Chapter 34 Correction of Hyperextension Gait Abnormalities
Preoperative and Postoperative Techniques
INTRODUCTION AND DIAGNOSIS
It is well appreciated that patients with chronic insufficiency of the lateral and posterolateral structures of the knee may develop a gait abnormality characterized by excessive knee hyperextension during the stance phase (initial contact or heel-strike, loading response, midstance, and toe-off) of the gait cycle (Fig. 34-1). The primary lateral and posterolateral structures of the knee joint are the fibular collateral ligament (FCL) and popliteus muscle-tendon-ligament unit (PMTL), including the popliteofibular ligament (PFL) and the posterolateral capsule (PLC). These structures function together to resist lateral tibiofemoral compartment opening, posterior subluxation of the lateral tibial plateau with tibial rotation, knee hyperextension, and varus recurvatum (see Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures).8,9,12,13,19,26 Posterolateral injuries are frequently accompanied by a rupture to the anterior cruciate ligament (ACL) and, in some cases, a rupture to the posterior cruciate ligament (PCL).5,7,11 In addition, many knees with insufficiency to the posterolateral structures also have varus osseous malalignment. The comprehensive physical examination and radiographic evaluation required to determine all of the abnormalities that exist in these complex knee joint injuries are detailed in Chapter 21, Posterior Cruciate Ligament: Diagnosis, Operative Techniques, and Clinical Outcomes, and 31, Primary, Double, and Triple Varus Knee Syndromes: Diagnosis, Osteotomy Techniques, and Clinical Outcomes.
The gait abnormality described in this chapter is easily identifiable in the clinic if the examiner devotes a small amount of time to observation during the initial patient presentation. An abnormal knee hyperextension gait pattern involves increased extension (>0°) in the sagittal plane and, frequently, associated varus malalignment in the coronal plane (varus recurvatum). The varus recurvatum position of the knee will be markedly worse if there is associated osseous tibiofemoral varus malalignment. The triple varus knee, described in detail in Chapter 31, Primary, Double, and Triple Varus Knee Syndromes: Diagnosis, Osteotomy Techniques, and Clinical Outcomes, refers to varus alignment caused by three factors: tibiofemoral varus osseous malalignment, increased lateral tibiofemoral compartment separation due to marked insufficiency of the FCL and PMTL, and varus recurvatum in extension. An abnormal increase in hyperextension usually indicates damage to not only the posterolateral structures but the ACL as well.
Critical Points INTRODUCTION AND DIAGNOSIS
Subjective complaints of knee instability of either partial or full giving-way during routine daily activities often accompany the knee hyperextension gait abnormality. Pain is frequently located in the medial tibiofemoral compartment, which is caused by increased compressive forces owing to the varus malalignment. Pain in the posterolateral tissues also occurs from increased soft tissue tensile forces. In addition to the pain and instability caused by this gait pattern, there is an increased risk of failure of posterolateral reconstructions if the gait abnormality is not corrected before surgery. This is due to the excessively high tensile forces from high knee extension and adduction moments that are expected to be resumed during weight-bearing activities after surgery.16 In addition, patients with associated ACL or PCL deficiency may have an increased risk of failure of cruciate ligament reconstructions if the hyperextension pattern is not corrected before surgery.14,15 Therefore, gait retraining and avoidance of the gait hyperextension pattern are paramount for both resolution of patient symptoms and reduction of the risk of failure of soft tissue ligament reconstructive procedures.
Many investigators have described a quadriceps-avoidance abnormal gait pattern in patients with ACL ruptures.1,2,6,18,20,27 An investigation at the authors’ center18 documented diminished quadriceps activity and enhanced hamstring muscle activity in one half of 32 ACL-deficient varus-angulated knees. Whereas the increased hamstring muscle force could be assumed to be beneficial because it provides a protective mechanism in decreasing anterior tibial translation, the increased muscle force creates high axial compressive forces and, therefore, increases medial and lateral joint compartment (calculated) loads. These loads could be deleterious to the joint over the long term, especially in knees with associated varus osseous malalignment. The abnormal gait characteristics of the ACL-deficient knee are discussed in detail in Chapter 6, Human Movements and ACL Function: ACL-Deficiency and Gait Mechanics.
A hyperextension gait abnormality pattern is also found in patients who have suffered a stroke or traumatic brain injury, cerebral palsy, and poliomyelitis.10 In these instances, the disorder may occur owing to many factors including quadriceps weakness, ankle plantar flexion spasticity, heel cord contracture, and gastrocnemius-soleus weakness. The concern is that the abnormal knee hyperextension may cause stretching of the posterior ligamentous and capsular structures from the increased external extensor torque that is placed across the knee during stance. It is not the purpose of this chapter to discuss the treatment of this problem in patients with neurologic pathology. Rather, this chapter focuses on the treatment of this gait disorder in patients with chronic insufficiency of the posterolateral structures, with or without cruciate ligament ruptures or varus malalignment.
ABNORMAL KNEE HYPEREXTENSION PATTERNS
The normal pattern of knee motion that occurs during the gait cycle is shown in Figure 34-2. A detailed description of normal human gait mechanics is beyond the scope of this chapter and has been presented by many authors.3,4,21,24,25 The loss of the normal knee flexion and extension patterns throughout the stance phase noted in patients with hyperextension gait abnormalities has important functional implications. During the loading response, normal amounts of knee flexion are required for the knee joint to absorb shock. A limb that is instead hyperextended transfers body weight directly from the femur to the tibia, resulting in abnormally high compressive forces. The usual muscle energy absorption and cushioning effect a flexed knee provides is lost.22,23 The thrusting hyperextension motion at the knee is associated with an abnormally high adduction moment, which tends to increase medial tibiofemoral compartment compressive forces and lateral distraction forces. The increased compressive forces manifest as pain in the medial tibiofemoral compartment and posterolateral soft tissues.
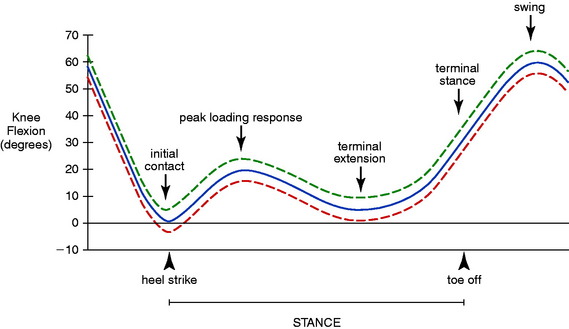
FIGURE 34-2 Knee motion (in degrees) during a normal gait cycle is shown. Phases of stance gait are indicated.
(From Noyes, F. R.; Dunworth, L. A.; Andriacchi, T. P.; et al.: Knee hyperextension gait abnormalities in unstable knees. Recognition and preoperative gait retraining. Am J Sports Med 24:35–45, 1996.).
Critical Points ABNORMAL KNEE HYPEREXTENSION PATTERNS
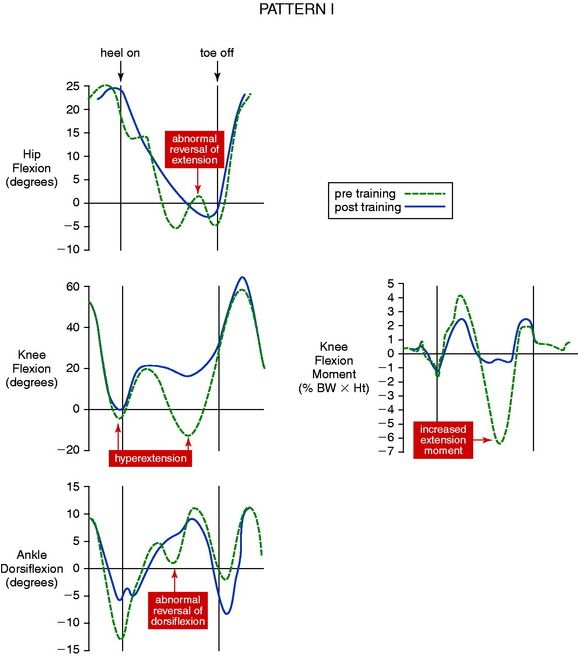
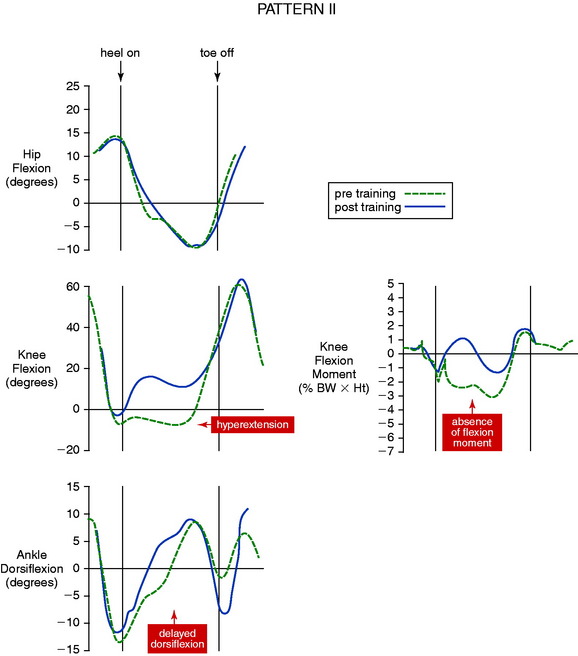
