Cranial Nerves
The Eye 2 – Fundi
BACKGROUND
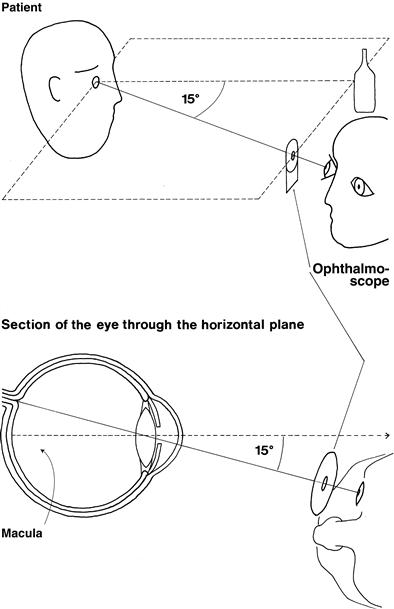
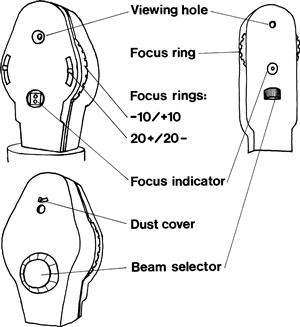
The ophthalmoscope provides a light source and an optical system to allow examination of the fundus (Fig. 8.1).
Its moving parts are:
The focus ring is used to correct (1) for your vision and (2) for the patient’s vision.
Beam selector choices are:
WHAT TO DO
• Turn off the lights or draw the curtains.
• Check the focus is set at zero, and that the light works and is on the correct beam.
To examine the right eye (Fig. 8.2):
• Take the ophthalmoscope in your right hand.
• Approach the patient’s right side.
• The pupil should appear pink, as in bad flash photographs. This is the red reflex.
• Gradually move in towards the eye.
• Encourage the patient to keep looking at the distant point and not at the light.
• Bring the ophthalmoscope to within 1–2 cm of the eye.
• Keep the ophthalmoscope at the same level as the patient’s eye and the fixation point.
If the eye is approached as described, the optic disc should be in view. If it is not, focus on a blood vessel and follow it. The acute angles of the branches and convergence of artery and vein indicate the direction to follow. Alternatively, start again.
To examine the left eye:
1 Look at the optic disc
2 Look at the blood vessels
Arteries (light-coloured) should be two-thirds the diameter of veins (burgundy-coloured).
3 Look at the retinal background
WHAT YOU FIND
1 Optic disc
See Figures 8.3 and 8.4.
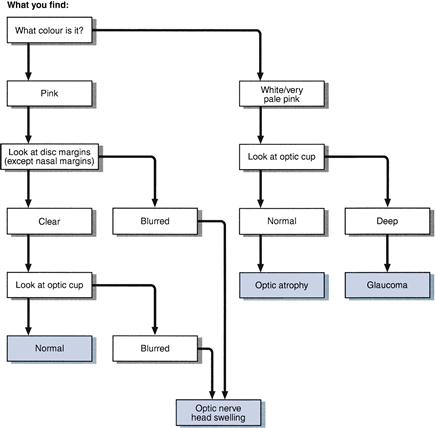
Figure 8.3 Flow chart: optic disc abnormalities
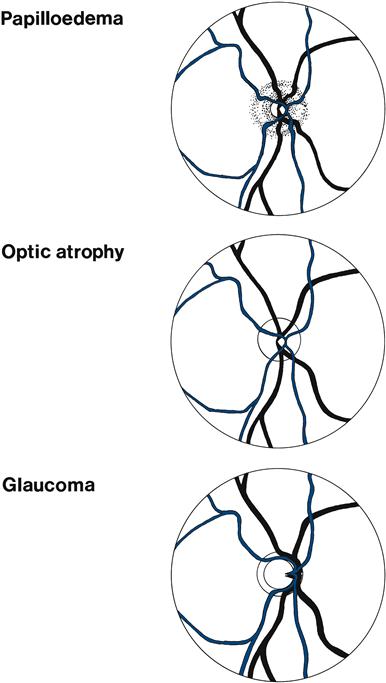
Figure 8.4 Optic disc abnormalities
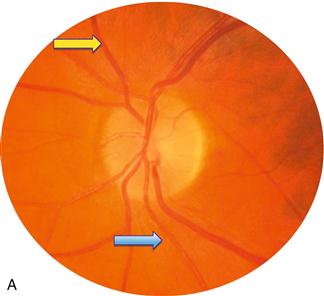
The optic cup is slightly on the nasal side of the centre of the optic disc. Its diameter is normally less than 50% of the disc (Figs 8.5A and 8.6).
