Chapter 53 Damage Control Trauma Care: Does It Save Lives or Make No Difference?
Controversy still exists about the early definitive treatment of fractures in patients with multiple injuries. Several authors in the 1980s supported the benefit of early intramedullary nailing of femoral shaft fractures.1–6 However, because of experimental and retrospective studies in the 1990s, concerns were raised about primary intramedullary nailing of the femur, sometimes referred to as early total care (ETC), especially in patients with associated chest and head injuries.7–9 The concept of “damage control orthopedics” (DCO) was then developed in the large trauma centers. This technique involves primary external skeletal fixation of the femoral fracture followed in a few days by definitive intramedullary nailing when the patient’s physiology has been completely corrected. Several authors have advocated delayed definitive treatment in the more recent literature.10–13 Since the 1990s, there has been an ongoing debate about early versus delayed definitive fracture fixation in femoral shaft fractures in the setting of polytrauma and when treating femoral shaft fractures in patients with multiple injuries regarding whether the reamed or the unreamed technique should be used.
Since the late 1980s, the assessment and treatment of the patient with multiple injuries has markedly improved. The establishment of highly specialized trauma centers for early intervention of life-threatening injuries, such as intrathoracic, intraabdominal, and intracranial injuries, has led to greater survival rates in these patients.14–17
EVIDENCE
Timing of Fracture Care in Patients with Multiple Trauma Injuries
Initial Clinical and Basic Science Research.
Several studies in the 1980s and 1990s found that early definitive care (less than 24 hours) leads to a decrease of morbidity and mortality.1–4,18–21 Most of the studies claimed that prevention of adult respiratory distress syndrome (ARDS), reduction of inflammatory mediators, and lower fat embolism rate were associated with early intramedullary nailing. In contrast, Pape and colleagues,7 in a retrospective review, found that although early intramedullary nailing of femoral shaft fractures in patients without chest injuries had a reduced risk for morbidity, the rates of ARDS and mortality were increased in patients with associated severe chest injuries treated with reamed intramedullary nailing within 24 hours of injury when compared with those who had delayed fracture fixation7 (Level of Evidence 3). Their suggestion was to consider alternate forms of femur fracture fixation or delayed definitive fixation in patients with severe chest injuries (Abbreviated Injury Scale [AIS] > 2). This then led to the development of the DCO concept. Other centers have advocated delayed definitive treatment in the more recent literature.10–13
Experimental Animal Studies.
Parallel to the clinical studies, several experimental animal studies investigated the effect of reamed or unreamed nailing of the femur and the tibia on the intramedullary pressure and the rate of fat embolization.8,9,22–28 In addition, Duwelius and researchers22 and Wolinsky and colleagues28 examined the effect of intramedullary nailing on pulmonary function in normal and contused lungs.
Most of the studies showed that intramedullary nailing of the femur increases the intramedullary pressure.8,9,22–24 No difference was found if a reamed or unreamed nailing procedure was used.22,23 Opening of the canal with an awl leads to the highest intramedullary pressure in studies by Heim and investigators24 and Duwelius and researchers.22 Marrow element extravasation and fat emboli are clearly associated with reamed and unreamed nailing of the femur.9,22–24,27,28
Manning and coworkers25 showed greater rates of fat release in intact femurs compared with fractured femurs and concluded that the fracture is responsible for the low incidence of pulmonary dysfunction in the clinical field. Duwelius and researchers22 found minimal pulmonary dysfunction in normal and contused lung in their sheep model with reamed or unreamed nailing of the femur. However, the reamed technique had a greater rate of fat emboli in the histologic analysis. Wolinsky and his group28 confirmed these results in 1998 in their sheep model with a reamed nailing procedure.
No evidence has been provided from this basic physiology research that reamed intramedullary nailing of the femur leads to greater pulmonary dysfunction than unreamed nailing. However, manipulation of the medullary canal does have a negative effect on pulmonary physiology.
