CHAPTER 31 Cryptorchidism
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
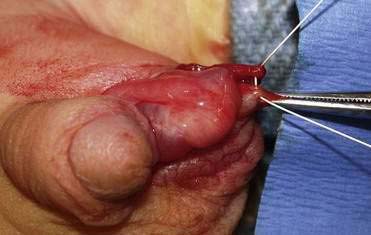
Step 3: Operative Steps
Anesthetic Induction
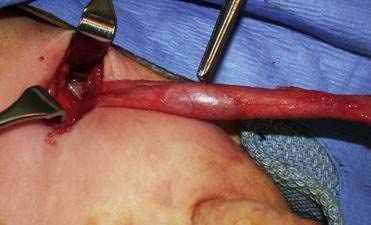
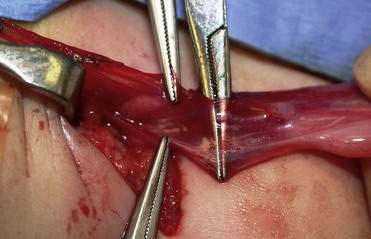
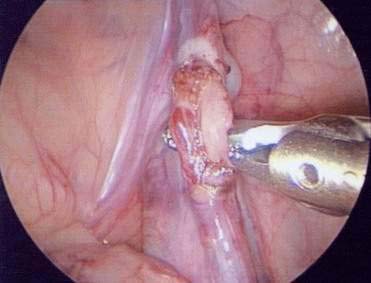
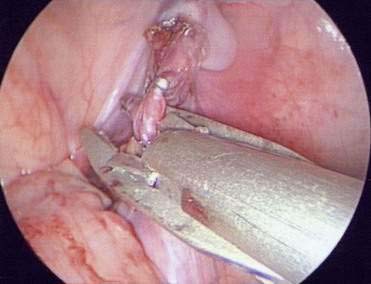
Incision and Technique
Step 5: Pearls and Pitfalls
Cristensen JD, Dogra VS. The undescended testis. Semin Ultrasound CT MRI. 2007;28:307-316.
Hutson JM, Clarke MCC. Current management of the undescended testicle. Semin Pediatr Surg. 2007;16:64-70.
Hutson JM, Hasthorpe S. Testicular descent and cryptorchidism: the state of the art in 2004. J Pediatr Surg. 2005;40:297-302.
Lee PA. Fertility in cryptorchidism: does treatment make a difference? Endocrinol Metab Clin North Am. 1993;22:479-490.
Lee PA, Coughlin MT. The single testis: paternity after presentation as unilateral cryptorchidism. J Urol. 2002;168:1680-1683.
Mesrobian H-GO, Chassaignac JM, Laud PW. The presence or absence of an impalpable testis can be predicted from clinical observations alone. BJU Int. 2002;90:97-99.
Murphy F, Paran TS, Puri P. Orchidopexy and its impact on fertility. Pediatr Surg Int. 2007;23:625-632.
Oh J, Landman J, Evers A, et al. Management of the postpubertal patient with cryptorchidism: an updated analysis. J Urol. 2002;167:1329-1333.
Rabinowitz R, Hulbert WC. Late presentation of cryptorchidism: the etiology of testicular re-ascent. J Urol. 1997;157:1892-1894.
Rasmussen TB, Ingerslev HJ, Hostrup H. Bilateral spontaneous descent of the testis after the age of 10: subsequent effects on fertility. Br J Surg. 1988;75:820-823.
Ritzen EM, Bergh A, Bjerknes R, et al. Nordic consensus on treatment of undescended testis. Acta Paediatr. 2007;96:638-643.
Taran I, Elder JS. Results of orchiopexy for the undescended testis. World J Urol. 2006;24:231-239.
Thorup J, Haugen S, Kollin C, et al. Surgical treatment of undescended testes. Acta Paediatr. 2007;96:631-637.
Tomiyama H, Sasaki Y, Huynh J, et al. Testicular descent, cryptorchidism and inguinal hernia: the Melbourne perspective. J Pediatr Urol. 2004;1:11-25.
Virtanen HE, Bjerknes R, Cortes D, et al. Cryptorchidism: classification, prevalence and long-term consequence. Acta Paediatr. 2007;96:611-616.
Virtanen HE, Cortes D, Rajpert-De Meyts E, et al. Development and descent of the testis in relation to cryptorchidism. Acta Paediatr. 2007;96:622-627.
Walsh TJ, DallEra MA, Croughan MS, et al. Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol. 2007;78:1440-1446.