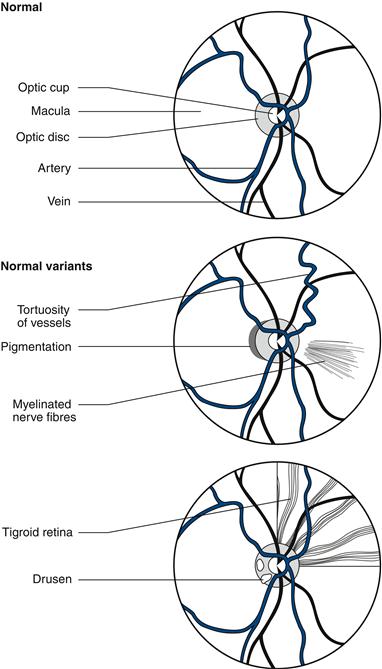
Figure 8.6 Normal variants
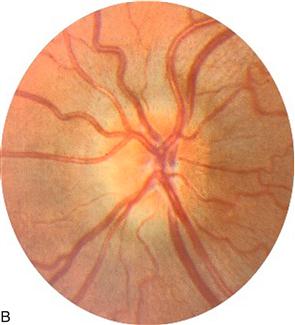
The optic nerve head is swollen (Fig. 8.5B). This can be caused by papilloedema or papillitis. Papilloedema usually produces more swelling, with humping of the disc margins—not usually associated with visual disturbance (may enlarge blind spot). Papillitis is associated with visual loss, especially central scotomas.
A swollen optic disc is often difficult to find, the vessels disappearing without an obvious optic disc.
The difference between papilloedema and papillitis can be remembered as follows:
• You see nothing (cannot find the disc) + patient sees everything (normal vision) = papilloedema.
• You see nothing + patient sees nothing (severe visual loss) = papillitis.
• You see everything (normal-looking disc) + patient sees nothing = retrobulbar neuritis.
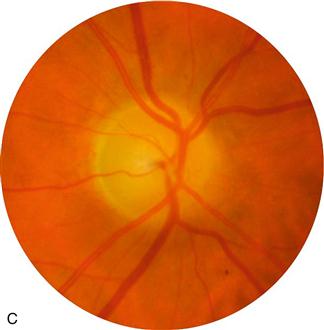
The optic nerve head is very pale—optic atrophy (Fig. 8.5C). The optic cup is markedly enlarged, taking up most of the disc – glaucoma (Fig. 8.5D).
2 Blood vessels
3 Retinal background (Fig. 8.7)
General background
• Pigmented background: normal, especially in dark-skinned people. If striped, this is called tigroid.
• Pale:
– Clear: normal in fair-skinned people, also seen in albinos.
– Cloudy: macula appears as ‘cherry-red’ spot, vessels narrow—seen in retinal artery occlusion.
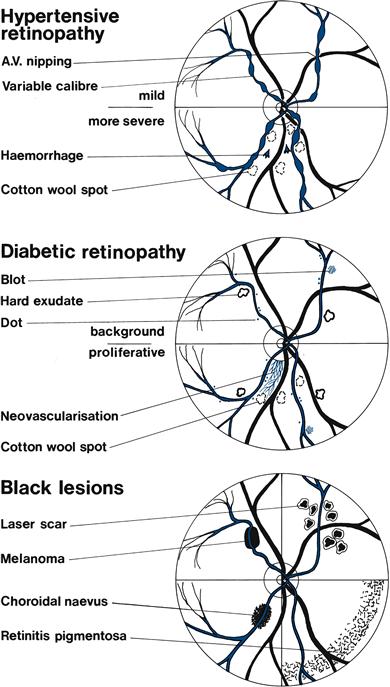
Figure 8.7 Retinal abnormalities
White/yellow lesions
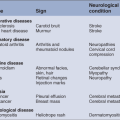
WHAT IT MEANS
1 Optic disc
2 Blood vessels and retinal background
• Hypertensive retinopathy (Figs 8.7 and 8.8A&B):
– Stage I: arteriolar narrowing and vessel irregularity.
– Stage II: arteriovenous nipping.
– Stage III: flame-shaped haemorrhages, hard exudates and cotton wool spots.
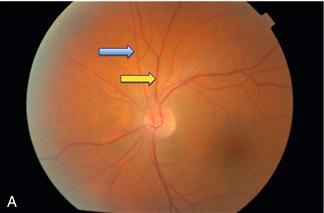
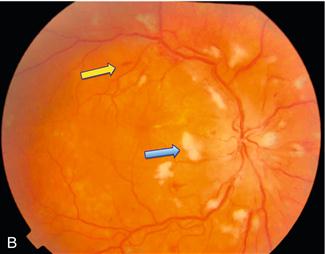
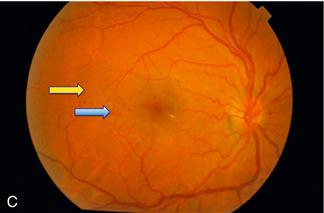
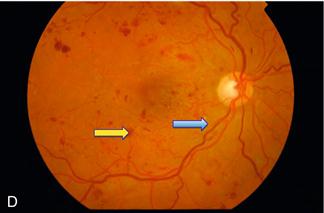
Figure 8.8 A. Normal retina: blue arrow = artery; yellow arrow = vein
B. Severe hypertensive retinopathy: blue arrow = cotton wool spot; yellow arrow = flame haemorrhage
C. Background diabetic retinopathy: blue arrow = blot haemorrhage; yellow arrow = dot haemorrhage
D. Severe diabetic retinopathy: blue arrow = hard exudate; yellow arrow = blot haemorrhage
• Diabetic retinopathy (Figs 8.7 and 8.8C&D):
– Background: microaneurysms, dot and blot haemorrhages, hard exudates.

 TIP
TIP TIP
TIP