Immunologic Response Studies.
Another field of interest is the systemic inflammatory response syndrome (SIRS) score of patients with multiple injuries related to the time of treatment. Several studies since the early 1990s have shown that the inflammatory response correlates with the severity of the injury, patient outcome, and mortality.29–36 However, only two studies have focused on the comparison of early versus delayed fixation.32,35 Pape and colleagues35 show in their prospective, randomized, multicenter study with 35 patients from 2003 that certain interleukin levels (IL-6 and IL-8) are significantly increased in the primary intramedullary fixation group. Both groups were similar regarding age, injury severity score (ISS), AIS, and Glasgow Coma Scale (GCS). However, no difference was found in the IL-1 level and in the incidence of ARDS, sepsis, and multiorgan failure (Level of Evidence 2).
The second study that is from the same group, reported by Harwood and colleagues32 in 2005, looked retrospectively at 174 patients and found a greater SIRS score in the early fixation group despite having significantly lower ISSs, and fewer head and chest injuries. They also had longer intensive care unit (ICU) stays, higher ARDS rates, and more multiorgan failures. Although the authors’ conclusion that DCO does not add additional detrimental inflammatory response to the patient seems clear, the study did not demonstrate that the greater SIRS score in the early definitive fixation group will lead to more complications (Level of Evidence III).
Chest Injuries and Femur Fractures.
The benefits of early definitive fracture fixation in patients with associated chest injuries have been demonstrated repeatedly.1,4,18–21,37–43 In contrast, Pape and colleagues7 were the first to demonstrate in their study from 1993 that early reamed intramedullary nailing in patients with severe chest injuries (AIS > 2) increased the risk for ARDS and death. In the same study, early fixation without chest injury was associated with decreased morbidity.
Comparison between studies is difficult. One main difficulty is the definition of the severity of chest trauma. In most studies, an AIS score of greater than 2 is considered to be a severe chest injury. In several studies, however, the AIS is either not mentioned or is indicated as 2 or lower.1,19, 38, 44 Another difficulty is the great variety of the ISSs in the studies. Most studies use an ISS of greater than 18 as a criterion for inclusion.1,3, 7, 20, 37, 40 However, often the ISS was significantly different across studies and across the two treatment groups.39
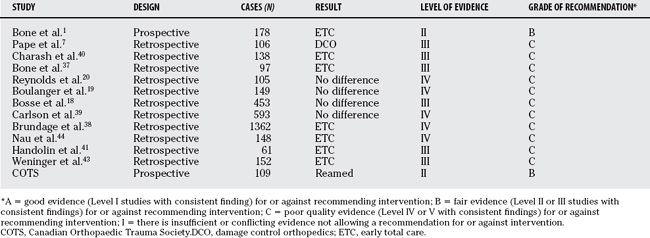
As mentioned previously and as shown in Table 53-1, most studies showed either no difference or better outcome in the early definitive fixation group.
Bone and coauthors1 showed in their prospective, randomized clinical study from 1989 that the incidence of pulmonary complications such as ARDS, pneumonia, and fat embolism is greater when the fracture fixation is delayed (Level of Evidence 2). This study was a prospective, randomized, clinical trial, but there were some limitations regarding the definition of the severity of the chest injury. In a retrospective review, similar results were presented from this group37 in 1995 with a chest AIS greater than 3 (Level of Evidence 3).
Interestingly, regarding Pape and colleagues’7 study, Charash and colleagues40 arrived at an opposite conclusion using the same study design in their study with 138 patients. A complication rate of 56% was observed in the patient group with delayed definitive fracture fixation, and associated severe chest injuries were compared with a rate of only 16% in the early fixation group (Level of Evidence 3).