The authors have reported two distinct knee hyperextension gait patterns. In pattern I, the abnormal hyperextension occurs during two periods of the stance phase, heel-strike and terminal extension (Fig. 34-3), with knee flexion noted during the loading response. Exceedingly high knee extension moments are present, along with an abnormal reversal of hip extension and ankle dorsiflexion. Pattern II is characterized by a prolonged knee hyperextension pattern from heel-strike throughout midstance (Fig. 34-4). In these patients, the knee flexion moment is markedly below normal, with its effects incurred primarily at the knee with only a slight delay in ankle dorsiflexion.
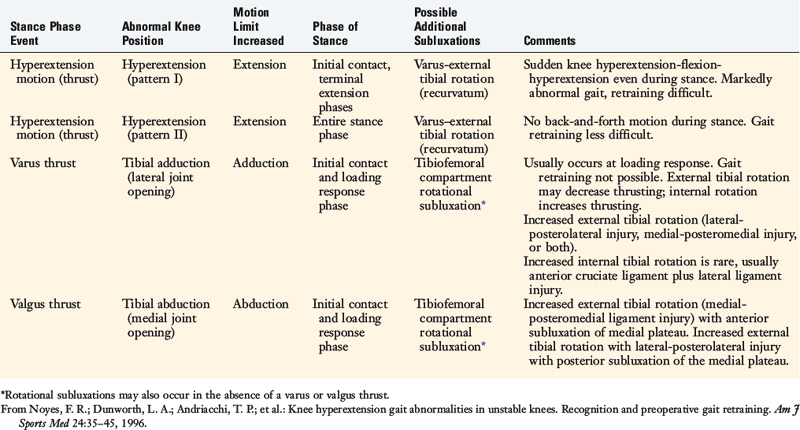
The authors’ clinical observations17 on the various types of abnormal knee motions and thrusts in the sagittal, coronal, and transverse rotational planes that occur during the stance phase of gait are summarized in Table 34-1. Any abnormality in tibiofemoral alignment (varus-valgus osseous malalignment or anterior-posterior tibial slope) may affect knee-thrusting motions in the sagittal or coronal plane. The most common of these is a varus-thrusting gait abnormality, caused by a varus tibiofemoral osseous malalignment. The thrusting motion occurs with the knee near full extension immediately after heel-strike, during the loading response. There may be an associated external or internal rotational subluxation with the varus thrust, depending on the presence of associated deficiency to the posterolateral structures. A less common abnormality, a valgus-thrusting gait, is usually associated with valgus lower limb malalignment. This disorder is typically accompanied by external rotation of the tibia. Knees with these osseous malalignments and associated knee ligament deficiencies require surgical correction of the malalignment by osteotomy prior to ligament reconstructive procedures.
GAIT-RETRAINING PROGRAM FOR ABNORMAL KNEE HYPEREXTENSION
A gait-retraining program has been successfully used at the authors’ center17 for knee hyperextension abnormalities since the mid-1980s. The program requires two to four initial clinical sessions (held preferably every other week) with an experienced physical therapist to instruct the patient on the abnormal gait mechanics that occur and the adaptations required to restore a normal gait pattern (Table 34-2). The patient is instructed to practice at home for at least 2 to 4 hours daily. In addition, the patient undergoes muscle strengthening and neuromuscular coordination training as part of the comprehensive rehabilitation process. In order to have a successful outcome, the patient must be compliant with the time commitment and constant motivation required of this program. A family member is also taught the same instructions so that she or he can observe and assist with the patient’s retraining at home. It is also helpful to video the patient’s abnormal and corrected gait to aid the educational process.
TABLE 34-2 Gait-Retraining Program for Abnormal Knee Stance Hyperextension
| Anatomic Part | Retraining Program |
|---|---|
| Trunk–upper body |
From Noyes, F. R.; Dunworth, L. A.; Andriacchi, T. P.; et al.: Knee hyperextension gait abnormalities in unstable knees. Recognition and preoperative gait retraining. Am J Sports Med 24:35–45, 1996.
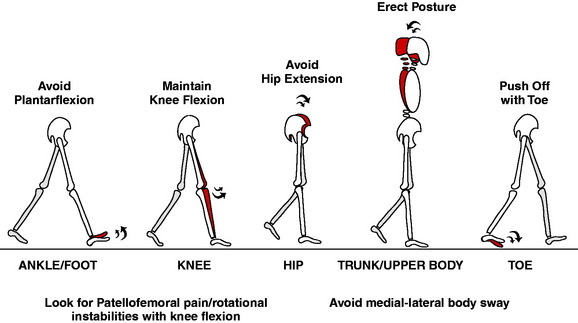
The initial focus of the retraining process is placed on the hyperextension of the knee in order for the patient to understand that this is the primary abnormality that requires modification (Fig. 34-5). The patient is instructed to maintain 5° of flexion with every step. This requires walking in a very slow and deliberate manner. A visual aid to provide to the patient is the mental image of a woman walking in high heels, which produces 5° to 8° of knee flexion. In addition, a 1- to 2-inch elevated heel may be used to help maintain flexion throughout stance phase. The clinician should be aware that problems might occur during gait retraining when the patient practices the flexed knee stance. While the flexed knee gait is advantageous in contributing to quadriceps strengthening, it may aggravate preexisting patellofemoral pain, which must be treated promptly.
The third step analyzes the hip and body trunk position (see Table 34–2). The fourth and final step of the retraining program determines whether an abnormal lower limb alignment (varus or valgus thrust) or an external or internal rotational knee subluxation occurs during stance. This is important because a primary cause of a patient’s abnormal knee hyperextension may be instability of the knee with flexion, so that coronal plane or rotational transverse plane subluxations occur. In these patients, a functional knee brace and additional gait retraining may be required.
Critical Points GAIT-RETRAINING PROGRAM FOR ABNORMAL KNEE HYPEREXTENSION
Quadriceps control is critical for normal gait and represents the muscle group that demands the most attention. Common exercises shown to be effective in helping with quadriceps reeducation include the straight leg plus raise (Fig. 34-6), performed with the patient in the seated position. The quadriceps is contracted, the leg is lifted approximately 6 inches off the table or chair, held in the lifted position for 15 seconds, and then lowered and relaxed for 45 seconds. This 1-minute cycle is maintained and progressed in ratios (1:3, 1:2, and eventually, 1:1), and then progressed from 5 to 10 repetitions, with additional ankle weight added to increase the difficulty of the exercise.
Active isometric hip adduction during the wall-sit by compressing a ball between the knees may assist vastus medialis obliquus recruitment. In addition to obtaining adequate quadriceps control, it is important to improve hip abduction control. A heavy elastic exercise band may be placed proximal to the knee (avoiding patellar pressure) and “clamshells” are performed in either the long-sitting (hook) (Fig. 34-7A and B) or the side-lying (see Fig. 34-7C and D) position. Three to five sets of 10 repetitions are performed. Adjustments to either knee flexion or hip flexion angles can make the exercise easier or more difficult depending on what is necessary to challenge the gluteal musculature.
