Definition and Prevalence of Dentofacial Deformities
The term dentofacial deformity refers to significant deviations from normal proportions of the maxillomandibular complex that also negatively affect the relationship of the teeth within each arch and the relationship of the arches with one another (occlusion).2,4,5,8,11,14,15,17,18,21,22,25,27,31,36,37,40,52,54 The affected individual will have varied degrees of compromise in head and neck functions related to breathing, swallowing, speech articulation, chewing, and lip closure/posture. Effects on the temporomandibular joints, the periodontium, and the teeth themselves may also occur.24,25,28,33,34,38,55 The presenting facial disproportion will, in general, have at least some negative effects on psychosocial health.16,39,56,57
Racial variations with regard to the incidence of facial dysmorphology and the resulting malocclusion are also known to occur.59,64 Definitions of acceptable levels of deviation from normal continue to be questioned by both clinicians and patients.7,26,30,32,35,58,61,62 Over the years, the National Center for Health Statistics has collected data and the Research Council has held multidisciplinary conferences to focus attention on these issues.6,12,19,20,29,41-51,53,63
Surgery to reposition the jaws (i.e., an orthognathic procedure) as part of an interdisciplinary approach is often recommended to manage the related skeletal, dental, and soft-tissue dysfunctions and concerns.3,13,23,60,66 Speech therapy, dental work, orthodontics, and surgical procedures alone are generally inadequate as isolated treatment modalities.
Facial disproportion observed in a child may at times be self-correcting. For example, apparent mandibular deficiency that is present before the pubertal growth spurt may normalize. In some cases, the maxilla or mandible may be induced to grow a few millimeters, more or less, through dentofacial orthopedics. However, major transformation of the jaws with the use of growth-modification techniques cannot be expected. Proffit has pointed out that, even with the well-intended aim of dentofacial orthopedics to alter jaw growth, as a result of anchorage requirements and biologic realities coupled with the practical desire of the orthodontist to “correct the occlusion,” the treatment generally results in the displacement of the teeth in the direction of correcting the occlusion rather than the jaw relationships.53 The term dental compensation for the skeletal discrepancy is universally understood to explain this treatment approach. Orthodontic-introduced dental compensation for the occlusion will hinder the eventual skeletal (orthognathic) correction if this is later required or requested.
Informed consent from the patient or his or her family is strongly recommended before embarking on a compromised treatment plan. For example, if a child is recognized to have an underdeveloped mandible with a Class II malocclusion and standard growth modification is attempted, it may be difficult for the orthodontist to prevent at least some retraction of the upper incisors and the forward displacement of the lower teeth. This may result in an “improved” occlusion, but it may also potentially involve long-term negative effects on periodontal health (e.g., labial cortical bone stripping), the airway (e.g., retroglossal obstruction), and facial aesthetics (e.g., a weak profile).39,56,57 It also compromises the option of an orthognathic correction with the need to first “undo” the dental compensations through “redo” orthodontics (Fig. 3-1).

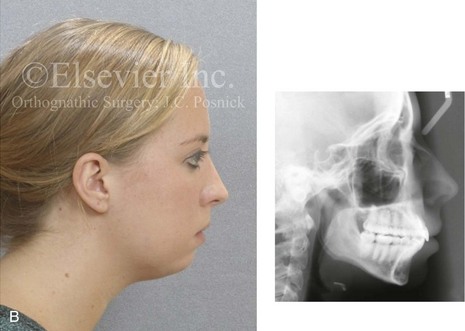
Figure 3-1 A 21-year-old woman with a primary mandibular deficiency growth pattern requested a surgical consultation for a “weak chin.” During her early teenage years, she underwent unsuccessful growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach. The mandibular anterior dentition was flared forward. The history was significant for restless sleeping and a degree of daytime fatigue, which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a Class II malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a “chin implant” would be effective to manage the aesthetic effects. A sleep study confirmed obstructive sleep apnea (respiratory disturbance index = 18/hour). An orthognathic approach (Le Fort I, Sagittal splits, Osseous genioplasty) with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.
