Cranial Nerves III, IV, VI
Eye Movements
BACKGROUND
Eye movements can be divided into four types:
The sites of control of these eye movements differ (Fig. 9.1).
| Type of eye movement | Site of control |
| Saccadic (command) | Frontal lobe |
| Pursuit | Occipital lobe |
| Vestibular–positional | Cerebellar vestibular nuclei |
| Convergence | Midbrain |
In the brainstem, the inputs from the frontal and occipital lobes, the cerebellum and the vestibular nuclei are integrated so that both eyes move together. Important structures are the centre for lateral gaze in the pons and the medial longitudinal fasciculus (MLF), which runs between the nuclei of the III and IV cranial nerves (in the midbrain) and the VI (in the pons).
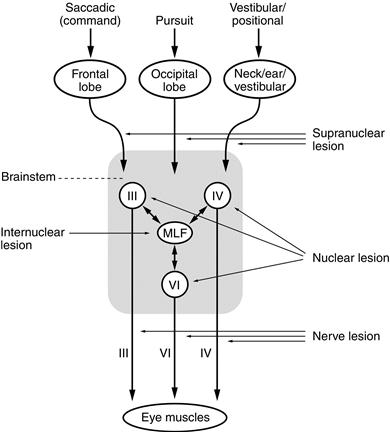
Figure 9.1 Control of eye movements
The III, IV and VI cranial nerves then control the following muscles (Fig. 9.2):
Abnormalities can arise at any level (Fig. 9.1):
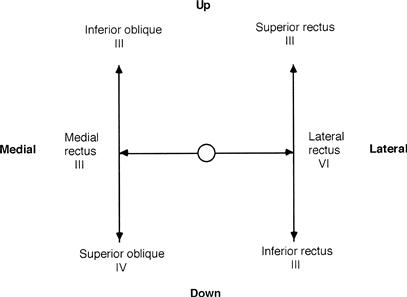
Figure 9.2 Muscles involved in eye movement
No double vision (generally):
Double vision:
Internuclear and supranuclear lesions rarely cause double vision.
WHAT TO DO
Look at the position of the head.
Look at the eyes.
• Note ptosis (see Chapter 6).
• Note the resting position of the eyes and the position of primary gaze.
Look at the position of the eyes in primary gaze.
Perform the cover test (Fig. 9.3).
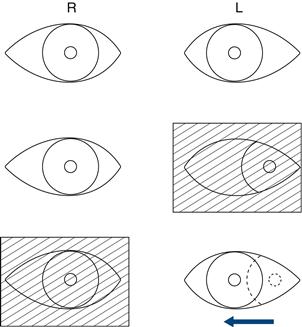
Figure 9.3 The cover test. For an explanation, see text
The cover test
What to do
This is a test for latent squint.
Ask the patient to look with both eyes at your right eye, then cover his left eye. Then uncover the left eye rapidly and cover the right eye. Look to see if the left eye has to correct to look back at your eye. Repeat, covering the left eye and watching the right eye.
What you find
If one eye has to correct as it is uncovered, this indicates that the patient has a latent strabismus (squint), which can be classified as divergent or convergent.
Test the eye movements to pursuit
• Move the pen slowly. Ask the patient to tell you if he sees double:
– up and down at the extreme of lateral gaze.
• Ensure the patient’s nose does not prevent the pen being seen at the extreme of lateral gaze.
As you do this, watch the movements of the eyes.
If the patient reports seeing double at any stage:
• Establish if the images are side by side, up and down, or at an angle.
• Establish the direction in which the images are widest apart.
• In this position, briefly cover one eye and ask which image disappears: the inner or outer. Repeat this by covering the other eye (Fig. 9.4).
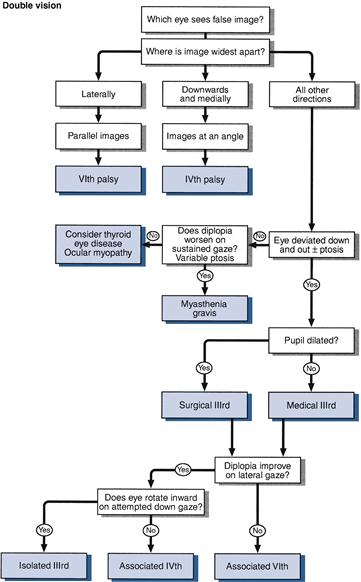
Figure 9.4 Flow chart: double vision
Test saccadic eye movements
Test convergence
Ask the patient to look into the distance and then look at your finger placed 50 cm in front of him. Gradually bring the eyes in, observing the limit of convergence of the eyes.