In order to create a functional gait-retraining program, a blending of the individual exercise programs must progress to include specific gait activities. Patients must overcome a variety of contributing factors including apprehension, muscle weakness, lack of range of motion, compensation, and pain. These factors must be resolved in order for the patient to restore a normal gait cycle. Each of the following factors contributes to a symmetrical gait pattern: adequate push-off, midstance quadriceps control, hip and knee flexion, and maintenance of an upright posture. Two common gait activities can be used quite successfully to assist both in the early time period after injury or surgery and in later time periods. Initially, an activity known as cup-walking is used to encourage the patient to break down the actual gait cycle into more manageable tasks. Cups are set up in two staggered rows with symmetrical stride lengths (Fig. 34-8). The patient is asked to walk or march over the cups, emphasizing each of the earlier four mentioned tasks. This activity allows the clinician to observe the gait cycle to determine where emphasis needs to be placed. Common compensatory mechanisms that patients exhibit include circumduction of the lower extremity, inadequate push-off, midstance hyperextension, lack of coordinated hip and knee flexion, positive Trendelenburg sign, and forward-flexed trunk. The clinician must be able to identify the deficiency in order to teach the patient and her or his support system how to observe the deficiency and to perform the corrective strategy. The normal automatic nature of gait now becomes a “thinking” activity for the patient. The patient is asked to exaggerate the gait cycle by stepping over the cups. This methodical approach allows the patient to apply a part of the gait cycle to the entire, normal gait pattern. Gait-retraining activities such as this must be repeated thousands of cycles over time in order to create a “new default” gait pattern.
As time progresses from the injury or surgery, another gait activity may be used that requires the patient to wear a heavy elastic band around the distal thighs (∼2 finger widths above the patella) and then produce a marching pattern to provide a resisted-gait cycle. With a central line on the floor, the patient, while marching, must maintain right foot-strike on the right side of the line and left foot-strike on the left side of the line (Fig. 34-9). This movement into swing ensures that adequate hip flexion and hip abduction musculature is used during the gait cycle. In addition, the stance limb requires adequate push-off of the gastrocnemius as well as a voluntary quadriceps contraction to prevent a hyperextension episode. This resisted-gait activity can be completed in forward, backward, and lateral directions. Each direction allows the clinician to emphasize what muscle groups are used to allow for adequate voluntary muscle control. Again, these activities require voluntary thought processes to focus on recruiting the quadriceps to avoid the hyperextension mechanism from occurring.
CLINICAL INVESTIGATION
Methods and Materials
The authors’ gait-retraining program17 was studied in 5 patients with symptomatic knee hyperextension and deficiency of the posterolateral structures. Computerized gait analysis testing was conducted before and after the retraining program using a two-camera video-based optoelectronic digitizer for measuring motion and a multicomponent force plate for measuring ground reaction force. The force plate was camouflaged under a 10-m walkway. Patients were asked to walk at three speeds (normal, fast, slow), and measurements were obtained over these ranges to enable comparison of similar walking speeds. Data from complete cycles of stance and swing phase were obtained.
Kinematic data in the sagittal plane and kinetic data in the sagittal, coronal, and transverse planes of the hip, knee, and ankle were evaluated. Peak values during the stance phase were recorded for each patient. Using a previously described mathematical model,3,24 joint reaction loads, lateral soft tissue forces, and muscle forces were calculated. The patient data were compared with those obtained from a control group of 11 subjects matched for age and walking speed. All moments, which were expressed as external moments, were normalized to body weight and height.
