Correction of Clitoral Phimosis
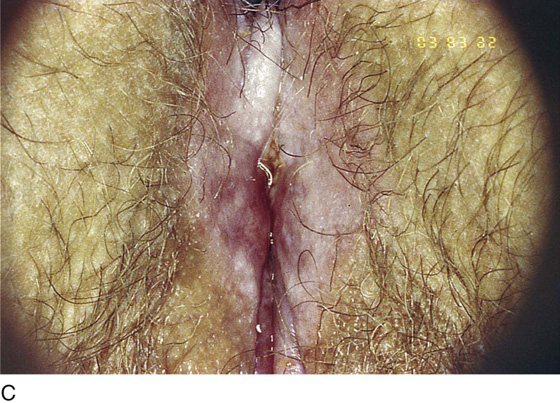
Severe clitoral phimosis is an end result of long-standing and suboptimally managed lichen sclerosus (Fig. 74–1A, B). In this circumstance, the skin of the frenulum and the clitoral hood fuse as a result of inflammation and subsequent scar formation (Fig. 74–1C). This creates persistent, severe itching, as well as outright pain. Because drainage is poor, smegma builds up, which may lead to abscess formation. The goal of surgery is to remove the scarred tissue and preserve the clitoris. Removal of the clitoris is unnecessary and should not be done.
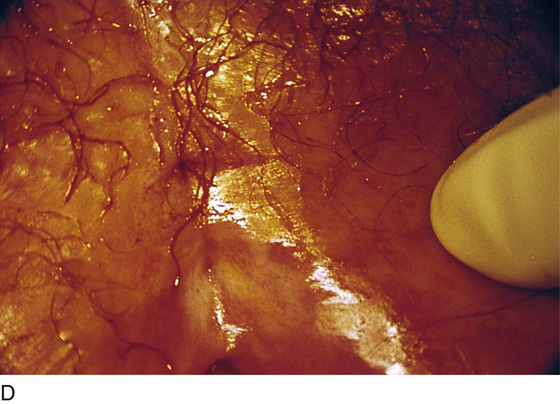
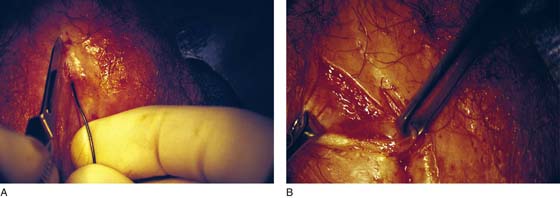
Examination with an operating microscope (colposcope) will reveal a tiny opening in the sheath or complete incarceration of the glans (Fig. 74–1D). Identifying an opening gives the surgeon the advantage of being able to insert a probe in close proximity to the clitoris (Fig. 74–2). The entire operation should be performed with use of the microscope. With a 27-gauge needle, a 1 : 100 vasopressin solution is injected on either side of the clitoris through the mass of tissue that was once the clitoral hood (Fig. 74–3). A knife incision is made to one side of the palpated clitoris. The incision should be made on the side with the least amount of scar tissue (Fig. 74–4A).
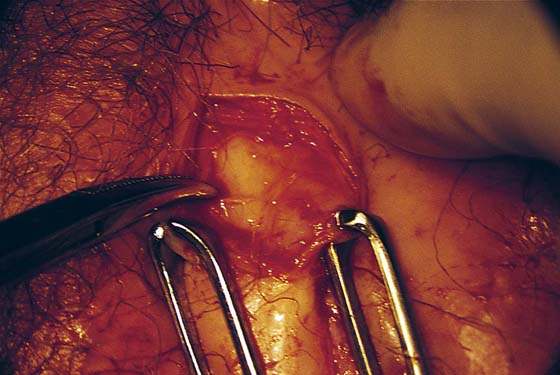
Dissection proceeds from lateral to medial (Fig. 74–4B). The skin edges are retracted with Allis clamps. Stevens tenotomy scissors are ideal for sharply dissecting and separating the clitoral body from the scar tissue (Fig. 74–5). The scar is dissected anteriorly and posteriorly to completely mobilize the clitoris (Fig. 74–6). Next, the sheath and the remains of the frenulum are cut away from the glans clitoris (Fig. 74–7). The junction of the frenulum to the glans is highly vascular and must be clamped, cut, and suture-ligated with 4-0 or 5-0 Vicryl (Fig. 74–8). When this is completed, the entire hood complex is removed. Bleeding vessels are suture-ligated with 5-0 Vicryl. When all scar tissue has been excised, the clitoris is placed in the hemostatic bed beneath the subcutaneous tissue, which then is closed with 4-0 Vicryl (Fig. 74–9). The skin is closed with interrupted 3-0 or 4-0 Vicryl sutures. The wound is cleansed with sterile water, dried, and covered with silver sulfadiazine (Silvadene) cream (Fig. 74–10).
