Chapter 38 Cutaneous manifestations of renal disease
Fuchs E, Lynfield Y: Dialysis acne, J Am Acad Dermatol 23:125, 1990.
Walsh SR, Parada NA: Images in clinical medicine. Uremic frost, N Engl J Med 352:e13, 2005.
Urbonas A, Schwartz RA, Szepietowski JC: Uremic pruritus: an update, Am J Nephrol 21:343–350, 2001.
Patterson JW: The perforating disorders, J Am Acad Dermatol 10:561–581, 1984.
Green JJ, Manders SM: Pseudoporphyria, J Am Acad Dermatol 44:100–108, 2001.
Key Points: Cutaneous Manifestations of Renal Disease
Desnick RJ, Brady RO: Fabry disease in childhood, J Pediatrics 144:S20–S26, 2004.
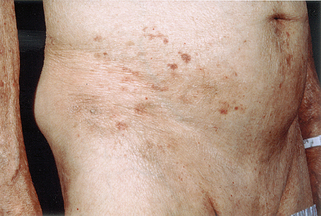
When skin lesions suggestive of vasculitis occur, a skin biopsy should be done to confirm the diagnosis and determine the type of vessel and inflammation involved (see also Chapter 15). Vessel involvement may vary from small postcapillary venules (leukocytoclastic vasculitis) to medium-sized arteries (polyarteritis nodosa). If vasculitis is confirmed, testing should be done to determine if the kidneys are also involved.
Wong CK, Wang WJ: Systemic amyloidosis. A report of 19 cases, Dermatology 189:47–51, 1994.