Chapter 35 Cutaneous manifestations of internal malignancy

Figure 35-1. Sweet’s syndrome demonstrating painful red indurated plaques on on the hand and arm.
(Courtesy of James E. Fitzpatrick, MD.)
Bae-Harboe Y-SC, Salter SA, Kimball A: Acute febrile neutrophilic dermatosis, eMedicine Online August 2009. Available at: http://www.emedicine.com.

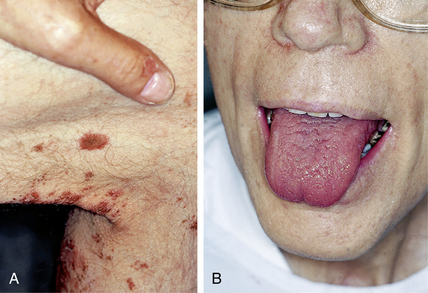
Figure 35-2. Acanthosis nigricans with hyperpigmented velvety skin lesions and small tags on the proximal thigh and groin.
Miller J, Rapini R: Acanthosis nigricans, eMedicine Online, June 2002. Available at: http://www.emedicine.com/derm/topic1.htm.
Zettouni N, Harvey N: Glucagonoma syndrome, eMedicine Online, http://www.emedicine.com. May 2008.
In addition to the facial rash, lesions on the scalp, neck, upper trunk, and extensor extremities are common. As the lesions mature, scaling and atrophy may develop. The erythema on the hands occurs over the knuckles rather than over the phalanges, as is typical of lupus erythematosus. Cuticular telangiectasias can be seen in both lupus erythematosus and dermatomyositis. Frequently, flat-topped, red-to-violaceous papules known as Gottron’s papules develop over the knuckles of patients with dermatomyositis (Fig. 35-4B).
Callen JP, Wortman RL: Dermatomyositis, Clin Dermatol 24:363–373, 2006.

Figure 35-5. Paraneoplastic pemphigus demonstrating extensive superficial blisters and erosions.
(Courtesy of James E. Fitzpatrick, MD.)
Zhu X, Zhang B: Paraneoplastic pemphigus, J Dermatol 34:503–511, 2007.
DelRosario R, Allen K, Kaneshiro S: Erythema gyratum repens, eMedicine Online, http://www.emedicine.com. May 2009.
Buxtorf K, Hubscher E, Panizzon R: Bazex syndrome, Dermatology 202:350–352, 2001.
Kao GF: Paget disease, mammary, eMedicine Online November 2007.
Wilde JL: Extramammary Paget’s disease, eMedicine Online, http://www.emedicine.com. November 2007.
Nyirady J, Schwartz RA: Primary systemic amyloidosis, eMedicine Online, http://www.emedicine.com. April 2009.
Schwartz R: The sign of Leser-Trélat, eMedicine Online May 2009.
Callen J, Jackson JM: Pyoderma gangrenosum: an update, Rheumatol Dis Clin N Am 33:787–802, 2007.
Nardino RT, Silber AL: Erythromelalgia, eMedicine Online, http://www.emedicine.com. August 2009.
Lober CW: Pruritis and malignancy, Clin Dermatol 11:125–128, 1993.
Key Points: Cutaneous Manifestations of Internal Malignancy
Rapini RP: Multicentric reticulohistiocytosis, eMedicine Online, http://www.emedicine.com. March 2008.
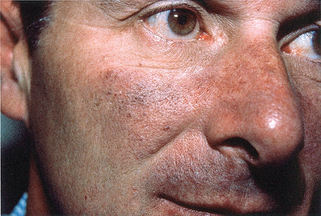
Figure 35-9. Carcinoid syndrome. Patient with long history of flushing and development of persistent telangiectasias of the face.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
Santacroce L, Diomede D, Balducci L: Malignant carcinoid syndrome, eMedicine Online, http://www.emedicine.com. November 2009.
Lynch HT, Fusaro R, Lynch JF, et al: Pancreatic cancer and the FAMM syndrome, Fam Cancer 7:103–112, 2008.