In the growing child who presents with a Class II malocclusion pattern, an active treatment approach is often offered by the orthodontist. This approach may attempt to alter jaw growth and to correct the occlusion by means of the following: (1) functional appliance use (e.g., Frankel, Twinblocks) to stimulate sagittal growth of the mandible; (2) the possible extraction of maxillary premolars with orthodontic incisor retraction; (3) the use of headgear to restrain maxillary sagittal growth; and (4) the orthodontic forward displacement of the lower anterior teeth (Fig. 3-2). With the use of this approach, favorable facial results will be seen in only a very specific patient subgroup that includes those patients with true maxillary dental protrusion and a limited degree of mandibular retrusion. In these cases, the extraction of maxillary premolars with the retraction of the incisors to a corrected inclination in combination with the minimal forward displacement of the lower teeth may result in both favorable occlusion and acceptable facial aesthetics.
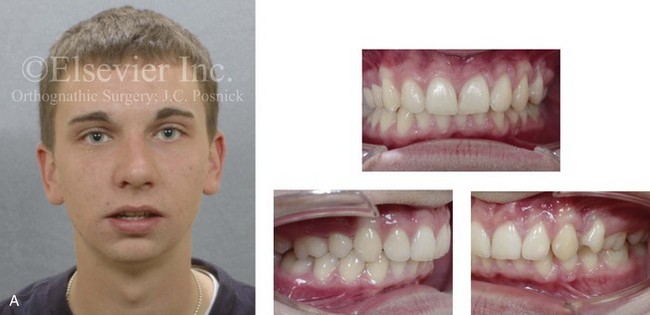

Figure 3-2 A 20-year-old man with a primary mandibular deficiency growth pattern requested a surgical consultation for a “weak chin.” During his early teenage years, he underwent unsuccessful growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach that included maxillary first bicuspid extractions to retract the anterior teeth. In addition, the mandibular anterior dentition was flared forward. His history was significant for heavy snoring, restless sleeping, and a degree of daytime fatigue, all of which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a molar Class II deep bite malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a “chin implant” would be effective to manage the aesthetic effects. A sleep study was recommended. An orthognathic approach (Le Fort I, Sagittal splits, osseous genioplasty) with redo orthodontic treatment was suggested as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.
Prevalence of Jaw Deformities and Malocclusion
U.S. Population Survey
As part of a large-scale evaluation of the health of the U.S. population, a National Health and Nutrition Examination Survey (NHANES III) was carried out between 1989 and 1994.53 Starting with a sampling of 14,000 individuals, estimates of the incidence of malocclusion and its severity were made. The sample of individuals was carefully selected to provide weighted estimates for an approximate 150,000,000 people between the ages of 8 and 50 years who were members of black, white, and Latino American racial and ethnic groups. Those individuals outside of that age range (i.e., those younger than 8 years and older than 50 years), Native Americans, those living on military reservations, and some other specific population groups were excluded from this study. Data collected included the following:
• The alignment of the incisor teeth
• The horizontal position of the incisors (i.e., overjet or reverse overjet)
• The vertical overlap of the incisors (i.e., deep bite or open bite)
The Horizontal/Sagittal Dimension
This study provides useful information about preadolescent children (8 to 11 years old), adolescents (12 to 17 years old), and adults (18 to 50 years old) with reference to how the teeth fit together and, by inference, the prevalence of dentofacial deformities. When interpreting the data collected for the NHANES III study, it is important to consider that at least some degree of dental compensation for an existing jaw deformity normally occurs during growth and is expected to have been present at the time that the study measurements were taken. Therefore, it is unlikely that either the moderate or greater values of positive overjet or the mild to moderate values of negative overjet measured in the NHANES III study were found in individuals with “normal” jaw relationships. It would be safe to assume that any individual in the study with more than 7 mm of positive overjet has a jaw discrepancy that is characterized by mandibular deficiency (see Chapter 19). In addition, those with 2 mm or more of reverse overjet are assumed to have elements of maxillary deficiency in combination with relative mandibular excess (see Chapter 20).
The Vertical Dimension
According to the NHANES III study, only half of the U.S. population has an ideal vertical relationship of the incisors (i.e., 0- to 2-mm overbite). In the others, a deep bite in combination with mandibular deficiency or maxillomandibular deficiency is more prevalent among whites, and an open bite in combination with bimaxillary dental protrusion is more frequent among blacks. Interestingly, either a severe deep bite (≥5 mm) or a marked open bite (≥2 mm) was present in approximately 20% of children and 13% of adults. The extreme values of open bite that were measured in the study group likely represent either a long face growth pattern (i.e., vertical maxillary excess or mandibular deficiency; see Chapter 21) or bimaxillary dental protrusion (see Chapter 24). Interestingly, significant anterior open bite as part of a long face growth pattern is more prevalent among white Americans. The extreme values of deep bite in the studied individuals are likely to represent either a short face growth pattern (i.e., maxillomandibular deficiency; see Chapter 23) or a primary mandibular deficiency. Significant degrees of vertical discrepancy (deep bite or open bite) at the incisors ideally benefit from orthognathic surgery. When dental compensating orthodontic treatment is instituted rather than orthognathic correction, compromised facial aesthetics, occlusal instability, and periodontal sequela are more likely to occur.