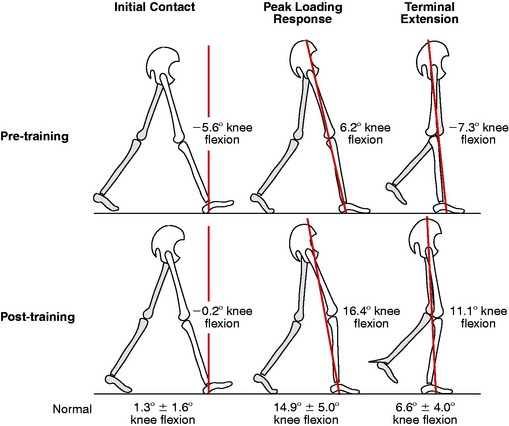
Analysis of Gait Mechanics before Retraining
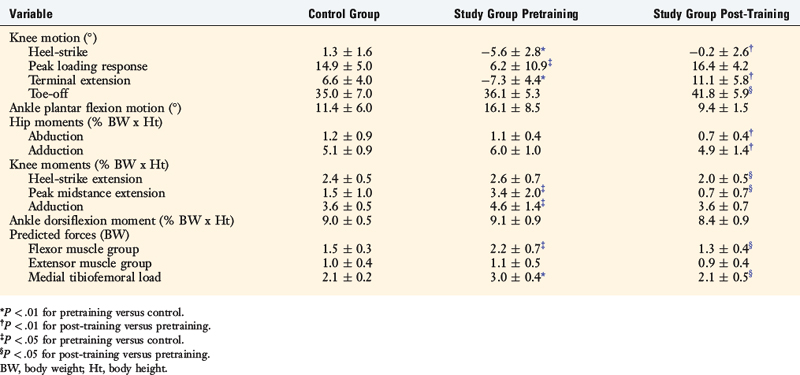
Statistically significant differences were found between the pretrained patients and the control subjects in the mean values for knee hyperextension during heel-strike and terminal extension (Table 34-3 and Fig. 34-10), with the patients demonstrating a range of 5.4° to 18.4° less flexion (P < .05). The patients had a significantly higher mean knee midstance extension moment (127%; P < .01), knee adduction moment (28%; P < .05) and calculated medial tibiofemoral compartment loads (43%; P < .001) than the controls. The two knee hyperextension patterns previously discussed were identified: 3 patients demonstrated pattern I and 2 patients, pattern II.
Critical Points CLINICAL INVESTIGATION
Patient data compared with control group of 11 subjects matched for age and walking speed.
Significant differences between pretrained patients and controls. Patients had
Effect of Retraining on Patient Symptoms
The patient symptoms before and after gait retraining were evaluated with the symptom rating scale of the Cincinnati Knee Rating System (see Chapter 44, The Cincinnati Knee Rating System). A statistically significant improvement occurred in the pain scale (0–10 points) from a mean of 1.6 ± 0.9 points before training to 4.8 ± 2.3 points after training (P < .05) and in the partial giving-way scale from a mean of 2.4 ± 0.9 points before training to 5.2 ± 2.3 points after training (P < .05). Four of the 5 patients improved from experiencing moderate pain and instability with daily activities before retraining to walking several hours per day without appreciable symptoms. Because of this improvement, 2 patients did not require ligament reconstructive surgery after retraining.
A 32-year-old physical therapist with chronic ACL deficiency of the left knee had given up strenuous athletics in order to avoid ACL reconstruction. She had no pain, swelling, or giving-way for several years. The patient participated in a light recreational volleyball game and experienced a partial giving-way episode. She presented with increasing medial joint line pain and a feeling of knee instability and believed she required ACL reconstruction. The patient had a bilateral standing physiologic varus recurvatum and walked with marked varus recurvatum thrust to the left lower extremity (Fig. 34-11). She was unaware that her gait pattern had changed. and the obvious hyperextension thrust became readily apparent to her after it was revealed under examination. The patient underwent the gait-retraining program and adapted to a normal gait pattern. Within 3 weeks, her medial joint pain and instability symptoms resolved. She returned to her preinjury compensated status and had no further symptoms to warrant ACL reconstruction. Because she was a physical therapist and could understand the retraining program, she had a fast response.
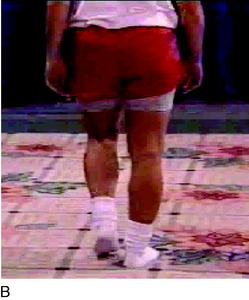
A 38-year-old woman presented 1 year after a motor vehicle accident with a diagnosis of a PCL rupture. She experienced frequent instability and shifting episodes and severe medial joint line pain. Physical examination revealed marked quadriceps atrophy, 12 mm of increased posterior tibial translation, 10 mm of increased lateral joint opening, 15° of increased external tibial rotation, and a varus alignment. On standing alignment, the patient showed a varus position, but did not demonstrate a varus recurvatum. However, on walking with increased forces, a severe varus recurvatum occurred with every step (Fig. 34-12). The patient first underwent gait retraining to correct the varus thrust and rehabilitation for quadriceps muscle strengthening for 3 months. Then, an opening wedge osteotomy was performed to correct the varus osseous malalignment, followed 6 months later with a PCL and posterolateral reconstruction.
