Chapter 9 Coronary MRA
Introduction
Coronary MRA is technically demanding since the coronary arteries are small, tortuous vessels embedded in epicardial fat that move with cardiac and respiratory motion.
Coronary MRA techniques
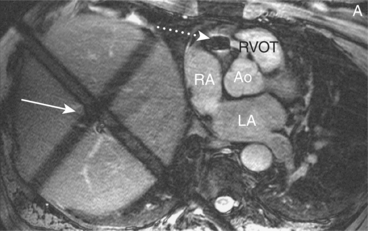
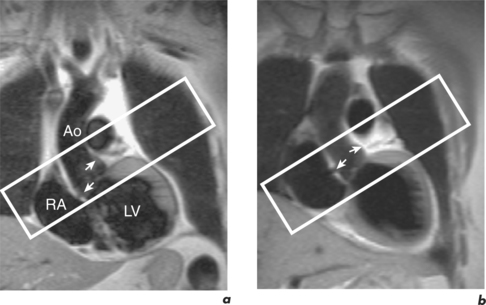
Free breathing combined with 3D imaging provides good signal-to-noise ratio (SNR) and anatomical coverage. GE sequences image blood within the coronaries, and SE sequences image the vessel wall. Subjects breathe normally throughout the scan and respiratory artefact is minimized by the prior addition of respiratory navigators. These provide a way of monitoring respiratory motion during data collection and correcting that data for the motion. Methods of motion assessment differ, and one commonly used is detection of the superior–inferior movement of the dome of the right hemidiaphragm (Figure 9.1). Following placement and navigator initiation, the user automatically accepts data when the diaphragm–lung interface falls within a pre-defined window and rejects data that fall outside this narrow limit. The acceptance window is positioned at the end expiratory pause period of the respiratory cycle and extends 2–3 mm either side of a patient-specific diaphragm–lung interface value.
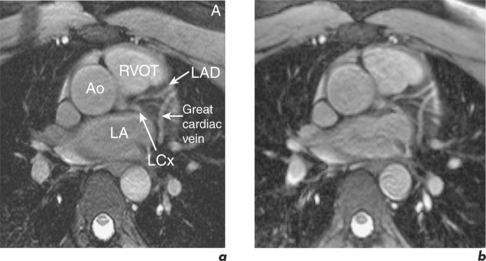
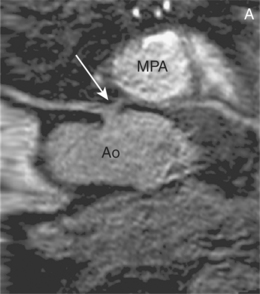
Free breathing sequences acquire data over several minutes and provide higher resolution than breath-hold techniques. Breath-hold 3D GE coronary MRA requires subjects to suspend their respiration for 20–25 s depending on their heart rate. Since navigators are avoided, breath-holding requires less expertise and circumvents problems arising from suboptimal respiratory patterns. The resolution and coverage sacrificed with the breath-hold option becomes relevant at the limits of coronary MRA indications, such as evaluation of coronary artery stenoses, and is not of significance for delineation of proximal coronary artery origin and early course. With free breathing SSFP GE coronary MRA a typical spatial resolution is 1.1 ×0.7 ×1.5 mm3 with 30 to 48 mm through-plane coverage, as compared to 1.3 ×1.1 ×1.6 mm3 with 16 to 19.2 mm through-plane coverage using the breath-hold sequence. Breath-holding permits several volumes of interest to be imaged in the same time it takes to perform one free breathing scan. Patients do vary in their response to the two methods with consequent compromise to image quality and diagnostic accuracy, and both may need to be attempted (Figure 9.2). Maximal and optimal resolution with either technique is not equivalent. Maximizing resolution will assist accuracy but will reduce SNR and lead to grainy images, while optimal resolution may be a little lower but produce better quality scans. Post-processing curved MPR is an excellent way of presenting findings in coronary MRA reports (Figure 9.3).
Coronary MRA protocol
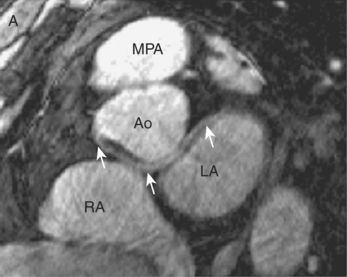
Anomalous coronary arteries
Anomalous coronary arteries are rare and usually asymptomatic. Prevalence ranges from 1% in patients with otherwise normal cardiac anatomy to 36% in individuals with ACHD such as TOF. Their importance lies in the association of specific variants with myocardial ischaemia or MI, syncope and sudden cardiac death, particularly amongst young adults. This premature morbidity and mortality typically occurs during strenuous physical exercise with coronary arteries that traverse between the aorta and PA (Figure 9.3). Three postulated mechanisms are: mechanical embarrassment from aortic and PA dilatation at a time of increased coronary flow demand, kinking of an ostial or proximal segment due to a sharp turn or bend at the origin, and a congenitally slit-like ostium which is inadequate to meet extra requirements.
Variations of anomalies include:
Referrals for coronary MRA are often made following X-ray coronary angiography where there is failure to engage one of the coronary ostia, or when an anomaly is angiographically demonstrated and delineation of the proximal course is needed. Coronary MRA is important in patients with ACHD and as part of the work-up in young patients with unexplained syncope or chest pain. These latter groups invariably undergo more comprehensive CMR evaluation than coronary MRA alone. A potential preparticipation screening role in competitive athletes has also been suggested, again with a CMR protocol encompassing more than isolated exclusion of anomalous coronary arteries.
Coronary artery aneurysms and Kawasaki disease
Coronary artery aneurysms are rare. Causes are congenital or acquired secondary to atherosclerosis, coronary interventions and connective tissue or inflammatory disorders such as Kawasaki disease (Figure 9.6). Kawasaki disease is a vasculitis affecting children. Cardiovascular complications are the leading cause of mortality and morbidity and include myocarditis and valvular regurgitation. Coronary artery aneurysms can lead to MI, sudden death or IHD and sites for aneurysm formation in reducing order of frequency are: