Dental Emergencies
The most common dental emergencies result from inflammation, infection, or trauma.
Toothache (Pulpitis)
Treatment
1. If the offending carious lesion can be localized, first apply a piece of cotton soaked with eugenol (oil of cloves).
2. Place a temporary filling material, such as Cavit or zinc oxide-eugenol (ZOE) cement (intermediate restorative material [IRM]), into the lesion to protect the nerve. Softened candle wax can be used if necessary as a temporary filling material.
3. Administer a nonsteroidal antiinflammatory drug (NSAID) (e.g., ibuprofen 400 to 800 mg PO q6h prn).
4. If the episode of pain lasts longer, indicating a moderate pulpitis, fill the lesion as described earlier and give the patient a non-narcotic analgesic.
5. For severe pulpitis with continuous and severe pain, administer a local anesthetic and then evacuate the patient. You can achieve a nerve block with bupivacaine 2% with 1 : 200,000 epinephrine (Marcaine) that lasts for about 8 hours and does not produce central nervous system depression. Large doses of narcotics may not provide pain relief and might compromise the patient’s ability to participate in evacuation.
6. In extraordinary circumstances, locate the offending tooth, expose the pulp, remove the inflamed tissue with a barbed hook, and cover the lesion with temporary filling material.
Periapical Osteitis
Inflammation of the supporting structures at the root of a tooth.
Temporomandibular Disorders
Myofascial Pain and Dysfunction
Signs and Symptoms
Mandibular Dislocation
Treatment
1. Place the rescuer’s thumbs on the patient’s lower molars and move the mandible down, then posteriorly, and then up. The thumbs should be padded to prevent bites as the jaw pops back into its socket.
2. Alternatively, rest the rescuer’s palms on the mandible and wrap the fingers along the occlusal surface of the mandibular teeth. Rock the hands posteriorly and down, sliding the mandibular condyle back into the TMJ.
3. If muscle spasm is severe, sedation might be necessary.
4. After reduction of the mandible, the patient must avoid wide mouth opening.
Infections
Treatment
1. Apply a topical steroid (fluocinonide 0.05%) mixed with oral benzocaine 20% over each ulcer six to eight times per day. Do not mix the medications until you are ready to apply them, and do not rub the mixture into the lesions.
2. Other options include premixed preparations, such as triamcinolone (Kenalog) in oral benzocaine 20%.
3. Tincture of benzoin or a topical anesthetic (viscous lidocaine 2%) can be applied to the dried surface of the ulcer before meals and at bedtime.
Viral Infections
Signs and Symptoms
1. Prodrome of tingling or paresthesia in the area
2. Yellow, fluid-filled vesicles that rupture to leave ragged ulcers on the lip, palate, tongue, and buccal mucosa
3. Primary herpetic gingivostomatitis is characterized by a thin zone of red, painful gingiva just next to the teeth. Sore throat, lymphadenopathy, and low-grade fever are also present
Treatment
1. Administer valacyclovir (Valtrex) 2 g PO q12h for 1 day as soon as the patient becomes aware of a prodromal “tingle” or paresthesia.
2. For herpetic gingivostomatitis, use soothing mouth rinses, such as warm saline or a mixture of equal amounts of diphenhydramine (Benadryl) elixir (12.5 mg per 5 mL), kaolin/pectin (Kaopectate), and viscous lidocaine 2%. Rinse with and expectorate 5 mL q2h.
Apical Abscess and Cellulitis
Treatment
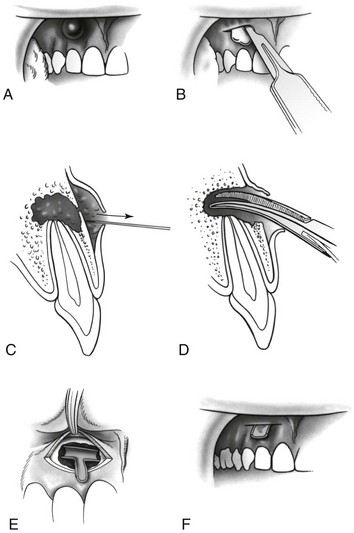
1. Incision and drainage is the treatment of choice (Fig. 34-1).
a. Infiltrate the area with a local anesthetic. Adequate anesthesia may also be obtained by applying cold (ice or snow) to the area to be incised.
b. Make an incision at the point of maximum fluctuance down to bone in one swift movement.
c. Spread the incision with a hemostat or knife handle.
d. Place a T-shaped drain into the wound. Drain material can be improvised from a piece of surgical glove or gauze dressing.
2. Administer warm saline rinses q2h, and an analgesic as needed for pain.
3. If incision and drainage cannot be performed, administer an oral antibiotic such as penicillin or erythromycin (see Appendix H).
