Chapter 48 Cutaneous metastases
1. How often do internal malignancies metastasize to the skin?
Cutaneous metastases of internal malignancies are relatively uncommon. An autopsy study including 7500 patients with internal malignancies demonstrated cutaneous metastases in 9% of patients. Most cases occur late in the course of the disease, but cutaneous metastasis may also be the initial presentation of an internal malignancy.
2. By what three routes do internal malignancies metastasize to the skin?
They extend by local infiltration, lymphatic spread, or hematogenous spread. Breast carcinoma and oral cancer are the most likely to demonstrate direct extension into the skin. It is assumed that the fundamental mechanisms are similar to those of metastasis to parenchymal organs, but this has not been investigated. Rare cases have been inoculated by local procedures such as needle biopsies.
3. How do malignant cells invade and metastasize?
The genetic and molecular events that allow cells to invade and metastasize are a complex issue that is being studied in numerous laboratories. Malignant cells must be able to detach from adjacent cells (i.e., downregulate adhesion molecules), adhere to the adjacent matrix by the development of receptors to matrix molecules, such as fibronectin; lyse the extracellular matrix by the production of various enzymes; and migrate by the production of motility factors, such as hepatocyte growth factor. Once the tumor cells gain access to lymphatic spaces or blood vessels, they must be able to express adhesion molecules on their surface, which then allows them to attach to endothelial cells (e.g., CD44). There is also evidence that certain normal tissues produce chemoattractants that may attract tumor to a specific site.
Nguyen TH: Mechanisms of metastasis, Clin Dermatol 22:209–216, 2004.
4. What are the most common cancers that metastasize to the skin in women?
Different gender and age groups are affected by somewhat different metastatic malignancies. In a large study done at the Armed Forces Institute of Pathology in the early 1970s, the most common etiologies of cutaneous metastases in women were:
5. What are the most common cancers that metastasize to the skin in men?
6. Do metastases to the skin typically occur in random patterns?
No. Different tumors demonstrate characteristic patterns of metastases (Table 48-1). A well-known example is ocular malignant melanoma, which frequently demonstrates metastasis to the liver. As a rule, cutaneous metastases usually appear in skin that is near the primary tumor (Fig. 48-2). Most regional metastases are probably spread through the lymphatic system, while distant metastases are more likely to occur via the hematogenous route.
7. Describe the most common presentations of malignancies metastatic to the skin.
Cutaneous metastases most commonly present as a cutaneous nodule or group of nodules that may be movable or fixed to underlying structures. Less commonly, they may present as indurated plaques. They may be skin-colored (Fig. 48-3), violaceous, erythematous, or, rarely, pigmented (malignant melanoma). The overlying epidermis is usually intact, but large metastatic lesions may be eroded or ulcerated. Clinically, they may mimic primary cutaneous lesions, including epidermoid cysts, lipomas, primary cutaneous malignancies, neurofibromas, scars, pyogenic granulomas, cellulitis, and even dermatitis. Metastatic breast carcinoma may uncommonly present with distinct patterns, including carcinoma erysipelatoides (inflammatory carcinoma; Fig. 48-4), carcinoma telangiectaticum (a variant of inflammatory carcinoma), and carcinoma en cuirasse (a sclerodermoid pattern).
8. What is alopecia neoplastica?
The scalp appears to be a unique site for cutaneous metastasis, and often cutaneous metastases to the scalp are a presenting sign for internal malignancy. One characteristic clinical presentation is that of an isolated, indurated plaque in the scalp with associated alopecia (Fig. 48-5). Biopsy of this site will demonstrate cutaneous metastasis of a visceral malignancy and loss of hair follicles. The most common tumors to metastasize to the scalp are those of the breast, lung, and kidney.
9. What is a Sister Mary Joseph’s nodule?
It is a nodular umbilical metastatic tumor (Fig. 48-6). This sign is named in recognition of Sister Mary Joseph, who was the superintendent of St. Mary’s Hospital in Rochester, Minnesota, and served as the first surgical assistant to Dr. W.J. Mayo. She is credited with recognizing that patients with this finding had a poor prognosis.