Vestibulo-ocular reflex (doll’s eye manœuvre)
This test is most commonly used in unconscious patients, when it provides a way of testing eye movements. In conscious patients with limited eye movements on command or pursuit, the test can be used to demonstrate preserved eye movements on vestibulo-positional stimulation, indicating a supranuclear eye movement abnormality.
Ask the patient to look into the distance at a fixed point; turn his head to the left then the right, and flex the neck and extend the neck.
The eyes should move within the orbits, maintaining forward gaze.
WHAT YOU FIND
• The eyes are misaligned in primary gaze:
– One eye is deviated downwards and out, with ptosis = third nerve lesion.
– Eyes aligned in different vertical planes = skew deviation.
• The patient has double vision (Fig. 9.4):
Try to answer the following questions:
Is there a single nerve (VI, III or IV) deficit (Fig. 9.5)?
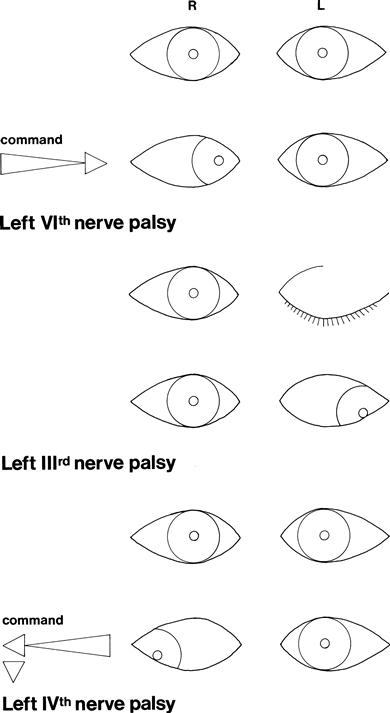
Figure 9.5 Single nerve palsies
– Is there a combination of single nerves?
Other common abnormalities:
• Patient does not look towards one side = lateral gaze palsy; check response to vestibulo-ocular reflex testing (Fig. 9.6).
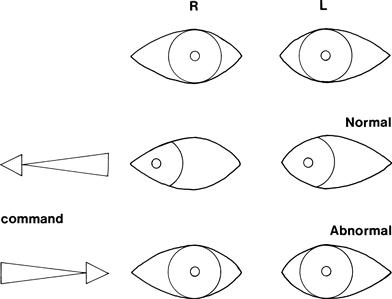
Figure 9.6 Left lateral gaze palsy
• Patient does not look up = upgaze palsy.
• Patient does not look down = downgaze palsy.
• Eyes do not move together, with markedly slowed adduction and with nystagmus in the abducting eye = internuclear ophthalmoplegia with ataxic nystagmus (Fig. 9.7).
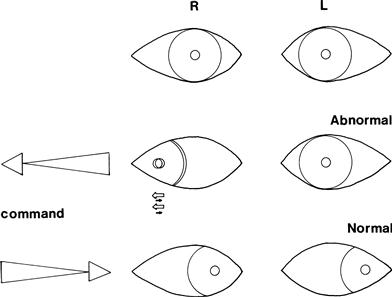
Figure 9.7 Left internuclear ophthalmoplegia. There is nystagmus of the right eye as the eye looks to the right
• Eye movement falls short of target and requires a second movement to fixate = hypometric saccades.
WHAT IT MEANS
• Lateral gaze palsy: can arise from:
• Vertical gaze palsy: lesions in the upper brainstem.
• Supranuclear palsy with preserved positional/vestibular testing: may arise in association with akinetic rigid syndromes (Chapter 24), when it is referred to as the Steele–Richardson syndrome or progressive supranuclear palsy, and may be seen in other degenerative conditions.
• Hypometric saccades: indicate a cerebellar lesion—see Chapter 23.

 TIP
TIP