U.K. Population Survey
An Index of Treatment Need was developed by the Swedish Dental Board to classify the severity of dental findings by the worst presenting characteristic.33 This method tends to downplay the specific alignment of individual teeth. It is a classification system that looks more globally at facial proportions and head and neck function than at isolated dental details. For example, if you have a mild irregularity of the incisors and only a mildly excessive overjet, you are judged to have only a mild problem. In other words, the impact on the individual is not judged to be more severe, because there is a combination of two mild occlusal deviations from normal. Alternatively, if you have a 10-mm overjet, even if the teeth are aligned in each jaw, you are judged to have a severe problem.
Brook and Shaw made modifications to the Swedish classification and developed the Index of Treatment Need for malocclusion to be used as a grading system of dental health and functional indications for treatment.9,10 The first part of their study was derived from the direct examination of occlusion and dental alignment. They defined five grades of treatment need, with Grade 1 representing little or no need for treatment and Grade 5 representing great need for treatment. The authors attempted to establish meaningful values for cutoff points between grades for each occlusal trait and to determine the quantifiable threat to the dentition if no treatment is provided. Grades 4 and 5 have characteristics that can result in a more severe impact on both facial aesthetic and dental aspects. These characteristics include the following:
• Defects of cleft lip and palate*
• Reverse overjet of more than 3.5 mm with reported masticatory and speech difficulties*
• Extreme lateral or anterior open bites (>4 mm)*
• Increased overjet (>6 mm but ≤9 mm)*
• Reverse overjet (>3.5 mm with no masticatory or speech difficulties)*
• Reverse overjet of more than 1 mm with reported masticatory or speech difficulties
• Posterior crossbite with no functional occlusal contacts in one or both buccal segments
• Increased and complete overbite with gingival or palatal trauma
• Anterior or posterior crossbites with more than 2 mm of centric relation/centric occlusion discrepancy
• Severe contact point discrepancy (>4 mm)
• Less extensive hypodontia (e.g., one tooth per quadrant requiring preprosthetic orthodontics)
• Partially erupted teeth that are tipped and impacted against adjacent teeth
The second part of the authors’ overall assessment of treatment priority was to record the aesthetic impairment contributed by the malocclusion. The authors used the Standard Continuum of Aesthetic Need (SCAN) index as a rating scale.16 The SCAN scale was constructed with the use of dental photographs from 1000 12-year-old children that were collected as part of a large multidisciplinary survey. Six non-dental judges rated these photographs on a 10-point visual analog scale. Both the aesthetic impairment component and the dental health component were part of the overall study.
The distribution of ratings for the Dental Health Indications Study conducted by Brook and Shaw were obtained from examination subjects (n = 222) who, at minimum, were felt to have a malocclusion to the extent that referral to a regional orthodontic center for advice or treatment was recommended.10 Each study patient was then examined, and their available radiographs were reviewed by skilled clinicians. Both components of the index (i.e., aesthetic and dental) were applied, and the patients were also asked to give their own rating according to the SCAN scale. Interestingly, there was a high correlation (confirmed by intraexaminer and interexaminer error testing of the findings) between both components (i.e., aesthetic and dental) of the study.
The study results indicated that 19.2% of the subjects (44 of 222) were considered to have Grade 5 conditions. Interestingly, the distribution of ratings from Grades 1 through 5 that were obtained from the examination of a matched, random, unselected group of schoolchildren (n = 333) indicated that only 5.1% fell in the Grade 5 category. A Grade 5 score indicates severe malocclusion with a high need for treatment to establish dental health. Most of the traits listed as Grade 5 cannot be corrected with orthodontics alone, and orthognathic surgery would likely be recommended or at least considered. The Shaw study indicates that, in the United Kingdom, more than 5% and as high as 19% of children who have been referred to an orthodontist for evaluation are likely to have a malocclusion to the extent that orthodontics alone would not be the first choice for full correction (i.e., there is a need for orthognathic surgery).10
Orthognathic Procedures Performed on Hospitalized Patients in the United States
Venugoplan and colleagues completed a study with the aim of providing a nationally representative estimate of the number and type of orthognathic procedures performed on hospitalized patients in the United States.65 Their data was obtained from the Nationwide Inpatient Sample (NIS) database from 2008 and included all hospitalizations for orthognathic procedures. The procedures were identified via the procedure code listed in the International Classification of Diseases, 9th Revision, Clinical Modification.1 The NIS database is sponsored by the Agency for Healthcare Research and Quality, a division of the Department of Health and Human Services of the U.S. government. Ten thousand three hundred and forty-five (10,345) hospitalizations for orthognathic procedures were identified as occurring during the 2008 calendar year. The average age of these patients was 26.7 years, and female patients comprised 56.2% of all those who were hospitalized for these procedures. Whites, blacks, Hispanics, Asians, Pacific Islanders, and Native Americans and other races constituted 71.9%, 4.9%, 12.6%, 5.6%, 0.4%, and 4.6% of the hospitalizations, respectively. Private insurance plans were the primary payers (77.3%). Government insurance plans (i.e., Medicare and Medicaid) accounted for 13.4% of the patient mix, whereas 3.5% of patient paid privately (i.e., out of pocket), without the benefit of medical insurance.
References
1. Agency for Healthcare Research and Quality. NIS Database Documentation: The Nationwide Inpatient Sample (NIS). www. hcup-us. ahrq. gov/db/nation/nis/nisdbdocumentation. jsp.
2. Allwright, WC, Bundred, WH. A survey of handicapping dentofacial anomalies among Chinese in Hong Kong. Int Dent J. 1964; 14:505–519.
3. American Association of Oral and Maxillofacial Surgeons. Residency procedure report. Chicago: American Association of Oral and Maxillofacial Surgeons; 2007.
4. Angle, EH. Classification of malocclusion. Dent Cosmos. 1899; 41:248–264.
5. Ast, D-B, CMOS, JP, Cons, NC. The prevalence and characteristics of malocclusion among senior high school students in upstate New York. Am J Orthod. 1965; 51:437–445.
6. Baume, LJ, Horowitz, HS, Summers, CJ, et al. A method of examining occlusal traits developed by the FDI commission on classification and statistics for oral conditions (COCSTOQ). Int Dent J. 1973; 23:530–537.
7. Bjork, A, Krebs, AA, Solow, B. A method for epidemiological registration of malocclusion. Acta Odontol Scand. 1964; 22:27–41.
8. Bolton, WA. Disharmony in tooth size and its relation to the analysis and treatment of malocclusion. Angle Orthod. 1958; 28:113–130.
9. Brook PH: The development of an orthodontic treatment priority index. MSc thesis. University of Manchester, 1987.
10. Brook, PH, Shaw, WC. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989; 11:309–320.
11. Carlos, JP. Evaluation of indices of malocclusion. Transactions of the Second FDI Conference on Oral Epidemiology, Epidemiological Assessment of Dentofacial Anomalies. 1969; 20(4):606–615.
12. Cirainger RM: The statistical basis for international dental epidemiology. World Health Organization Document No. PA/98. 6
13. DeLuke, DM. Orthognathic surgery: the state of the art. N Y State Dent J. 1998; 64:30.
14. Draker, HL. Handicapping labio-lingual deviations, a proposed index for public health purposes. Am J Orthod. 1960; 46:295–305.
15. Emrich, RE, Brodie, AG, Blayney, JR. Prevalence of class I, class II, and class III malocclusions (Angle) in an urban population: an epidemiological study. J Dent Res. 1965; 44:947–953.
16. Evans, MR, Shaw, WC. Preliminary evaluation of an illustrated scale for rating dental attractiveness. Eur J Orthod. 1987; 9:314–318.
17. Foster, TD, Walpole Day, AJ. A survey of malocclusion and the need for orthodontic treatment in a Shropshire school population. Br J Orthod. 1973; 3:73–78.
18. Gardiner, JH. A survey of malocclusion and some aetiological factors in 1000 Sheffield school children. Dent Practit. 1956; 6:187–201.
19. Grainger, RM. Indexing handicapping malocclusions. Working paper for meeting of Expert Committee on Dental Health. Geneva: World Health Organization; 1961.
20. Grainger, RM. Orthodontic treatment priority index. Public Health Service Publication No. 1000, Series 2, No 25. Washington, DC: U. S. Government Printing Office; 1967.
21. Gravely, JF, Johnson, DB. Angle’s classification of malocclusion: an assessment of reliability. Br J Orthod. 1974; 3:79–86.
22. Grewe, JM, Cervenka, J, Shapiro, BL, et al. Prevalence of malocclusion in Chippewa Indian children. J Dent Res. 1968; 47:302–305.
23. Hausamen, JE. The scientific development of maxillofacial surgery in the 20th century and an outlook into the future. J Craniomaxillofac Surg. 2001; 29:2–21.
24. Haynes, S. Discontinuation of orthodontic treatment in the General Dental Service in England and Wales 1972-1979. Br Dent J. 1982; 152:127–129.
25. Helm, S, Kreiborg, S, Barlebo, J, et al. Estimates of orthodontic treatment need in Danish schoolchildren. Community Dent Oral Epidemiol. 1975; 3:136–142.
26. Helm, S. Intra-examiner reliability of epidemiological registrations of malocclusion. Acta Odontol Scand. 1977; 35:161–165.
27. Horup, N, Melsen, B, Terp, S. Relationship between malocclusion and maintenance of teeth. Community Dent Oral Epidemiol. 1987; 15:74–78.
28. Jarvinen, S. Traumatic injuries to upper permanent incisors related to age and incisal overjet. Acta Odontol Scand. 1979; 37:335–338.
29. Kelley, JE, Sanchez, M, Van Kirk, GE. An assessment of the occlusion of teeth of children 6-11 years. U. S. Department of Health, Education, and Welfare, Public Health Service publication (HRA) No. 74-1612. Washington, DC: National Center for Health Statistics; 1973.
30. Kelley, JE, Harvey, CR. An assessment of the occlusion of teeth of youths 12-17 years. U. S. Department of Health, Education, and Welfare, Public Health Service publication (HRA) No. 77-1644. Washington, DC: National Center for Health Statistics; 1977.
31. Kelly, JF, Helfrick, JF, Smith, DW, Jones, BL. A survey of oral and maxillofacial surgeons concerning their knowledge, beliefs, attitudes, and behavior relative to parameters of care. J Oral Maxillofac Surg. 1992; 50:50–58.
32. Lau, D, Griffiths, G, Shaw, WC. Reproducibility of an index for recording the alignment of individual teeth. Br J Orthod. 1984; 11:80–84.
33. Linder-Aronson, S. Orthodontics in the Swedish Public Dental Health System. Trans Eur Orthod Soc. 1974; 233–240.
34. Lundstrom, A. Need for treatment in cases of malocclusion. Trans Eur Orthod Soc. 1977; 53:111–123.
35. Malmgren, O, Studies on the need and demand for orthodontic treatment. Swed Dent J Suppl. 1980;(6):1–121.
36. Massler, M, Frankel, JM. Prevalence of malocclusion in children aged 14-18 years. Am J Orthod. 1951; 37:751–768.
37. Mills, LF. Epidemiologic studies of occlusion: IV. The prevalence of malocclusion in a population of 1,455 school children. J Dent Res. 1966; 45:332–336.
38. Mohlin, B, Thilander, B. The importance of the relationship between malocclusion and mandibular dysfunction and some clinical applications in adults. Eur J Orthod. 1984; 16:192–204.
39. Montegi, E, Hatch, JP, Rugh, JD, Yamaguchi, H. Health-related quality of life and psychosocial function 5 years after orthognathic surgery. Am J Orthod Dentofacial Orthop. 2003; 124:138–143.
40. Moyers, RE, van der Linden, FPGM, Riolo, ML, et al. Standards of human occlusal development. Ann Arbor, MI: University of Michigan Center for Human Growth and Development; 1976.
41. National Center for Health Statistics. Volume of dental visits, United States, July 1963-June 1964. Vital and Health Statistics. PHS Pub No 1000-Series 10-No 23. Public Health Service. Washington, DC: U. S. Government Printing Office; 1965.
42. National Center for Health Statistics. Decayed, missing, and filled teeth in adults. Vital and Health Statistics. PHS Pub No 1000-Series 11-No 23. Public Health Service. Washington, DC: U. S. Government Printing Office; 1967.
43. National Center for Health Statistics. Plan, operation and response results of a program of children’s examinations. Vital and Health Statistics. PHS Pub No 1000-Series l-No 5. Public Health Service. Washington, DC: U. S. Government Printing Office; 1967.