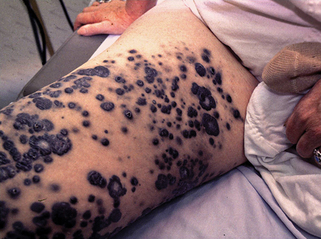
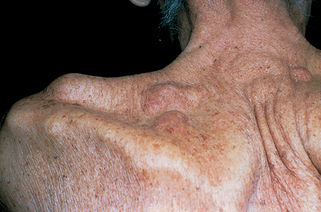
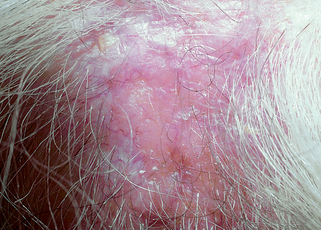
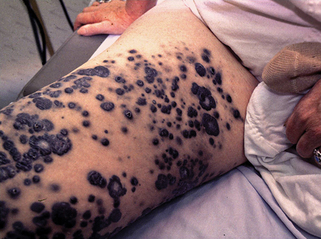
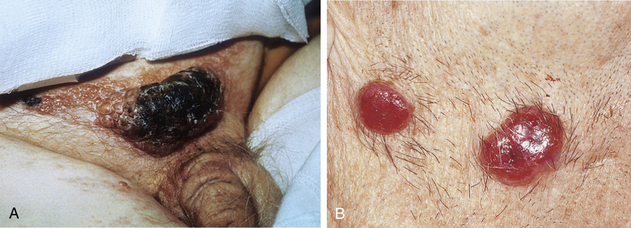
Figure 48-1. Heavily pigmented metastatic melanoma due to in transit metastases from a primary tumor on the lower extremity.
(Courtesy of Rene Gonzalez, MD.)
Table 48-1. Characteristic Sites of Cutaneous Metastases
| PRIMARY TUMOR | SITE OF METASTASES |
|---|---|
| Oral squamous cell carcinoma | Head and neck |
| Thyroid carcinoma | Neck |
| Lung | Chest wall |
| Breast | Anterior chest wall |
| Renal cell carcinoma | Head |
| Gastrointestinal carcinoma | Abdomen |
| Genitourinary carcinoma | Lower abdomen |
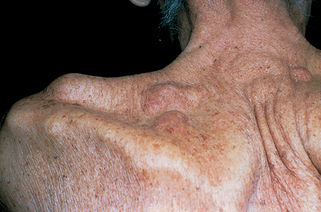
Figure 48-3. Metastatic adenocarcinoma of the gastrointestinal tract presenting as skin-colored dermal and subcutaneous nodules.
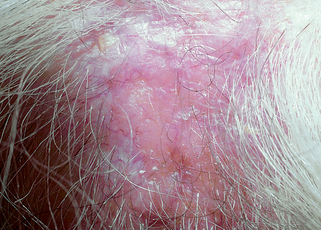
Figure 48-5. Alopecia neoplastica secondary to metastatic breast carcinoma. On palpation, the lesion was firm and indurated.
11. Does basal cell carcinoma ever metastasize?
Yes. Basal cell carcinoma is the most common cutaneous malignancy in the United States with over 1 million new cases per year. It has been estimated that the overall metastatic rate is 0.03% with the majority of cases occurring in large destructive tumors that have been present for many years. Basal cell carcinomas most commonly metastasize to regional lymph nodes followed by the lungs, bones, and skin. The 5-year survival for metastatic basal cell carcinoma is grave and is estimated to be about 10%.
12. How do you diagnose a cutaneous metastasis?
The diagnosis is best established by doing an excisional, incisional, or punch biopsy, and by submitting the specimen in formalin for routine processing. In addition to hematoxylin and eosin (H&E) stains, the pathologist can perform special histochemical stains (e.g., mucicarmine for mucin, Fontana-Masson for melanin) or immunoperoxidase studies (e.g., prostate-specific antigen for prostate cancer and calcitonin for medullary thyroid carcinoma). Problematic cases may require submission of part of the tumor for electron microscopy, or frozen for immunoperoxidase studies that cannot be done on formalin-fixed tissue. Less commonly, the tumor specimen is obtained by a fine-needle aspiration.
13. What is the prognosis of a patient with a cutaneous metastasis?
Cutaneous metastasis is usually a poor prognostic sign and often reflects preexisting widespread internal metastasis. In one study, the average life expectancy after development of skin metastases was only 3 months. The prognosis is ultimately dependent on the primary tumor, and some patients do survive for years.