Chapter 21
Coronary Artery Bypass Surgery
1. What are the indications for coronary artery bypass grafting (CABG)?
2. How does CABG compare with medical management for CAD?
3. How does CABG compare with stents?
4. What about with drug-eluting stents (DES)?
Drug-eluting stents have reduced the problem of restenosis, but data directly comparing DES with CABG is limited and still relatively short-term. In a registry study from the New York state cardiovascular database, CABG resulted in improved survival at 3 years compared with DES for patients with double- and triple-vessel disease. ARTS II randomized patients to DES or CABG, and showed that the primary composite outcomes at one year were similar. The international SYNTAX trial, involving 85 centers and 1800 patients with multivessel or left main CAD, recently published 3-year follow-up data in 2011. This showed worse outcomes in the PCI group as compared to the CABG group at 3 years, with increased composite major adverse cardiac and cerebrovascular events (MACCE: death, stroke, MI, or repeat revascularization). Although there was no significant difference in all-cause mortality and stroke at 3 years, MI and repeat revascularization were both increased in the PCI group. The study concluded that patients with more complex disease (three-vessel CAD with intermediate-high SYNTAX scores and LM artery CAD with high SYNTAX scores) have an increased risk of MACCE with PCI, and CABG is the preferred treatment option.
6. Which patients benefit most from CABG?
7. What is the cardiopulmonary bypass (CPB) pump, and how is it used?
8. Why is heparin required for CPB?
9. How is the heart stopped while on CPB?
The heart is stopped by placing a completely occluding cross-clamp across the ascending aorta, below the aortic cannula, eliminating arterial blood flow to the coronary arteries. Cardioplegia solution is then used to induce arrest of the heart, and can be given antegrade and/or retrograde. Components of cardioplegia solution are varied in different institutions but include potassium to achieve diastolic arrest. Cardioplegia solution administered into the aortic root, via a small cannula below the cross-clamp, is delivered in an antegrade fashion to the myocardium via the coronary ostia. Retrograde cardioplegia is also used frequently, by infusing cardioplegia solution into the coronary sinus with backward filling of the cardiac veins to reach the myocardium, and is especially important in situations where antegrade may not be as effective, such as with severe CAD and aortic valve insufficiency. Most commonly, cold cardioplegia at 4° C is administered intermittently in 15- to 20-minute intervals. Blood can be mixed to the crystalloid component of cardioplegia in a 4:1 mix to provide oxygenated blood to the myocardium and to buffer the pH of the tissue (Fig. 21-1).
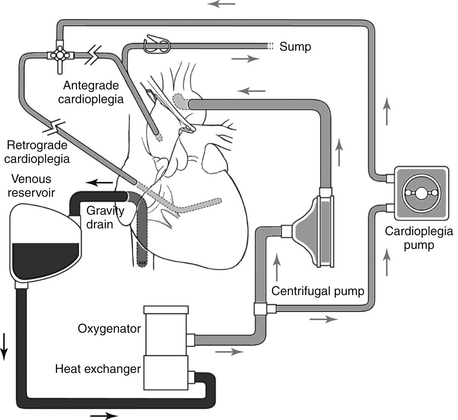
Figure 21-1 Schematic of total cardiopulmonary bypass circuit. All returning venous blood is siphoned into a venous reservoir and is oxygenated and temperature regulated before being pumped back through a centrifugal pump into arterial circulation. The common site for inflow into the patient is the ascending aorta, but alternate sites include the femoral arteries or the right axillary artery in special circumstances (see later). A parallel circuit derives oxygenated blood that is mixed with cold (4° C) cardioplegic solution in the ratio of 4:1 and administered in an antegrade or retrograde fashion to accomplish cardiac arrest. Antegrade cardioplegia is administered into the aortic root and retrograde through the coronary sinus. During the administration of retrograde cardioplegia, the efflux of blood from the coronary ostium is siphoned off via the sump drain. The sump drain, a return parallel circuit connected to the venous reservoir (not shown), also helps to keep the heart decompressed during the arrest phase. (From Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL: Sabiston Textbook of Surgery, ed 19, Philadelphia, 2012, Saunders.)
10. How is the myocardium protected during cardiac arrest during bypass surgery?
11. What are the benefits of using the internal mammary artery for bypass?
Use of the internal mammary artery (IMA) was first described by Kolessov in 1967, but its impact on survival wasn’t noted until the mid-1980s. Left IMA (LIMA) anastomosed to the LAD artery has an approximately 90% patency at 10 years and offers an advantage in both survival and freedom from reoperation. The current guidelines for CABG include a class I recommendation for use of the LIMA to bypass the LAD artery when bypass of the LAD artery is indicated (Fig. 21-2).
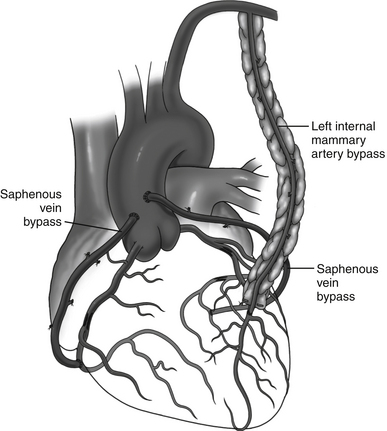
Figure 21-2 Typical configuration for a three-vessel coronary artery bypass. The left internal mammary artery is anastomosed to the left anterior descending artery. Aortocoronary bypasses are created using the reversed saphenous vein to the distal right coronary artery and an obtuse marginal branch of the circumflex coronary artery. The circumflex coronary artery is usually avoided as a target for bypass because it is located well into the atrioventricular groove and difficult to visualize. (From Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL: Sabiston Textbook of Surgery, ed 19, Philadelphia, 2012, Saunders.)