44. National Center for Health Statistics. The orthodontic treatment priority index. Vital and Health Statistics. PHS Pub No 1000-Series 2-No 25. Public Health Service. Washington, DC: U. S. Government Printing Office; 1967.
45. National Center for Health Statistics. Plan and operation of a health examination survey of US youths 12-17 years of age. Vital and Health Statistics. PHS Pub No 1000-Series l-No 8. Public Health Service. Washington, DC: U. S. Government Printing Office; 1969.
46. National Center for Health Statistics. Decayed, missing, and filled teeth among children. Vital and Health Statistics. Series 11-No 106. DHEW Pub No (HSM) 72-1003. Health Services and Mental Health Administration. Washington, DC: U. S. Government Printing Office; 1971.
47. National Center for Health Statistics. Dental visits, volume and interval since last visit, United States, 1969. Vital and Health Statistics. Series 10-No 76. DHEW Pub No (HSM) 72-1066. Health Services and Mental Health Administration. Washington, DC: U. S. Government Printing Office; 1972.
48. National Center for Health Statistics. Plan and initial program of the health examination survey. Vital and Health Statistics. Series l-No 4. DHEW Pub No (HRA) 74-1038. Health Resources Administration. Washington, DC: U. S. Government Printing Office; 1973.
49. National Center for Health Statistics. An assessment of the occlusion of the teeth of children 6-11 years, United States. Vital and Health Statistics. Series 1l-No 130. DHEW Pub No (HRA) 74-1612. Health Resources Administration. Washington, DC: U. S. Government Printing Office; 1973.
50. National Center for Health Statistics. Decayed, missing, and filled teeth among youths 12-17 years, United States. Vital and Health Statistics. Series 1l-No 144. DHEW Pub No (HRA) 75-1626. Health Resources Administration. Washington, DC: U. S. Government Printing Office; 1974.
51. National Center for Health Statistics. Vital statistics of the United States, 1971, Vol. I, Nationality. DHEW Pub No (HRA) 75-1113. Health Resources Administration. Washington, DC: U. S. Government Printing Office; 1975.
52. Newman, GV. Prevalence of malocclusion in children six to fourteen years of age and treatment in preventable cases. J Am Dent Assoc. 1965; 52:566–575.
53. Proffit, WR, Fields, HW, Jr., Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES III survey. Int J Adult Orthod Orthognath Surg. 1998; 13:97–106.
54. Salzmann, JA. Handicapping malocclusion assessment to establish treatment priority. Am J Orthod. 1968; 54:749–765.
55. Sandali, T. Irregularities of the teeth and their relation to the periodontal condition with particular reference to the lower labial segment. Trans Eur Orthod Soc. 1973; 319–333.
56. Shaw, WC, Addy, M, Ray, C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dent Oral Epidemiol. 1980; 8:36–45.
57. Shaw, WC, Addy, M, Dummer, PMH, et al. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a strategy for investigation. Community Dent Oral Epidemiol. 1986; 14:60–64.
58. Singh, IJ, Savara, BS. Norms of size and annual increments of seven anatomical measures of maxillae in girls from 3 to 17 years of age. Angle Orthod. 1968; 36:312.
59. Siriwat, PP, Jarabak, JR. Malocclusion and facial morphology: is there a relationship? An epidemiologic study. Angle Orthod. 1985; 55:127–138.
60. Sullivan, SM. Orthognathic surgery dilemma: increasing access. J Oral Maxillofac Surg. 2011; 69:813–816.
61. Summers, CJ. The occlusal index: a system for identifying and scoring occlusal disorders. Am J Orthod. 1971; 57:552–567.
62. The American Association of Orthodontists. Study of the availability of orthodontists’ services. Am J Orthod. 1975; 68(3):326–338.
63. U. S. National Health Survey. Dental care, interval and frequency of visits, United States, July 1957-June 1958. PHS Pub No 584-1314. Public Health Service. Washington, DC: U. S. Government Printing Office; 1960.
64. Van Kirk, LE, Jr., Pennell, EH. Assessment of malocclusion in population groups. Am J Pub Health. 1959; 49(9):1157–1163.
65. Venugoplan, SR, Nanda, V, Turkistani, K, et al. Discharge patterns of orthognathic surgeries in the United States. J Oral Maxillofac Surg. 2012; 70:e77–e86.
66. Zins, JE, Bruno, J, Moreira-Gonzalez, A, et al. Orthognathic surgery: is there a future? Plast Reconstr Surg. 2005; 116:1442–1450.