In the more recent literature, Handolin and researchers41 and Weninger and colleagues43 compared patients with severe chest injuries (AIS ≥ 3) and femoral fractures treated with early intramedullary nailing with a group with severe chest injury but without long bone fractures (Level of Evidence 3). Both studies found that intramedullary nailing of the femur did not add any additional risk for ARDS, multiorgan failure syndrome, and mortality. The strength of Weninger and colleagues’43 study is the equal distribution in the ISS (39.5 vs. 38.3), the chest AIS (4.2 vs. 4.1), and the distribution of thoracic injuries.
The Canadian Orthopaedic Trauma Society45 report on a prospective, randomized, clinical trial that compared the rates of ARDS in patients with multiple trauma injuries who had their femur fractures treated primarily with either a reamed or an unreamed nail. The society found that there was no significant difference in the rate of ARDS (reamed, 4.8%; unreamed, 4.3%) or mortality between the two groups. The number of subjects was small and the event rate was low, indicating that further study may be necessary (Level of Evidence 2).
In summary, the literature is inconclusive regarding the optimal timing and type of fixation for femoral shaft fractures in association with severe chest injuries. It would appear from the early retrospective studies and from the Bone and coauthors’1 prospective randomized trial that early (within 24 hours) femur fracture fixation is advantageous in terms of morbidity and perhaps mortality. It is not clear whether the primary fixation should be external skeletal fixation (DCO) or definitive fixation (ETC). For patients treated with early definitive fixation, it would appear from the Canadian prospective randomized trial that there is no advantage to the unreamed technique over the reamed technique for pulmonary complication or mortality.
Timing of Fracture Care in Patients with Multiple Trauma Injuries: Head Injuries.
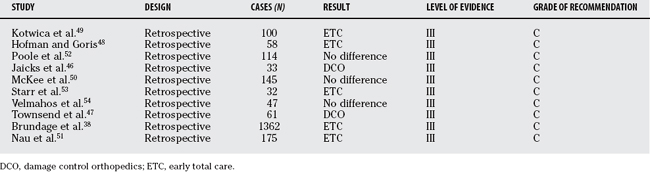
Both early and delayed femur fracture fixation in polytrauma victims with head injury has been supported (Table 53-2). Jaicks and investigators46 and Townsend and coworkers47 postulate that early fracture fixation exposed the patient to an unacceptable risk for secondary brain damage.
Jaicks and investigators46 retrospectively reviewed 33 patients with significant closed head injuries who were treated either with early (≤ 24 hours) or late fixation (>24 hours). He found that patients with early fixation received significantly more fluids in the first 48 hours, had a greater rate of intraoperative hypotension and hypoxia, and had an average discharge GCS that was lower compared with the delayed fixation group. In contrast, the neurologic complication rate, ICU stay, and hospital time was slightly higher in the delayed fixation group46 (Level of Evidence 3).
Sixty-one patients with moderate-to-severe closed head injuries in the retrospective review from Townsend and coworkers47 received intramedullary nailing of the femur in the first 2 hours, within 24 hours, or after 24 hours of admission to hospital. Compared with fracture fixation after 24 hours, the authors note an eight-fold increased risk for becoming hypotensive during fracture fixation when treated within the first 2 hours. The risk for hypotension was twice as high when fracture fixation occurred within 24 hours compared with treatment after 24 hours. The authors conclude that the risk for low intraoperative cerebral perfusion pressure remains important for at least 24 hours47 (Level of Evidence 3).
In contrast with these studies, there are numerous studies that not only shown no risk for early fracture fixation,38,48–54 but also show benefit in patients with ancillary chest trauma.38,53 Hofman and Goris48 found a better neurologic outcome based on the Glasgow Outcome Scale score and Brundage and colleagues38 based on a greater GCS score in the early fixation group in their studies from 1991 and 2002, respectively. None of the reviewed studies showed poorer neurologic outcome in the early fixation group. Hofman and Goris48 showed a three-fold greater mortality rate, and also Kotwica and colleagues49 and Riemer and coauthors55 demonstrate greater rates of mortality in the delayed fixation group. Several authors present no difference in the mortality rate.38,50, 51, 54
Velmahos and associates54 in their study from 1998 showed in 47 patients no difference of intraoperative hypotension and hypoxia in the early fixation group and found a trend to longer hospital and ICU stays after delayed treatment (Level of Evidence III). Also, Brundage and colleagues38 detected longer hospital stay and ICU length in the delayed fixation group, where McKee and coworkers50 and Nau and colleagues51 could not find a difference between the two groups.