12. What about other arterial conduits?
13. What is the long-term patency of the saphenous vein?
The saphenous vein is readily available and relatively easy to procure, provides multiple graft segments, and is the most common bypass graft used other than the LIMA. The major limitation of the SVG is its long-term patency. Early attrition of up to 15% can occur by 1 year, with 10-year patency traditionally cited at 60%. Early patency has been shown to be improved by use of aspirin postoperatively. SVG can be harvested using a single long leg incision, multiple short incisions with intervening skin islands, or endoscopic techniques. Early patency has largely been found to be equivalent both clinically and angiographically between open and endoscopic techniques.
14. What is off-pump CABG, and what are the differences between on-pump and off-pump CABG?
Off-pump bypass is CABG surgery performed without use of the CPB machine. The heart remains beating throughout the procedure, and stabilizers and coronary occlusion and shunts are used to perform the bypass graft to native coronary artery anastomoses (Fig. 21-3). Because off-pump surgery avoids CPB, it should lessen the side effects of the extracorporeal circulation, such as activation of inflammatory mediators, coagulopathy, and risk of embolic events. Surgeons have debated the merits of off-pump verses on-pump bypass for many years, and the goal of demonstrating differences between the two techniques in hard endpoints, such as mortality, stroke, and renal failure, has been elusive. In fact, the literature largely shows equivalency in these major early outcomes. In some studies, slightly shorter lengths of hospital stay and lower transfusion rates have been noted with off-pump surgery.
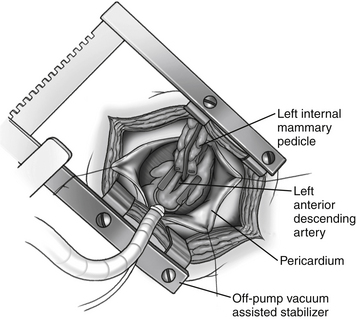
Figure 21-3 Left thoracotomy approach for performing off-pump left internal mammary to left anterior descending bypass. This is commonly used in the minimally invasive direct coronary artery bypass (MIDCAB) approach. Multiarticulating stabilizers are essential for this technique. (From Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL: Sabiston Textbook of Surgery, ed 19, Philadelphia, 2012, Saunders.)
The technique of off-pump revascularization can be particularly useful in selected cases, such as in patients with a heavily calcified aorta (often called a “porcelain aorta”). In experienced centers, patency rates of the bypass grafts performed on-pump versus off-pump should not differ greatly. Most centers use off-pump selectively. In the United States, currently approximately 80% of CABG operations are performed on-pump using CPB, whereas 20% are performed off-pump.
15. What are minimally invasive, robotic, and hybrid CABG procedures, and what are their current roles in coronary revascularization?
16. What complications can occur following CABG?
17. Who is at risk for mediastinitis?
Mediastinitis is a deep surgical-site infection following sternotomy. The infection involves the sternal bone and underlying heart and mediastinum. The organism most commonly recovered is Staphylococcus, but gram-negative organisms can also be found. The incidence of mediastinitis has been reported in the past to be 1% to 4%, but a recent Society of Thoracic Surgeons (STS) database study has shown an incidence less than 1%. The incidence of mediastinitis increases with the presence of diabetes, morbid obesity, COPD, and when bilateral mammary harvesting is performed. Perioperative prophylactic antibiotics, proper skin preparation and clipping, and active control of hyperglycemia in the postoperative setting are important measures believed to decrease the incidence of mediastinitis.
18. What causes strokes during coronary bypass?
19. What is a type II neurologic deficit?
20. How should clopidogrel be managed preoperatively?
21. What factors are important in the follow-up of CABG patients?
22. What is the incidence of recurrent disease requiring redo-CABG?
Bibliography, Suggested Readings, and Websites
1. Collins, P., Webb, C.M., Chong, C.F., et al. Radial artery versus saphenous vein patency (RSVP) randomized trial: five-year angiographic follow-up. Circulation. 2008;117:2859–2864.
2. Goldman, S., Sethi, G.K., Holman, W., et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery. A randomized trial. JAMA. 2011;305:167–174.
3. Goldman, S., Zadin, K., Moritz, T., et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs cooperative study. J Am Coll Cardiol. 2004;44:2149–2156.
4. Hannan, E.L., Wu, C., Walford, G., et al. Drug-eluting stents vs. coronary artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358:331–334.
5. Hillis, L.D., Smith, P.K., Anderson, J.L., et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg. 2012;143:4–34.
6. Kappetein, A.P., Feldman, T.E., Mack, M.J., et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125–2134.
7. Lamy, A., Devereaux, P.J., Prabhakaran, D., et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. (CORONARY investigators). N Engl J Med. 2012;366:1489–1497.
8. McKhann, G.M., Grega, M.A., Borowicz, L.M., Jr., et al. Is there cognitive decline 1 year after CABG? Comparison with surgical and nonsurgical controls. Neurology. 2005;65:991–999.
9. Sellke, F.W., DiMaio, J.M., Caplan, L.R., et al. Comparing on-pump and off-pump coronary artery bypass grafting: numerous studies but few conclusions: a scientific statement from the American Heart Association Council on Cardiovascular Surgery and Anesthesia in collaboration with the Interdisciplinary Working Group on Quality of Care Outcomes Research. Circulation. 2005;111:2858–2864.
10. Shroyer, A.L., Grover, F.L., Hattler, B., et al. Veterans Affairs randomized on/off bypass (ROOBY) study group. On-pump versus off-pump coronary artery bypass surgery. N Eng J Med. 2009;361:1827–1837.
11. Smith, S.C., Jr., Allen, J., Blair, S.N., et al. AHA\ACC Guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Circulation. 2006;113:2363–2372.