A 24-year-old woman presented 2 years after a motor vehicle accident with a severe gait abnormality and limp on the left lower extremity (Fig. 34-13). She had pain throughout the knee joint. Physical examination revealed complete deficiency of the PCL and posterolateral structures. The patient had seen three other orthopaedic surgeons who were all reluctant to perform surgery owing to the severe gait abnormality and lower extremity muscle atrophy. She required 6 months of gait retraining. Although she was never fully able to control her knee stability, she did experience marked improvement and could consciously control the severe varus recurvatum.
1 Andriacchi T.P. Dynamics of pathological motion: applied to the anterior cruciate–deficient knee. J Biomech. 1990;23(suppl 1):99-105.
2 Andriacchi T.P., Birac D. Functional testing in the anterior cruciate ligament–deficient knee. Clin Orthop Relat Res. 1993;288:40-47.
3 Andriacchi T.P., Hampton S.J., Schultz A.B., Galante J.O. Three-dimensional coordinate data processing in human motion analysis. J Biomech Eng. 1979;101:279-283.
4 Andriacchi T.P., Ogle J.A., Galante J.O. Walking speeds as a basis for normal and abnormal gait measurements. J Biomech. 1977;10:261-268.
5 Baker C.L.Jr., Norwood L.A., Hughston J.C. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1983;65:614-618.
6 Berchuck M., Andriacchi T.P., Bach B.R., Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72:871-877.
7 DeLee J.C., Riley M.B., Rockwood C.A.Jr. Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983;11:199-207.
8 Gollehon D.L., Torzilli P.A., Warren R.F. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233-242.
9 Grood E.S., Noyes F.R., Butler D.L., Suntay W.J. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63:1257-1269.
10 Kerrigan D.C., Deming L.C., Holden M.K. Knee recurvatum in gait: a study of associated knee biomechanics. Arch Phys Med Rehabil. 1996;77:645-650.
11 LaPrade R.F., Terry G.C. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433-438.
12 Nielsen S., Ovesen J., Rasmussen O. The posterior cruciate ligament and rotatory knee instability. An experimental study. Arch Orthop Trauma Surg. 1985;104:53-56.
13 Nielsen S., Rasmussen O., Ovesen J., Andersen K. Rotatory instability of cadaver knees after transection of collateral ligaments and capsule. Arch Orthop Trauma Surg. 1984;103:165-169.
14 Noyes F.R., Barber-Westin S.D. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33:646-654.
15 Noyes F.R., Barber-Westin S.D. Revision anterior cruciate surgery with use of bone–patellar tendon–bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131-1143.
16 Noyes F.R., Barber-Westin S.D., Albright J.C. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med. 2006;34:1419-1430.
17 Noyes F.R., Dunworth L.A., Andriacchi T.P., et al. Knee hyperextension gait abnormalities in unstable knees. Recognition and preoperative gait retraining. Am J Sports Med. 1996;24:35-45.
18 Noyes F.R., Schipplein O.D., Andriacchi T.P., et al. The anterior cruciate ligament–deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20:707-716.
19 Pasque C., Noyes F.R., Gibbons M., et al. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br. 2003;85:292-298.
20 Patel R.R., Hurwitz D.E., Bush-Joseph C.A., et al. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68-74.
21 Perry J., editor. Gait Analysis: Normal and Pathological Function. Thorofare, NJ: Slack; 1992:49-281.
22 Perry J., Antonelli D., Ford W. Analysis of knee joint forces during flexed-knee stance. J Bone Joint Surg Am. 1975;57:961-967.
23 Saunders J., Inman V., Eberhart H. The major determinants in normal and pathological gait. J Bone Joint Surg Am. 1953;35:543-558.
24 Schipplein O.D., Andriacchi T.P. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113-119.
25 Simon S.R. Gait—normal and abnormal. In: Insall J., Scott W.N., editors. Surgery of the Knee. Philadelphia: Churchill Livingstone; 2001:232-254.
26 Veltri D.M., Deng X.H., Torzilli P.A., et al. The role of the cruciate and posterolateral ligaments in stability of the knee. A biomechanical study. Am J Sports Med. 1995;23:436-443.
27 Wexler G., Hurwitz D.E., Bush-Joseph C.A., et al. Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Relat Res. 1998;348:166-175.