FIGURE 74–1 A. Severe lichen sclerosus et atrophicus (LSA) creates intense pruritus. The patient’s scratching results in excoriation of the skin. The pallor of the vulvar skin is characteristic of LSA. Note the labial fusion, clitoral hood fusion, and puckering of the skin of the vulva. In this early case, the clitoris is relatively free. B. This more advanced case of LSA illustrates clitoral fusion, labial fusion, and introital stenosis. C. The clitoral hood and the frenulum are totally fused. The clitoris is tightly locked into its hood, which is adherent to the glans. The patient experienced painful swelling of the clitoris. D. This colposcopic view of a phimotic clitoris reveals a small opening. The location of the opening corresponds to the point where the frenulum joins the clitoral hood.
FIGURE 74–2 A lacrimal probe is engaged into the opening (see Fig. 71–1D) and is used to break up and probe adhesions between the glans clitoris and the inner aspect of the hood. It also serves as a useful orientation marker.
FIGURE 74–3 Surgery for clitoral phimosis is best performed by utilizing the operating microscope. A 27-gauge needle is inserted via the opening seen in Figure 71–1D. A 1 : 100 vasopressin solution is injected into the hood. Additionally, the vasopressin is injected on either side of the palpated clitoral body.
FIGURE 74–4 A. A scalpel cut is made through the skin to the level of Colles’ fascia. This cut is located parallel but lateral to the body of the clitoris. Care must be taken not to go deeper than Colles’ fascia. The clitoral corpora cavernosa (crus) are located beneath Colles’ fascia in this view. B. The margins of the wound are placed on traction with Allis clamps. The dissection proceeds from lateral to medial with the use of mosquito clamps and Stevens scissors.
FIGURE 74–5 The body of the clitoris is located. The entire length of the clitoris is dissected free from the surrounding scarred connective tissue and clitoral hood.
FIGURE 74–6 The dissection proceeds from the root of the clitoral body to the terminal glans. All scar tissue is removed.
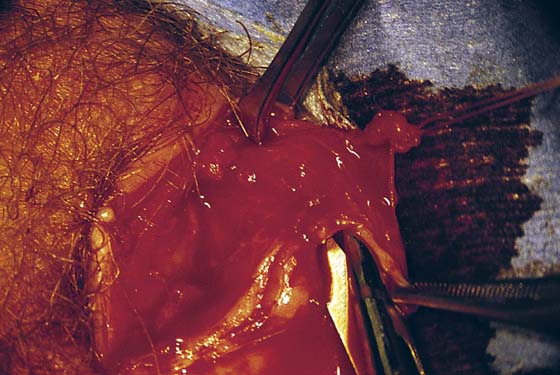
FIGURE 74–7 The clitoral frenula are located and dissected away from the glans. These are cut with Stevens scissors. In this photo, the edge of the left frenulum is held in the forceps. The tip of the Stevens scissors is dissecting a space between the frenulum and the glans. The Allis clamp is holding the tissue just superior to the clitoral body.
FIGURE 74–8 The cut edges of the frenulum are sutured with 5-0 Vicryl. The unencumbered glans clitoris is clearly visible.
FIGURE 74–9 All scarred tissue has been removed. The clitoris is located between normal subcutaneous tissue and Colles’ fascia. No part of the clitoris has been excised or injured. The subcutaneous layer is closed with 4-0 Vicryl (interrupted) sutures. The skin margins are approximated without tension with 3-0 or 4-0 Vicryl sutures.
FIGURE 74–10 The wound site is irrigated with normal saline or sterile water and then is covered with Silvadene cream. The cream is applied 3 times per day and at bedtime.