4. Evacuate the patient and seek dental care, because this condition often requires dental extraction and antibiotics.
Pericoronitis
Treatment
1. Initiate field treatment, which consists of curettage of the area around the tooth and under the flap. In the absence of proper dental instruments, use a small, curved hemostat.
2. Irrigate the space under the flap with disinfected water or sterile normal saline solution using a syringe and catheter.
3. Begin hot saline rinses q2h, and administer an oral antibiotic such as penicillin or erythromycin (see Appendix H).
Deep Fascial Space Infection
Signs and Symptoms
3. Swelling minimal because of the overlying muscle mass
4. Submandibular space infection (Ludwig’s angina) that produces elevation of the tongue and brawny, painful edema of the submandibular area
5. Continued swelling that restricts neck motion and produces dysphonia, odynophagia, and drooling; possible progression to acute airway obstruction and asphyxia
Treatment
1. Be aware that airway management with early intubation or cricothyroidotomy may be necessary.
2. Administer an intravenous antibiotic (penicillin, 2 million units) or oral antibiotic (penicillin, 1000 mg) if intravenous therapy is not available.
3. Evacuate the patient immediately to the nearest medical facility.
Trauma
See Table 34-1 for dental trauma definitions.
Table 34-1
| CONDITION | SIGNS AND SYMPTOMS | TREATMENT |
| Concussion | Fully rigid tooth but has sustained trauma | Observation only |
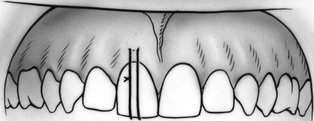
| Subluxation | Loose tooth but in correct position | Splint |
| Extrusive luxation | Loose or rigid tooth displaced outward from occlusal surface | Pad contralateral occlusal surface, analgesia, dental follow-up |
| Lateral luxation | Loose or rigid tooth displaced laterally | Local anesthesia, reduction to anatomic position |
| Intrusive luxation | Loose or rigid tooth displaced inward from occlusal surface | Analgesia, dental follow-up |
| Avulsion | Tooth completely missing from alveolar socket | Locate missing tooth, and rinse in water or saline, but do not scrub. Replace in socket if possible and splint. If unable to replace, transport in saline or saliva and evacuate to immediate dental care |
| Fracture | Irregular surface with exposed dentin or pulp | File rough edges. Cover exposed dentin or pulp with Cavit, zinc oxide-eugenol cements, or warm wax |
Root Fracture
Extrusive Luxation
Treatment
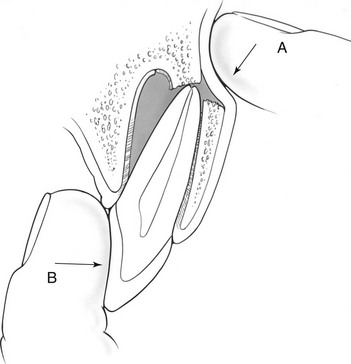
1. Reposition the tooth with gentle, steady pressure, allowing time to displace the blood that has collected into the apical region of the socket.
2. Observe the patient’s occlusion as a guide to proper reduction. If the patient bites and contacts only the injured tooth, further positioning is necessary.
3. If the patient is unable to close the occlusal surface normally, place soft padding on the contralateral occlusal surface for comfort.
Lateral Luxation
Total Avulsion
Treatment
1. Clean the debris off the tooth by rinsing gently (do not scrub) with either saline solution or milk. Handle the tooth only by the crown.
2. Remove any clotted blood from the socket with gentle irrigation and suction.
3. Gently replace the tooth in the socket with slow, steady pressure.
4. Splint or suture the tooth in place.
5. If the tooth cannot be replaced immediately, store it in balanced Hank’s solution, tissue culture medium, physiologic saline solution, white milk, or saliva, in that order of preference.
6. Relieve bleeding by placing a moistened tea bag into the socket that is bleeding.
7. Do not replace children’s primary (non-adult) teeth as this can cause complications with adult tooth eruption and alignment.
Dental First-Aid Kit
1. Cavit is a temporary filling. Squeeze a small amount of the material from the tube, and place it in the tooth. Wet a dental packing instrument or cotton-tipped applicator or toothpick to prevent sticking, and pack the Cavit well. Then remove any excess. Have the patient bite to displace material that would interfere with occlusion. The filling material will set in a few minutes after contact with saliva.
2. Zinc oxide-eugenol cements consist of a liquid and a powder. Start with two drops of the liquid, and begin mixing in the powder. Keep adding powder to make a consistency that is not sticky yet will hold together. Dip the instruments in some powder to keep the mixture from sticking. Insert and shape the filling material as explained earlier.