88
Cutaneous small vessel vasculitis (hypersensitivity vasculitis)
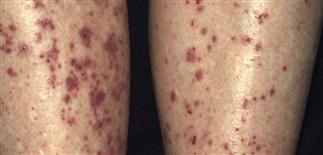
The pretibial surfaces are often affected in hypersensitivity vasculitis.
Lesions occur in crops. Early lesions may be nonpalpable, late lesions are palpable and may ulcerate.

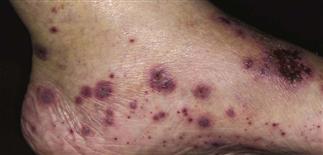
Lower extremities become edematous and papules coalesce in patients with severe hypersensitivity vasculitis.

The dorsal aspect of the toe is a common location to find hypersensitivity vasculitis.
DESCRIPTION
Group of disorders characterized by inflammation of small blood vessels in the skin, primarily postcapillary venules. The principle skin lesion is palpable purpura.
HISTORY
• Precipitated by many infectious agents, drugs, chemicals, and food allergens; associated with many chronic connective tissue diseases and malignancies. • In 60% of patients, no precipitating agent or coexistent disease is identified. • Caused by deposition of IgG or IgM immune complexes in small postcapillary venules, resulting in leukocytoclastic vasculitis. • Commonly associated with arthralgias, myalgias, fever, and malaise. Multiple organs can be involved. • Most patients improve in 1 month, but condition may be chronic in some.
PHYSICAL FINDINGS
• Early lesions are asymptomatic purpuric macules. Older lesions coalesce and become edematous and palpable, ranging in size from pinpoint to several centimeters. • Purpuric papules, nodules, pustules, vesicles, bullae, and ulcerations can occur. • Lesions are more prominent on any dependent area or an area under local pressure (e.g. the back and arms of supine patients). They are uncommon on face, palms, and soles. • Lesions can be itchy and painful, and occur in crops. • Patients frequently develop ankle and lower leg edema.
TREATMENT
• Removal of precipitating agents and appropriate treatment of coexistent disease usually results in resolution. • Local measures using topical steroids and antibiotics help some patients. • Antihistamines and non-steroidal anti-inflammatory drugs control fever, myalgias, and arthralgias. • Systemic corticosteroids (prednisone 60–80 mg q.d.) are helpful for managing systemic manifestations and skin ulceration. Rebound can be prevented with a slow taper over 3–6 weeks. • Immunosuppressive agents (cyclophosphamide, methotrexate, azathioprine, ciclosporin) have been used when systemic corticosteroids fail.







