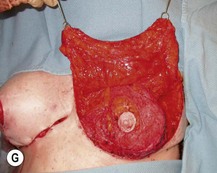










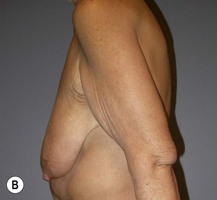
Fig. 41.2 A 57-year-old woman after 60 kg (130 lb) weight loss.
Reprinted with permission from: Rubin JP, Gusenoff JA, Coon D. Dermal suspension and parenchymal reshaping mastopexy after massive weight loss. Statistical analysis with concomitant procedures from a prospective registry. Plast Reconstr Surg 2009, 123(3):782–789.



1 Rubin JP, Khachi G. Mastopexy after massive weight loss: dermal suspension and selective auto-augmentation. Clin Plast Surg. 2008;35:123-129.
2 Rubin JP. Mastopexy in the massive weight loss patient: dermal suspension and total parenchymal reshaping. Aesth Surg J. 2006;26:214-222.
3 Graf RM, Mansur AEC, Tenius FP, et al. Mastopexy after massive weight loss: extended chest wall-based flap associated with a loop of pectoralis muscle. Aesth Plast Surg. 2007;32:371-374.
4 Hamdi M, Van Landuyt K, Blondeel P, et al. Autologous breast augmentation with the lateral intercostal artery perforator flap in massive weight loss patients. J Plast Reconstr Aesth Surg. 2007;62:65-71.
5 Hurwitz DJ, Agha-Mohammadi S. Postbariatric surgery breast reshaping: the spiral flap. Ann Plast Surg. 2006;56:481-486.
6 Kwei S, Borud LJ, Lee BT. Mastopexy with autologous augmentation after massive weight loss: the intercostal artery perforator (ICAP) flap. Ann Plast Surg. 2006;57:361-365.
7 Losken A, Holtz DJ. Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotation-advancement technique. Plast Reconstr Surg. 2007;120:1060-1068.
8 Regnault P. Breast ptosis: definition and treatment. Clin Plast Surg. 1976;3:193-203.
9 Song AY, Jean RD, Hurwitz DJ, et al. A classification of contour deformities after bariatric weight loss: the Pittsburgh rating scale. Plast Reconstr Surg. 2005;116:1535-1544.
10 American Cancer Society. Detailed guide: breast cancer. Available at http://www.cancer.org/docroot/CRI/content/CRI_2_2_3X_How_is_breast_cancer_found_5.asp?sitearea, 2008. Accessed June 2 2009