Starr and colleagues53 found that delayed fixation was a strong predictor of pulmonary complications in 32 patients with mild-to-severe head injuries. Pulmonary complications were 48 times more likely in the delayed treatment group compared with early fixation. For each point increment in the chest AIS and head/neck AIS, the risk for pulmonary complications increased by 300% and 500%, respectively. The authors report no difference in the incidence of central nervous system complications with early or delayed treatment (Level of Evidence 3). Poole and coauthors52 state that the neurologic outcome is determined by the severity of the head injury, and that delayed fixation did not protect the injured brain.
AREAS OF UNCERTAINTY
If hemodynamic stability cannot be reached within the first hours of admission, temporary external fixation should be considered. The possible restriction of organ function caused by any surgical intervention in the vulnerable phase of hypovolemia and shock should always be kept in mind. Patient populations, resuscitation protocols and teams, orthopedic expertise, anaesthesia capabilities, and ICU resources vary from institution to institution. All of these are important to consider when making the decision about whether a polytrauma patient should have his or her femur treated with primary intramedullary nailing or with the DCO protocol. It would appear from the literature that both techniques are acceptable if the patient has been adequately resuscitated. Table 53-3 provides a summary of recommendations.
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Bone LB, Johnson KD, Weigelt J, Scheinberg R. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am. 1989;71:336-340.
2 Goris RJ, Gimbrere JS, van Niekerk JL, et al. Early osteosynthesis and prophylactic mechanical ventilation in the multitrauma patient. J Trauma. 1982;22:895-903.
3 Johnson KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: Effect of early operative stabilization of fractures. J Trauma. 1985;25:375-384.
4 Meek RN, Vivoda EE, Pirani S. Comparison of mortality of patients with multiple injuries according to type of fracture treatment—a retrospective age- and injury-matched series. Injury. 1986;17:2-4.
5 Riska EB, Myllynen P. Fat embolism in patients with multiple injuries. J Trauma. 1982;22:891-894.
6 Shapiro MB, Jenkins DH, Schwab CW, Rotondo MF. Damage control: Collective review. J Trauma. 2000;49:969-978.
7 Pape HC, Auf’m’Kolk M, Paffrath T, et al. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion—a cause of posttraumatic ARDS? J Trauma. 1993;34:540-548.
8 Sturmer KM, Schuchardt W. [New aspects of closed intramedullary nailing and marrow cavity reaming in animal experiments. II. Intramedullary pressure in marrow cavity reaming (author’s transl)]. Unfallheilkunde. 1980;83:346-352.
9 Wozasek GE, Simon P, Redl H, Schlag G. Intramedullary pressure changes and fat intravasation during intramedullary nailing: An experimental study in sheep. J Trauma. 1994;36:202-207.
10 Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg Am. 2000;82:781-788.
11 Roberts CS, Pape HC, Jones AL, et al. Damage control orthopaedics: Evolving concepts in the treatment of patients who have sustained orthopaedic trauma. Instr Course Lect. 2005;54:447-462.
12 Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: Damage control orthopedics. J Trauma. 2000;48:613-621.
13 Taeger G, Ruchholtz S, Waydhas C, et al. Damage control orthopedics in patients with multiple injuries is effective, time saving, and safe. J Trauma. 2005;59:409-417.
14 Feliciano DV, Mattox KL, Jordan GLJr. Intra-abdominal packing for control of hepatic hemorrhage: A reappraisal. J Trauma. 1981;21:285-290.
15 Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin North Am Aug. 1997;77:761-777.
