Problem 33 Cough, dyspnoea and fever in a 55-year-old man
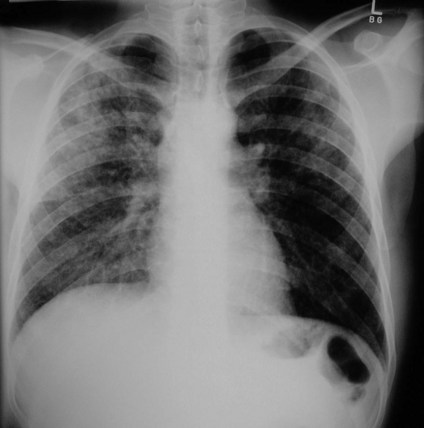
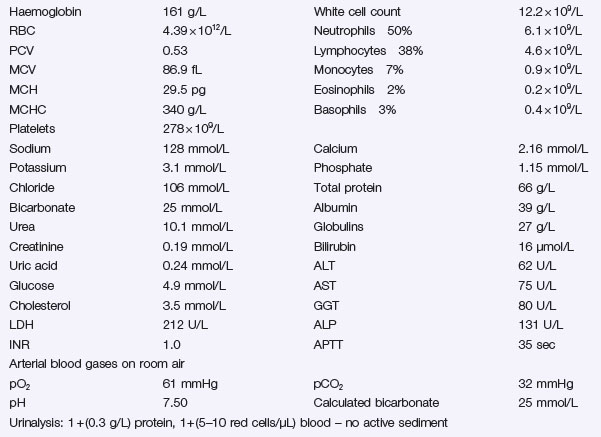
You review the chest X-ray Figure 33.1 and the results of your other tests can be seen in Investigation 33.1.
Answers
However, some patients can present with fever without localizing symptoms.
A.4 Community-acquired pneumonia in the immunocompetent host can be caused by a broad range of pathogens which differ from those seen in hospital-acquired pneumonias and pneumonias in immunocompromised hosts (Table 33.1).
| Causative Oragnism | Percentages |
|---|---|
| Streptococcus pneumoniae | 42 |
| Mycoplasma pneumoniae | 9 |
| Legionella species | 3 |
| Chlamydia species | 2 |
| Gram-negative | 3 |
| Haemophilus influenzae | 5 |
| Staph. aureus | 1 |
| Respiratory viruses | 14 |
| Other or unknown | 21 |
A.5 You should always assess the severity of pneumonia in every patient. It predicts the risk and prognosis, and determines admission and the types of recommended empiric antibiotics (see Table 33.2). The 30-day mortality for low-risk or mild pneumonia is less than 1%, while the 30-day mortality for severe (high-risk) pneumonia is approximately 27%.
Table 33.2 Treatment of community-acquired pneumonia
| Mild (Low-Risk) Pneumonia | Moderate Severity Pneumonia | Severe (High-Risk) Pneumonia |
|---|---|---|
| Outpatient treatment | Hospital admission | Hospital admission – consider intensive care assessment/admission |
| Oral amoxicillin plus doxycycline or Oral macrolide (clarithromycin or roxithromycin, azithromycin) |
IV benzyl penicillin and gentamicin plus oral doxycycline or macrolide or IV ceftriaxone plus IV erythomycin/azithromycin |
IV ceftriaxone or Tazocin plus IV azithromycin |
The severity of pneumonia can be graded and scored and is based on the following factors:
A.6 The initial antibiotic selection should be empirical as clinical and chest X-ray findings are not sufficiently specific for causal organism. The antibiotic choice should cover both pneumococcus and other less common organisms such as Legionella, Mycoplasma and Chlamydia pneumonias (see Table 33.2).
Revision Points
Community-Acquired Pneumonia
Aims of Management at Presentation
Issues to Consider
, www.brit-thoracic.org.uk. The website of the British Thoracic Society, with access to the excellent guidelines for the management of community-acquired pneumonia
, www.legionella.org. Public access website from the USA with plenty of information on this organism and the public health issues related to it