Serous Cystadenoma
Synonyms/Description
An epithelial-stromal cystic tumor containing serous fluid
Etiology
Serous cystadenomas are the most common type of epithelial-stromal tumors. They are lined with cells similar to those lining the fallopian tubes, suggesting that the origin may be tubal rather than ovarian. These cysts can become very large, although not typically as large as mucinous cystadenomas, and up to 20% are bilateral. Most (70%) are benign, whereas 5% to 10% have borderline malignant potential, and 20% to 25% are frankly malignant, although there is no indication that benign serous tumors transform into malignant ones.
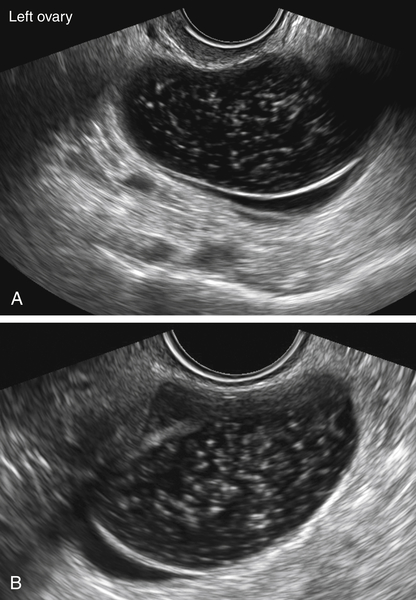
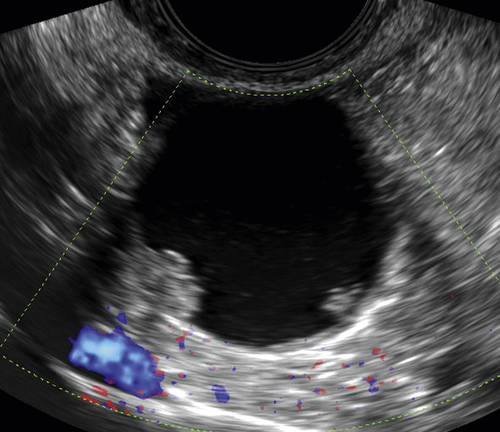
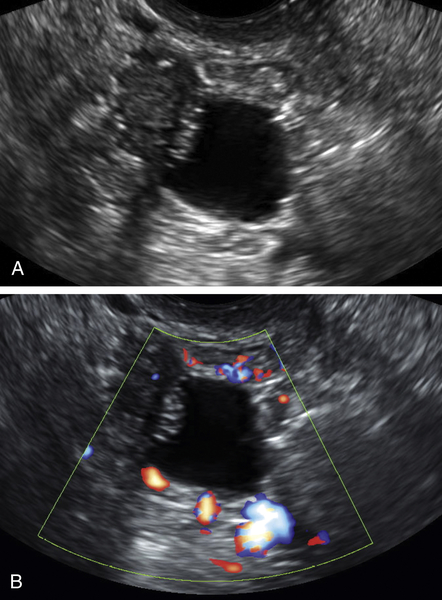
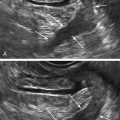
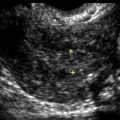
Ultrasound Findings
Serous cystadenomas are typically thin-walled unilocular cysts, although they can also be multilocular. They are filled with serous fluid, which is usually clear or may contain tiny particles. Although less common, a borderline or malignant tumor must be considered (see elsewhere in the book for more information on borderline and malignant ovarian tumors) in cysts with solid components or nodules, especially if blood flow is detected with color Doppler.
Differential Diagnosis
The differential diagnosis includes any adnexal cystic mass such as a mucinous cystadenoma, cystadenofibroma, endometrioma, peritoneal inclusion cyst, degenerating fibroid, or hydrosalpinx. When unilocular, or simple, they are virtually indistinguishable from functional type follicular cysts. The presence of a separate ovary may be helpful to focus on non-ovarian etiologies such as a hydrosalpinx, degenerating fibroid, or even paraovarian cysts. A mucinous cystadenoma is more likely to be multicystic, displaying varying sonographic textures within the different compartments compared with a serous cystadenoma. An endometrioma typically has characteristic homogeneous low-level echoes. Serous cystadenomas and some cystadenofibromas can be virtually indistinguishable.
Clinical Aspects and Recommendations
Cysts that are symptomatic, growing over several cycles, or extremely large are typically managed surgically. The type of surgery and route will depend on multiple factors, such as the patient’s age, reproductive stage, size of the mass, and benign versus nonbenign appearance of the mass.
Figures