16 Schweiberer L, Dambe LT, Klapp F. [Multiple injuries: Severity and therapeutic measures]. Chirurg. 1978;49:608-614.
17 Trentz O, Oestern HJ, Hempelmann G, et al. [Criteria for the operability of patients with multiple injuries (author’s transl)]. Unfallheilkunde. 1978;81:451-458.
18 Bosse MJ, MacKenzie EJ, Riemer BL, et al. Adult respiratory distress syndrome, pneumonia, and mortality following thoracic injury and a femoral fracture treated either with intramedullary nailing with reaming or with a plate. A comparative study. J Bone Joint Surg Am. 1997;79:799-809.
19 Boulanger BR, Stephen D, Brenneman FD. Thoracic trauma and early intramedullary nailing of femur fractures: Are we doing harm? J Trauma. 1997;43:24-28.
20 Reynolds MA, Richardson JD, Spain DA, et al. Is the timing of fracture fixation important for the patient with multiple trauma? Ann Surg. 1995;222:470-481.
21 Riska EB, von Bonsdorff H, Hakkinen S, et al. Prevention of fat embolism by early internal fixation of fractures in patients with multiple injuries. Injury. 1976;8:110-116.
22 Duwelius PJ, Huckfeldt R, Mullins RJ, et al. The effects of femoral intramedullary reaming on pulmonary function in a sheep lung model. J Bone Joint Surg Am. 1997;79:194-202.
23 Heim D, Regazzoni P, Tsakiris DA, et al. Intramedullary nailing and pulmonary embolism: Does unreamed nailing prevent embolization? An in vivo study in rabbits. J Trauma. 1995;38:899-906.
24 Heim D, Schlegel U, Perren SM. Intramedullary pressure in reamed and unreamed nailing of the femur and tibia—an in vitro study in intact, human bones. Injury. 1993;24(suppl 3):S56-S63.
25 Manning JB, Bach AW, Herman CM, Carrico CJ. Fat release after femur nailing in the dog. J Trauma. 1983;23:322-326.
26 Oztuna V, Ersoz G, Ayan I, et al. Early internal fracture fixation prevents bacterial translocation. Clin Orthop Relat Res. 2006;446:253-258.
27 Pape HC, Dwenger A, Regel G, et al. Pulmonary damage after intramedullary femoral nailing in traumatized sheep—is there an effect from different nailing methods? J Trauma. 1992;33:574-581.
28 Wolinsky PR, Banit D, Parker RE, et al. Reamed intramedullary femoral nailing after induction of an “ARDS-like” state in sheep: Effect on clinically applicable markers of pulmonary function. J Orthop Trauma. 1998;12:169-176.
29 Bochicchio GV, Napolitano LM, Joshi M, et al. Systemic inflammatory response syndrome score at admission independently predicts infection in blunt trauma patients. J Trauma. 2001;50:817-820.
30 Ertel W, Keel M, Bonaccio M, et al. Release of anti-inflammatory mediators after mechanical trauma correlates with severity of injury and clinical outcome. J Trauma. 1995;39:879-887.
31 Giannoudis PV, Abbott C, Stone M, et al. Fatal systemic inflammatory response syndrome following early bilateral femoral nailing. Intensive Care Med. 1998;24:641-642.
32 Harwood PJ, Giannoudis PV, van Griensven M, et al. Alterations in the systemic inflammatory response after early total care and damage control procedures for femoral shaft fracture in severely injured patients. J Trauma. 2005;58:446-454.
33 Malone DL, Kuhls D, Napolitano LM, et al. Back to basics: Validation of the admission systemic inflammatory response syndrome score in predicting outcome in trauma. J Trauma. 2001;51:458-463.
34 Napolitano LM, Ferrer T, McCarter RJJr, Scalea TM. Systemic inflammatory response syndrome score at admission independently predicts mortality and length of stay in trauma patients. J Trauma. 2000;49:647-653.
35 Pape HC, Grimme K, Van Griensven M, et al. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: Prospective randomized analysis by the EPOFF Study Group. J Trauma. 2003;55:7-13.
36 Wanner GA, Keel M, Steckholzer U, et al. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med. 2000;28:950-957.
37 Bone LB, Babikian G, Stegemann PM. Femoral canal reaming in the polytrauma patient with chest injury. A clinical perspective. Clin Orthop Relat Res.; 318; 1995; 91-94.
38 Brundage SI, McGhan R, Jurkovich GJ, et al. Timing of femur fracture fixation: Effect on outcome in patients with thoracic and head injuries. J Trauma. 2002;52:299-307.
39 Carlson DW, Rodman GHJr, Kaehr D, et al. Femur fractures in chest-injured patients: Is reaming contraindicated? J Orthop Trauma. 1998;12:164-168.
40 Charash WE, Fabian TC, Croce MA. Delayed surgical fixation of femur fractures is a risk factor for pulmonary failure independent of thoracic trauma. J Trauma. 1994;37:667-672.
41 Handolin L, Pajarinen J, Lassus J, Tulikoura I. Early intramedullary nailing of lower extremity fracture and respiratory function in polytraumatized patients with a chest injury: A retrospective study of 61 patients. Acta Orthop Scand. 2004;75:477-480.
42 Riska EB, von Bonsdorff H, Hakkinen S, et al. Primary operative fixation of long bone fractures in patients with multiple injuries. J Trauma. 1977;17:111-121.
43 Weninger P, Figl M, Spitaler R, et al. Early unreamed intramedullary nailing of femoral fractures is safe in patients with severe thoracic trauma. J Trauma. 2007;62:692-696.
44 Nau T, Aldrian S, Koenig F, Vecsei V. Fixation of femoral fractures in multiple-injury patients with combined chest and head injuries. ANZ J Surg. 2003;73:1018-1021.
45 The Canadian Orthopaedic Trauma Society. Reamed versus unreamed intramedullary nailing of the femur: Comparison of the rate of ARDS in multiple injured patients. J Orthop Trauma. 2006;20:384-387.
46 Jaicks RR, Cohn SM, Moller BA. Early fracture fixation may be deleterious after head injury. J Trauma. 1997;42:1-6.
47 Townsend RN, Lheureau T, Protech J, et al. Timing fracture repair in patients with severe brain injury (Glasgow Coma Scale score <9). J Trauma. 1998;44:977-983.
48 Hofman PA, Goris RJ. Timing of osteosynthesis of major fractures in patients with severe brain injury. J Trauma. 1991;31:261-263.
49 Kotwica Z, Balcewicz L, Jagodzinski Z. Head injuries coexistent with pelvic or lower extremity fractures—early or delayed osteosynthesis. Acta Neurochir (Wien). 1990;102(1-2):19-21.
50 McKee MD, Schemitsch EH, Vincent LO, et al. The effect of a femoral fracture on concomitant closed head injury in patients with multiple injuries. J Trauma. 1997;42:1041-1045.
51 Nau T, Kutscha-Lissberg F, Muellner T, et al. Effects of a femoral shaft fracture on multiply injured patients with a head injury. World J Surg. 2003;27:365-369.
52 Poole GV, Miller JD, Agnew SG, Griswold JA. Lower extremity fracture fixation in head-injured patients. J Trauma. 1992;32:654-659.
53 Starr AJ, Hunt JL, Chason DP, et al. Treatment of femur fracture with associated head injury. J Orthop Trauma. 1998;12:38-45.
54 Velmahos GC, Arroyo H, Ramicone E, et al. Timing of fracture fixation in blunt trauma patients with severe head injuries. Am J Surg. 1998;176:324-330.
55 Riemer BL, Butterfield SL, Diamond DL, et al. Acute mortality associated with injuries to the pelvic ring: The role of early patient mobilization and external fixation. J Trauma. 1993;35:671-677.